|
| (From left to right) Figure 1: After the three trocars are inserted in a standard three-port pars plana vitrectomy setup, with the infusion in place, the 23-gauge MVR blade is used to create four additional sclerotomies, two on the nasal side and two on the temporal side. These sclerotomies should be 4 mm apart on each side and equidistant from the corneal marks at the 3- and 9-o’clock positions. Figure 2: An Alcon 23-ga. Maxgrip forceps is used to enter the sclerotomy sites. I then complete a vitrecomy and lensectomy (if lens particles have fallen back into the vitreous cavity). Figure 3: If an IOL has dislocated into the vitreous cavity, I retrieve it from the posterior segment. Fig. 3 shows the vitrectomy and lensectomy. |
Technique
As a retina surgeon, I typically get patients referred to me for scleral-fixated PCIOL implantation when either the capsular bag has been violated intraoperatively and the patient is left aphakic with retained lens material or when a patient’s existing IOL/bag complex has subluxated out of the visual axis or has dislocated into the vitreous cavity. Following is a description of the technique I use in such cases.
• Scleral wounds. I make a conjunctival peritomy down to bare sclera at the 3- and 9-o’clock positions. I then use external cautery (eraser tip) to cauterize any bleeding vessels in the scleral bed, and insert three 23-gauge, valved trocars 3.5 mm from the limbus in the standard fashion in preparation for pars plana vitrectomy. The first trocar goes in the inferotemporal quadrant, the next one in the superotemporal quadrant and the last one in the superonasal quadrant, all done in a beveled fashion. I then insert the infusion into the inferotemporal trocar and set it at a pressure of 25 mmHg. When performing this step of the procedure, make sure to insert the trocars slightly more superior and inferior than usual (away from the horizontal meridians) to make room for the additional sclerotomies to come.
 |
| (From left to right) Figure 4: The surgeon uses a 2.75-mm keratome blade to create a triplanar incision at 12 o’clock. Figure 5: The Akreos lens is laid onto the corneal surface and CV8 Gore-Tex sutures are threaded through the lens eyelets. Figure 6: The distal suture end on the temporal side is introduced through the corneal wound and is transferred intraocularly to the bent Maxgrip forceps and externalized though the distal sclerotomy. |
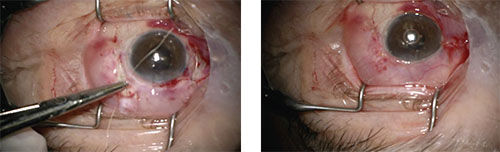
I use a toric marker to place two marks on the cornea 180 degrees apart, one at 3 o’clock and the other at 9 o’clock. I use calipers to make two marks 4 mm apart on either side of the sclera, 2.5 mm from the limbus. This amounts to two marks nasally and two marks temporally. The scleral marks should straddle and be equidistant from the corneal marks previously created to ensure proper lens centration. I then use the 23-ga. MVR blade (without the trocar) to create four sclerotomies, one at each of the marks that I just created (See Figure 1). I use a 23 ga. Maxgrip forceps (Alcon) to enter each of these fresh sclerotomy sites to ensure their patency (See Figure 2). It’s at this phase of the procedure that I complete a vitrectomy and a lensectomy if lens particles have fallen back into the vitreous cavity, and will also retrieve a dislocated IOL, if need be (See Figure 3). It’s also important to note that, depending on how much manipulation has been done to the eye or is planned, I have a low threshold for 360-degree prophylactic laser at the ora serrata to prevent postoperative retinal tears and detachment.
• Corneal incision. I then create a triplanar corneal incision at the 12-o’clock position and enlarge the wound on either side to a diameter of approximately 4 mm (See Figure 4).
A common pitfall to watch out for at this point in the procedure is shelving of the wound, so make sure to create a clean corneal incision. If shelving occurs, the suture and IOL may become caught in this incision during its introduction.
 |
| (From left to right) Figure 7: The proximal suture end on the temporal side is introduced through the corneal wound and is transferred to the bent Maxgrip forceps and externalized through the proximal sclerotomy. Figure 8: The Gore-Tex sutures have been externalized through the four sclerotomy sites on both the temporal and nasal sides. Figure 9: The lens is “taco folded.” |
• Suturing. I then lay the lens onto the corneal surface in the correct orientation, with the two eyelets with notches oriented in the upper right and lower left corners. I cut a CV8 Gore-Tex suture—with the needles removed—in half. One half is threaded through the two nasal eyelets and the other half is threaded through the two temporal eyelets (See Figure 5). Using two Maxgrip forceps (one in each hand), I use the “handshake” technique to externalize the sutures through the sclerotomy sites on both sides.
