Docking the Laser
Surgeons say there are steps you can take to avoid stumbling out of the gate when you start the procedure.
Inadequate suction while trying to dock the laser on the patient’s eye can scuttle a case. Vancouver, Wash., surgeon Brian Will says, in his experience, there are three patient-related reasons for this to occur. “The first is related to the patient’s presentation or actions that affect the quality of suction,” he says. “For instance, in a patient with high astigmatism, such as 4 to 6 D, the entire globe is kind of elliptical, not just the cornea. So, you’re trying to put a device on the football-shaped eye that was actually designed to be used on a spherical shape. You’re more prone to get a vacuum break in that situation, even with a silicone skirt on your device.
“The second reason,” Dr. Will continues, “is if you’ve got really tight lids or a small fissure. This will make it difficult to get full apposition of the vacuum ring on the globe. This type of eye is more prone to getting a vacuum break because it’s more challenging to get the skirt seated on the globe itself. The third patient-related reason is excessive lid squeezing, or instances when the eye tends to roll superiorly due to Bell’s phenomenon. These can torque the vacuum ring once it’s on the eye, and can cause a break in vacuum, as opposed to a patient who is well-fixated and not stressing or straining against the vacuum ring.”
Dr. Will says a second group of causes stems from improper technique. “A vacuum break can result from having some lashes under the silicone vacuum-ring skirt,” Dr. Will says. “Even a broken-off lash under there can cause it.
So, make sure the ocular surface environment is clean. A break can also happen if there’s a fold of the silicone skirt itself, or if it’s a small eye or tight lid that doesn’t give much room for the skirt to spread out into the fornices. A possible cause that was more common years ago than now is that there’s something wrong with the vacuum ring: The ring is either defective, such as an instance in which the silicone skirt isn’t perfect, or there’s a poor seal where the syringe meets the silicone. There can be a potential leak there.”
To deal with a suction break, Dr. Will says to first look for obvious problems. “Take out the failed ring and assess the situation,” he says. “Note how chemotic the conjunctiva is, and look around the lids and fornices for debris such as lashes. Have the patient blink to possibly clear debris. If need be, instill another drop of anesthetic if the patient is having some discomfort and squeezing a lot.” Dr. Will says it’s also important that the patient understands to be relaxed so as not to move during flap creation. Vance Thompson, MD, a surgeon from Sioux Falls, S.D., says this idea of preop patient communication about intraoperative movement is an important point. “The most common cause of suction loss is a slow drift,” Dr. Thompson avers. “It’s up to us to prepare the patient with pre-docking instructions. I tell him the best thing to do is hold still, but I define what that means: not just keeping the eye and head still, but also not moving the arms or legs or talking. We don’t do small talk because it creates movement.”
Dr. Will says, in many cases, the problem may be mechanical. “Most of the time, I’ll assume the vacuum ring is defective and just replace it,” he says. There’s not much downside to doing that, because the company will give you a new ring for free. However, never change the applanation cone if the suction break occurred during dissection.”
Dr. Will provides these other tips:
• if it’s a large flap, try shortening the diameter to shave seconds off the case to help ensure you can complete your treatment before another break occurs;
• use an open-wire lid speculum to control the lids better and to stretch redundant conjunctiva—which can result in a suction break—back in the fornices;
• in the absence of a speculum, go around the perimeter of the eye with your finger, retracting the lid and pulling it away from the edge of the vacuum ring; and
• put a little downward pressure onto the globe with the vacuum ring throughout the entire applanation.
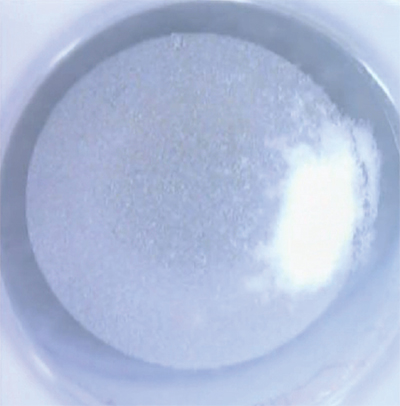 |
| Less energy, a smaller spot separation, regular laser maintenance and soft docking can help avoid an opaque bubble layer. (Image: Brian Will, MD) |
Surgeons say you can take steps to prevent or manage other events that occur during the LASIK case, as well.
• Opaque bubble layer. The photodisruption of the femto can result in bubbles that block subsequent laser pulses or interfere with the pupil tracker. Salt Lake City surgeon Majid Moshirfar, who is a professor of ophthalmology at the Moran Eye Center, says OBL can often be prevented with the proper steps. “Using less energy, using a smaller spot separation, maintaining the laser regularly and avoiding too much suction can help prevent OBL,” he explains.
“If you end up with OBL, it’s recommended that you wait three to 10 minutes, examine the patient either in the supine position or at the slit lamp and then attempt to lift the flap and continue with the treatment. The other recommendation: If the bubble layer is paracentral and you don’t think it’s going to impact the central 4 to 6 mm of the ablation zone, just lift the flap and continue.”
• Vertical gas breakthrough. This is when the photodisruption causes an upward-directed break in the corneal layers. “It’s analogous to the buttonholes we used to see with mechanical microkeratomes,” explains Dr. Moshirfar.
“But with them, they were quite central, while vertical gas breakthrough is usually peripheral and somewhat paracentral. I’ve never seen it in the center of a flap. Most of the time, vertical gas breakthrough happens due to some abnormality in the corneal density such as a scar or a subepithelial opacity due to contact lens use that caused subepithelial haze. If the gas breakthrough is very paracentral—not involving the central 6 mm—and it’s small, you can lift the flap, do the treatment and lay it back down. Many will place a bandage contact lens after such a treatment to ensure the vertical gas breakthrough doesn’t result in ingrowth in that area. However, if it’s larger than 0.5 mm x 0.5 mm, even if it’s paracentral, I recommend not lifting the flap and postponing the procedure. Maybe later you can consider creating a much thicker flap with a different device, possibly a microkeratome, or performing a PRK.”
• Corneal scar. A scar can cause problems with the femtosecond laser, but many cases are salvageable, surgeons say. “Since a scar, especially one from a previous foreign body removal, involves the loss of tissue, you could easily cause a stromal hole as you’re creating the flap,” says Dr. Thompson. “Then, as you use your LASIK spatula to dissect the plane, the tip can get into that hole and tear the flap. If we’re operating on someone with a scar, we try to go to a 130-µm flap, as opposed to our usual 110 µm. In the case of a subtle scar from contact lens use, we’ll note how much loss of tissue there is, and it’s not unusual that we can do these at 130-µm flap thickness. If it’s another type, such as from an injury, we probably aren’t going to do it. Note that, if the patient has a scar from Salzmann’s or early pterygium, the changes in the corneal stroma are often more pronounced than the scar looks.
The collagen in such cases is often disorganized, and the femto will go through it irregularly and result in an irregular flap.” Dr. Will says, since scars are often composed of disorganized collagen, the slit lamp can be misleading. “It’s helpful to assess the scar’s density by also viewing it with a pen light,” he says. “Use your own two eyes, because there’s often a disconnect between the scar’s density at the slit lamp and its density in natural light. The latter will be much more predictive of how much trouble you’ll have with flap creation.” REVIEW




