The incidence of epithelial ingrowth after LASIK has been reported to be as low as 0.2 percent and as high as 15 percent. Commonly reported figures are 0.92 percent after primary LASIK and 1.7 percent after enhancement procedures.
Epithelial ingrowth is the presence of corneal epithelium in an area where it does not belong. After LASIK, epithelial ingrowth can occur in the interface between the flap and the stromal bed of the patient's cornea. Corneal epithelial cells can be introduced into the interface in two ways: during the microkeratome pass or other parts of the procedure, or due to a loss of contact inhibition and the presence of a pathway to the interface.
When epithelial cells come in contact with epithelium, they stop growing, and this is called contact inhibition. If there is no contact inhibition, the epithelial cells will grow to fill that space.
Rarely, when a buttonhole develops in the LASIK flap, the epithelial cells from the surface of the cornea can go through the buttonhole and get into the interface between the flap and the stromal bed and create epithelial ingrowth.
Risk Factors
Patients with corneal epithelial basement membrane dystrophy and patients with recurrent corneal erosion are at risk for epithelial ingrowth after LASIK. Other risk factors include diabetes mellitus, older age, having had previous corneal surgery (such as RK or PK), and having had epithelial ingrowth in the fellow eye.
To avoid epithelial ingrowth, patient selection is very important. Patients with the risk factors mentioned above may achieve better results with PRK than with LASIK and, thus, avoid the possibility of epithelial ingrowth.
There are surgical risk factors, as well. These include buttonholes, partial flaps and enhancement procedures. Anytime a flap is re-lifted for an enhancement procedure, the risk of epithelial ingrowth increases. Another surgical risk factor is a thin flap with ragged edges. Excess manipulation of the flap should be avoided, and it is always a good idea to use new blades, along with minimal and careful use of topical anesthesia.
Additionally, a study suggested that the laser system used has an effect on the rate of epithelial ingrowth after LASIK.1 The study examined the incidence of epithelial ingrowth after LASIK using the Visx 20/20B and the Visx Star S3 laser systems. Patients with known risk factors for epithelial ingrowth were excluded from the study. Both eyes of patients who were operated with both laser systems were included in a paired analysis, and the first operated eyes of the remaining patients were included in an unpaired analysis. In the paired study, epithelial ingrowth occurred in 11 (61.1 percent) of the 18 eyes treated with the Visx 20/20B laser, and seven of these eyes required treatment. In contrast, none of the eyes treated with the Visx Star S3 had epithelial ingrowth. In the unpaired study, 39 (37.1 percent) of 105 eyes treated with the Visx 20/20B had epithelial ingrowth, and 14 eyes required treatment. Again, none of the eyes treated with the Visx Star S3 experienced epithelial ingrowth. This study concluded that the laser system used in LASIK is a risk factor for the development of epithelial ingrowth.
Grades of Ingrowth
There are three different grades of epithelial ingrowth, according to Jeffrey Machat's classification. Patients with Grade 1 epithelial ingrowth will have epithelial ingrowth that is less than 2 mm from the edge of the flap, and there will be a clear demarcation line. There is no change in the flap. Grade 2 is similar to Grade 1, because the epithelial ingrowth will be less than 2 mm from the flap edge, but, with Grade 2, there is no demarcation line. The epithelial cells look grayish-white, and there is very slow progression. With Grade 3, the ingrowth is more than 2 mm from the flap edge, and it extends toward the visual axis. Flap changes can include melting of the flap or erosion. Additionally, the cells look thick, opaque and whiter than other epithelial cells.
A recent Japanese study found that the clinical appearance and histopathology of epithelial ingrowth from LASIK flap margins differ in early and late stages.2 The study included five epithelial ingrowth specimens from four patients who had undergone initial LASIK procedures two to 17 months previously. The lesions were surgically removed and were examined using light and transmission electron microscopy. Early epithelial ingrowth was clinically observed as faint opacities with demarcation lines and epithelial pearls, while late epithelial ingrowth was observed as homogeneous whitish masses. Histopathologically, early epithelial ingrowth consisted of multilayered squamous epithelium resembling normal corneal epithelium, while late ingrowth consisted of clumps containing amorphous materials with scarce cellular elements.
Signs and Symptoms
In many cases, patients with epithelial ingrowth after LASIK may have no symptoms. Patients with more severe cases may have foreign body sensation, photophobia, discomfort, irritation or pain. Depending on the severity, patients may also have glare, haloes and loss of best-corrected visual acuity.
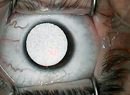
Epithelial ingrowth looks like white or gray nests of cells. Sometimes, finger-like extensions from the flap edge can be seen. If the patient has a buttonhole in the center of the flap and epithelial ingrowth, the extensions appear near the buttonhole. With nasally hinged flaps, epithelial ingrowth is commonly seen in the temporal margin. With superiorly hinged flaps, ingrowth commonly occurs at the inferior margin and at the border of the hinge.
Epithelial ingrowth can cause regular or irregular astigmatism. Additionally, if the epithelial cells become necrotic, they release enzymes like collagenase and protease, which can cause melting of the flap and the stromal bed. As a result, patients can experience a decrease in vision.
Treatment
For mild and non-progressive epithelial ingrowth (Grade 1), no treatment is required. Carefully observe these patients to ensure that the ingrowth is not progressing. A recent case study concluded that surgery is only necessary when the epithelium appears to be progressing, affects visual function, or causes flap melting.3 In this particular case, a 34-year-old woman underwent bilateral LASIK. On the first postoperative day, a large downward displacement of the flap in the right eye was observed. The flap was repaired, but, one month later epithelial ingrowth from the flap edge was noted at the 1, 5, 8 and 11 o'clock positions. Without any treatment, the epithelial ingrowth regressed. At 15 months postoperatively, all epithelial ingrowth had resolved except for that at the 5 o'clock position. At 20 months postoperatively, the ingrowth at the 5 o'clock position had also regressed.
