|
Evolution
Since the invention of the ophthalmoscope in 1851 by Hermann von Hemholtz, visualization of the posterior segment of the eye by ophthalmologists has undergone dramatic improvements. Obtaining photographs of the posterior segment of the eye has always been challenging because illumination of the posterior segment is required simultaneously with visualization of the ocular structures by the photographer. The first reliable fundus camera was introduced by Carl Zeiss and J.W. Nordensen in 1926, and this allowed for documentation of ocular fundus structures. This camera provided a 20-degree field of view, but it wasn’t until years later that the Carl Zeiss Co. set a 30-degree field of view as the standard in ocular fundus photography.1 This field of view was adequate for imaging of the optic nerve and the posterior pole, but provided a limited view of the retinal periphery. Throughout the years, several advances have been made to posterior segment imaging. These currently provide the clinician with several options for posterior segment documentation and evaluation.
|
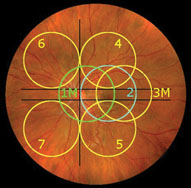
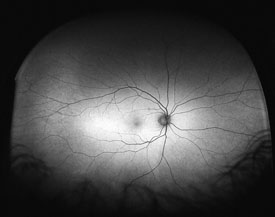
Traditional fundus cameras may provide images of the retinal periphery if the objective lens is directed towards the periphery. The Diabetic Retinopathy Study detailed a method of acquiring images of the retinal periphery in a systematic manner.2 This strategy utilizes traditional lenses to take multiple photographs of the posterior pole, which can then be viewed independently or fused into a montage (See Figure 1). Seven standard fields, when viewed collectively, create an image that covers about 75 degrees field of view. Although the seven standard fields image the mid-peripheral retina very well, they will not image structures in the far periphery. This has been demonstrated specifically in regards to peripheral pathology, such as is present from diabetic retinopathy and sickle cell retinopathy.3,4
The Retcam is a portable wide-angle camera system that offers convenient imaging of the posterior pole. It was made commercially available in 1997. The system consists of a contact lens and offers several different lens attachments, depending on the operator’s goals. The widest field lens provides for 130 degrees field of view. The system is particularly well-suited for imaging pediatric patients because it is portable and can be placed directly on a patient who is supine. This system, however, has difficulty imaging through lens opacities, which are rare in infants. Specifically, this imaging modality has been well-studied in patients with retinopathy of prematurity.5-9
Recently, imaging of the ocular fundus has been possible through the use of scanning laser ophthalmosocopy (SLO). This technology uses laser light and the principles of confocal laser scanning microscopy to yield images with high resolution. The Heidelberg HRA (Heidelberg Engineering) can be used to create wide-field images if used in conjunction with a wide-angle lens, such as the Staurenghi lens system.10 The Staurenghi lens system is a contact lens that is applied prior to imaging and produces a wide-field inverted image of the ocular fundus.
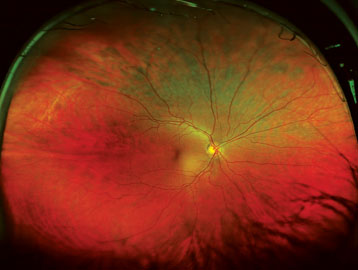
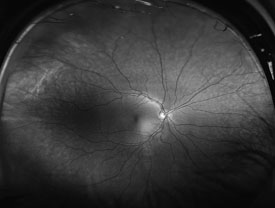
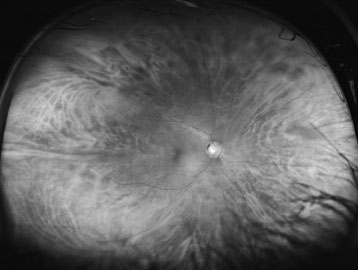
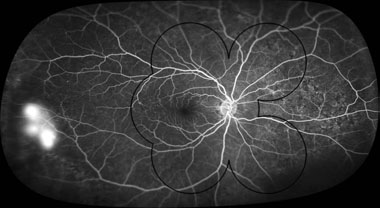
The Optos camera also employs scanning laser ophthalmoscopy technology and is capable of producing wide-field images (See Figure 2). Introduced in 2000, the Optos is the first camera capable of producing 200 internal degrees field of view, which equates to about 82.5 percent of the total retinal surface area.11 The technology utilizes an ellipsoid mirror to obtain images of the retinal periphery without the need for bright illumination lighting or a contact lens, and in some patients, pupillary dilation. The current model uses a red (633 nm) (See Figure 3) and green laser (523 nm) (See Figure 4) to scan the retina and obtain the images. The images created by each of these laser wavelengths may be separated into their individual components.