You can use a hemostat to bend one of the Maxgrip forceps to facilitate the suture hand-off. One Maxgrip forceps is used to grasp the end of the distal Gore-Tex suture on the temporal side and the suture end is introduced through the corneal incision. In the other hand, the bent Maxgrip forceps enters the distal sclerotomy site on the temporal side. The suture end is now passed off to the bent Maxgrip forceps and is then externalized through the distal sclerotomy site (See Figure 6).
I use the same technique to externalize the proximal end of the suture on the temporal side, and then externalize this end through the proximal sclerotomy (See Figure 7). Next, I use this handshake technique to externalize the distal and proximal Gore-Tex sutures on the nasal side (See Figure 8).
I insert Viscoat through the corneal wound to coat the endothelium and fill the anterior chamber, and clamp the infusion. At this point, I fold the lens in a “taco” shape with a tie forceps, and introduce it into the anterior chamber (See Figures 9 and 10). I gently pull the sutures on either side and the lens slides behind the iris plane.
A potential complication at this step is the sutures tangling intraocularly, which will result in the IOL not lying flat when it’s inserted. To avoid this entanglement, you have to pay meticulous attention to suture placement. If you notice the intraocular lens isn’t lying flat after insertion, check to see if one of the sutures is tangled on one of the contralateral eyelets, which is rather common. Attempt to untangle the suture with a Maxgrip forceps. If this isn’t possible, then remove either the temporal or the nasal suture, depending on the one that’s tangled. Then, reintroduce the suture, thread it through the two eyelets intraocularly, and then externalize the two suture ends.
 |
| (From left to right) Figure 10: After being taco-folded, the lens is manually inserted into the anterior chamber. Figures 11 and 12: The lens lies flat in the eye and the Gore Tex sutures are tied down in a 3-1-1-1 fashion on both sides. |
Once the lens is properly inserted intraocularly, I tie the Gore-Tex suture in a 3-1-1-1 fashion on both sides and bury the suture knot using one of the forceps (See Figures 11 and 12). Before locking the suture on either side, make sure the lens is well-centered. Also make sure the lens isn’t pulled so tightly that the eyelets bow on either side, which can lead to astigmatism.
• Closing the case. At this point, I close the corneal incision with 10-0 nylon sutures, take one more look at the retina and then remove the three trocars. If there’s any leakage, I close the sclerotomy with a 6-0 plain suture (See Figure 13).
At this stage, it’s crucial to ensure that the four additional sclerotomy sites aren’t leaking. You should have a low threshold for closing any or all of them with 6-0 plain sutures to avoid postoperative hypotony and choroidal detachment.
Finally, I close the conjunctiva at the limbus at the 3- and 9-o’clock positions and make sure that the Gore-Tex sutures are covered by the conjunctiva (See Figure 14). If the conjunctiva isn’t covering the Gore-Tex sutures completely, or the patient’s conjunctiva is extremely thin, there’s a significant risk of exposure of the suture, which can lead to endophthalmitis. If
 |
| Figure 13 (left): Close the sclerotomy sites with 6-0 plain suture, if leaking. Figure 14 (right): The conjunctiva is closed over the Gore-Tex sutures at 3 and 9 o’clock. |
The scleral-sutured Akreos or Cz70BD IOL using a Gore-Tex suture is an effective technique to use when there’s a lack of capsular support for an in-the-bag or sulcus placement. It’s important to note that the Akreos lens is hydrophilic acrylic, however, so there’s a theoretical risk of lens opacification when intraocular gas is used. Knowing this, in my own personal experience, if a postoperative retinal detachment occurs, SF6 gas is preferable to C3F8 in order to prevent potential complications from prolonged gas exposure. REVIEW
Dr. Rosenberg is in private practice at Retina Vitreous Surgeons of Central New York and is a clinical associate professor at SUNY Upstate Medical University.
Suggested Reading:
1. Cao, D, et al. Akreos Adapt AO Intraocular lens opacification after vitrectomy in a diabetic patient: A case report and review of the literature. BMC Ophthalmol 2016; doi: 10 10.1186/s12886-016-0268-3.
2. Khan, A, Gupta O, Smith R, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile Br J Ophthalmol doi:10.1136/bjophthalmol-2015-306839.