|
Medicare recently found two scoring errors related to the QPP/MIPS 2020 data which might affect you in a few months, and also changed the Cost scoring for this past year (remember that 2020 scoring affects your 2022 payments). There are also some changes to 2021 reporting that, though they might not impact every provider, in some cases you’ll have some decisions to make as we enter the last quarter of 2021. Even though the pandemic regulations are still in place, CMS has also instructed the MACs to re-start some of the audits that were on pause for that reason. Lastly, we discuss the (very) few changes to ICD-10-CM for 2022.
What changes has CMS made to QPP/MIPS for 2020 scoring?
On September 27, CMS noted that eye doctors might see some changes to their 2022 payment and performance adjustments. They found two errors. One is only for those providers enrolled in a Medicare Shared Savings Program or Accountable Care Organization; CMS found that in some cases they might not have attributed up to 10 complex patient bonus points. This means that CMS didn’t give the points they should have, so scores can only go up.
The other change affects only those who reported more than one “high priority” quality measure. CMS’ error was that the bonus points for the additional high-priority measures a practice reported were not credited, so scores can only go up and no scores can go down.
The downside to some QPP scores going up is that even if you’re not directly affected via a score, the overall budget neutrality provisions built into QPP might mean that your payment adjustments are slightly affected up or down; but these will be truly minor. If your increased score moved you into the exceptional performer category, that money is in addition to your already higher-than-average payment adjustment. Those who were already in the exceptional performer category but had no score change might see a slight dilution in their particular bonus due the effect on the pool of funds being spread further.
If you feel your score for 2022 is still incorrect, due to the changes above, CMS extended the appeal timeline—you now have until 8 PM Eastern on November 29 to request a targeted review.
What about the Cost category? My practice was closed or ran a severely reduced schedule for part of the year.
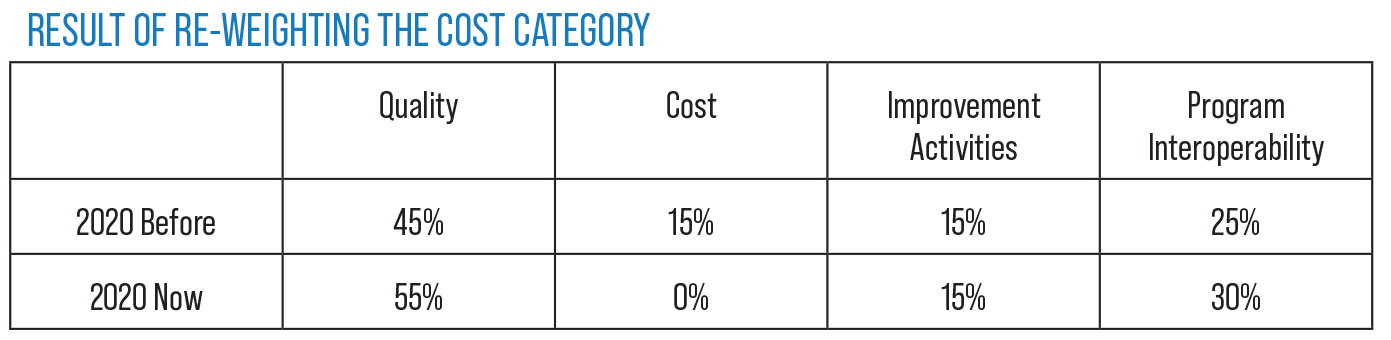
This is also good news. CMS announced in late summer that all eligible MIPS providers will automatically receive re-weighting of the Cost category from 15 to zero percent in their 2020 final calculation, regardless of their status in MIPS as an individual, group or virtual group, or their participation in an APM Entity. CMS noted that unlike some other re-weighting in the past, where it all went from one area directly to another, this 15-percent change is split between the Quality (10-percent increase) and Program Interoperability (5-percent increase) areas. The before-and-after weighting appear in the table above. If a practice has other re-weighting from hardship exceptions, CMS notes that those will remain in effect and this split from Cost re-weighting is additive.
 |
I was in an area that was affected by Hurricane Ida. Is there anything that can help me in 2021?
Yes. Those in the affected areas (New York, New Jersey, Louisiana, most of Mississippi and parts of Pennsylvania) will now be automatically identified by their billing ZIP code and will receive no negative adjustment in 2023. This new declaration is in addition to the waivers already in place due to the COVID-19 public health emergency (PHE). As with other “Extreme and Uncontrollable Circumstance” hardship exceptions, if you are affected but choose to submit MIPS data anyway in two or more MIPS categories for the 2021 reporting year, you will be scored and receive the adjustment.
You mentioned TPE audits. What are those?
This is a special type of audit with education afterwards. CMS announced in an August issue of the “MLNConnects” newsletter for the Medicare Learning Network (https://www.cms.gov/files/document/2021-08-12-mlnc.pdf) that Targeted Probe and Educate (TPE) audits would resume again after being paused as part of the COVID-19 pandemic.
CMS notes on the TPE webpage (www.cms.gov/Research-Statistics-Data-and-Systems/Monitoring-Programs/Medicare-FFS-Compliance-Programs/Medical-Review/Targeted-Probe-and-EducateTPE) the following information:
- CMS’ Targeted Probe and Educate program is designed to help providers and suppliers reduce claim denials and appeals through one-on-one help.
- MACs use data analysis to identify:
— providers and suppliers who have high claim error rates or unusual billing practices; and
— items and services that have high national error rates and are a financial risk to Medicare.
- Providers whose claims are compliant with Medicare policy won’t be chosen for Targeted Probe and Educate.
- [This type of audit] “typically involves the review of 20 to 40 claims per provider/supplier, per item or service. This is considered a round, and the provider/supplier has a total of up to three rounds of review.
“After each round, providers/suppliers are offered individualized education based on the results of their reviews. Providers/suppliers are also offered individualized education during a round when errors that can be easily resolved are identified.”
Any changes to ICD-10-CM for 2022?
Yes, but they’re very minor and won’t likely affect you much at all.
In the unusual situation in which you do actually encounter a condition that requires a new code, you must use the new codes as of October 1, 2021; don’t delay until January 2022 just because the “code year” says 2022.
Our specialty’s chapter of the ICD-10 code manual, (Chapter 7: Diseases of the Eye and Adnexa) had one minor change: Eliminating an improper “dash” on code I10 that you wouldn’t use on claims anyway.
Chapter 19 (Injury, Poisoning & Certain Other Consequences of External Causes) had similar changes to S00.1 (Contusion of eyelid and periocular area) and S01.0 (Open wound of scalp).
Chapter 12 (Diseases of the Skin and Subcutaneous Tissue) has a few changes that we actually might encounter when the skin is irritated. That change under L24 (Irritant contact dermatitis) is:
- Add: L24.A Irritant contact dermatitis due to friction or contact with body fluids
— Add: L24.A9 Irritant contact dermatitis due to friction or contact with other specified body fluids
In Chapters 13 (Diseases of the Musculoskeletal System & Connective Tissue) and 18 (Symptoms and Signs), the term that was previously used in the ICD-10 manual, “Sicca syndrome,” was replaced by the term “Sjögren syndrome” for M35.01 codes.
Chapter 20 (the strange chapter with all the external causes of morbidity) had lots of changes that don’t affect you unless your specific state Medicaid program requires their use—and even that would be rare, as most states’ programs don’t ask for or require them.