|
Research into several retinal diseases that affect the anterior retina has been performed using wide-field imaging. The use of wide-field angiography to image the anterior retina of patients with diabetic retinopathy, for example, has been shown to enhance the clinical evaluation (See Figure 7).3 In addition to identifying areas of capillary non-perfusion and neovascularization, the wide-field images of diabetic patients can be instrumental in planning surgical or laser treatment.13 In addition to diabetic retinopathy, retinal vasculitis and uveitis often present with peripheral vascular changes. Fluorescein angiography is able to detect vessel inflammation and incompetence that may be difficult to detect on peripheral retinal examination with an indirect ophthalmoscope. Wide-field fluorescein angiography enhances this evaluation. For example, in the case of sickle cell retinopathy, a recent report demonstrated that wide-field imaging was able to image the peripheral retinal vascular pathology—not possible with traditional seven standard fields.4 Further research into the utility of wide-field imaging in pathologies such as retinal detachment, choroidal dystrophies and even macular degeneration is ongoing.
|
Although these imaging modalities are changing the way that clinicians practice medicine and have become valuable research tools, wide-field imaging currently has several limitations. It is important for a clinician to be aware of these drawbacks in order to appropriately analyze the volume of information that wide-field images provide. The first limitation that is critical to recognize is the inability of wide-field imaging to image the ora serrata 360 degrees with a single image. Specifically, imaging of the anterior retina superiorly and inferiorly is limited with this modality. The current available modalities of retinal imaging, therefore, do not replace the use of indirect ophthalmoscopy with scleral depression to evaluate the anterior retina in all quadrants. Another limitation is the fact that the imaging technique requires training of the photographer in a new modality. For example, unlike in traditional fundus photography, the photographer using the Optos is not provided with an image of the retinal area that will be photographed prior to the capture of the image. Lastly, when using the Optos, the ellipsoid mirror and the spherical nature of the globe result in distortion of the peripheral image and prevent direct measurement of the peripheral retinal structures on the image.
Imaging of the peripheral retina has significantly improved over the past several decades. Wide-field technology has become important clinically with regards to diagnosis, treatment, and monitoring of several diseases. In addition, wide-field imaging has demonstrated significant utility in a research capacity. It is likely that with additional time, the full utility of wide-field imaging will be revealed. REVIEW
Dr. Witmer and Dr. Kiss are in the Department of Ophthalmology, Weill Cornell Medical College. Dr. Kiss serves as a consultant for Optos. Contact him at 1305 York Ave, New York, N.Y. 10128. Phone: (646) 962-2217; e-mail:
szk7001@med.cornell.edu.
1. Ciardella A, Brown D. Wide field imaging. In: Agarwal A, ed. Fundus Fluorescein and Indocyanine Green Angiography: A Textbook and Atlas. New York: Slack Inc., 2007:79-83.
2. Diabetic retinopathy study. Report Number 6. Design, methods, and baseline results. Report Number 7. A modification of the Airlie House classification of diabetic retinopathy. Prepared by the Diabetic Retinopathy. et al.. Invest Ophthalmol Vis Sci 1981;21(1 Pt 2):1-226.
3. Wessel MM, Aaker GD, Parlitsis G, Cho M, et al. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2011 Nov 10. [Epub ahead of print]
4. Cho M, Kiss S. Detection and monitoring of sickle cell retinopathy using ultra wide-field color photography and fluorescein angiography. Retina 2011;31(4):738-47.
5. Chiang MF, Wang L, Busuioc M, et al. Telemedical retinopathy of prematurity diagnosis: Accuracy, reliability, and image quality. Arch Ophthalmol 2007;125:1531-8.
6. Photographic Screening for Retinopathy of Prematurity (Photo-ROP) Cooperative Group. The photographic screening for retinopathy of prematurity study (photo-ROP). primary outcomes. Retina 2008;28(3 Suppl):S47-54.
7. Dhaliwal C, Wright E, Graham C, et al. Wide-field digital retinal imaging versus binocular indirect ophthalmoscopy for retinopathy of prematurity screening: A two-observer prospective, randomised comparison. Br J Ophthalmol 2009;93(3):355-9.
8. Dai S, Chow K, Vincent A. Efficacy of wide-field digital retinal imaging for retinopathy of prematurity screening. Clin Experiment Ophthalmol 2011;39(1):23-9.
9. Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: Results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol 2003;121:1684-94.
10. Staurenghi G, Viola F, Mainster MA, et al. Scanning laser ophthalmoscopy and angiography with a wide-field contact lens system. Arch Ophthalmol 2005;123:244-52.
11. Atkinson A, Mazo C. Imaged area of the retina. Data on file, Optos.
12. Novotny HR, Alvis DL. A method of photographing fluorescence in circulating blood in the human retina. Circulation 1961;2482-6.
13. Muqit MM, Marcellino GR, Henson DB, et al. Optos-guided pattern scan laser (pascal)-targeted retinal photocoagulation in proliferative diabetic retinopathy. Acta Ophthalmol 2011 Dec 16. doi: 10.1111/j.1755-3768.2011.02307.x. [Epub ahead of print]