A number of techniques have been described for managing epithelial ingrowth. In general, when treatment is indicated, the surgeon will need to lift the flap and scrape the epithelial cells, both from the undersurface of the flap and from the stromal bed. It is a good idea to resect the epithelium from around the flap bed.
Use balanced salt solution to irrigate the interface, the flap and the stromal bed to ensure the removal of all of the epithelial cells. Then, tightly replace the flap. It is a good idea to put on a bandage contact lens; however, a recent study found that using bandage contact lenses can cause a recurrence.4
This study compared the incidence of postoperative epithelial ingrowth using three different surgical LASIK retreatment techniques. The retrospective, consecutive case series included 30 eyes that underwent LASIK retreatments by a single surgeon. Ten eyes underwent retreatment using forceps to lift the flap. The next 10 retreated eyes had a bandage contact lens placed after surgery and removed the following day, and the other 10 eyes had retreatment performed using a Pinelli spatula to cleave the circumference of the flap edge before lifting the flap. These patients did not have a contact lens placed after surgery.
According to the study results, the incidence of epithelial ingrowth was 40 percent in the contact lens group, 20 percent in the forceps lift group, and 10 percent in the spatula cleaving group. Additionally, the patients with the epithelial ingrowth were older, with a mean age of 53 ±8.5 years compared with a mean age of 44 ±13 years for patients without epithelial ingrowth.
Another recent study found that severe progressive epithelial ingrowth may be treated successfully with a combination of mechanical debridement, flap suturing and fibrin glue application.5 This case report described a 42-year-old woman who underwent LASIK in 1998 and an enhancement in 2002. Two years after the enhancement, she developed severe, visually significant epithelial ingrowth. She was treated with a combination of mechanical debridement, flap suturing and fibrin glue application, and no recurrence and no adverse effects were observed during the 15-month follow-up period.
Similar results were observed in a second case report,6 which described a 50-year-old woman who presented 21 months after uncomplicated LASIK with painful vision loss in the right eye after minor trauma. On examination, a dislocation of the flap was noted, and the flap was repositioned. One week later, epithelial ingrowth was observed in the flap interface, and the ingrowth was treated with flap lifting, debridement and fibrin glue application. This patient's visual acuity returned to baseline, and no recurrence was observed after 20 months of follow-up.
A separate study evaluated the safety and efficacy of flap suturing with proparacaine application for the management of recurrent epithelial ingrowth after LASIK.7 This study included six eyes of five patients with recurrent epithelial ingrowth who underwent flap lifting followed by debridement of interface epithelial cells, interface application of proparacaine, and the placement of interrupted 10-0 nylon sutures. In this study, four eyes achieved a best-corrected visual acuity of 20/40 or better, and two eyes required repeat debridement with suturing. These two eyes were stable after one year of follow-up. None of the eyes lost more than one line of BCVA.
Additionally, amniotic membrane overlays have been found to be an effective adjuvant therapy to secure a LASIK flap when direct suturing would threaten the visual axis.8 In one study, two patients had epithelial ingrowth after LASIK that created defects in the flap near the visual axis. After removing the epithelium, an amniotic membrane patch was sutured tightly to the episclera so that it covered the entire cornea, and it was left in place for one week. After four months, there was no evidence of recurrent epithelial ingrowth.
Lasers have also been used in combination with manual scraping with good results.9 In Sweden, three patients who had undergone several surgeries after LASIK to remove epithelial ingrowth were treated with a flap lift, manual debridement of the epithelial cells, and phototherapeutic keratectomy. PTK was performed on both the stromal and the flap sides. Uncorrected visual acuity and best spectacle-corrected visual acuity remained the same or improved. While central epithelial ingrowth did not recur, peripheral ingrowth did.
The use of mitomycin C in these patients has also been described.10 One study in
Dr. John is a clinical associate professor at Loyola University at Chicago and in private practice in Tinley Park and Oak Lawn, Ill., and Hammond, Ind. Contact him at (708) 429-222, (219) 845-2020, or by e-mail at lasikcornea@gmail.com.
1. Jun RM, Cristol SM, Kim MJ,
2. Asano-Kato N, Toda I, Hori-Komai Y, Takano Y, Dogru M, Tsubota K. Histopathological findings of epithelial ingrowth after laser in situ keratomileusis. Cornea 2005;24:130-134.
3. Lin JM, Tsai YY, Tseng SH. Spontaneous regression of dense epithelial ingrowth after laser in situ keratomileusis. J Refract Surg 2005;21:300-302.
4. Chan CC, Boxer Wachler BS. Comparison of the effects of LASIK retreatment techniques on epithelial ingrowth rates. Ophthalmology 2007;114:640-642.
5. Narvaez J, Chakrabarty A, Chang K. Treatment of epithelial ingrowth after LASIK enhancement with a combined technique of mechanical debridement, flap suturing, and fibrin glue application. Cornea 2006;25:1115-1117.
6. Yeh DL, Bushley DM, Kim T. Treatment of traumatic LASIK flap dislocations and epithelial ingrowth with fibrin glue. Am J Ophthalmol 2006;141:960-962.
7. Spanggord HM, Epstein RJ, Lane HA, et al. Flap suturing with proparacaine for recurrent epithelial ingrowth following laser in situ keratomileusis surgery. J Cataract Refract Surg 2005;31:916-921.
8. Lee ES, Lee HK, Cristol SM, et al. Amniotic membrane as a biologic pressure patch for treating epithelial ingrowth under a damaged laser in situ keratomileusis flap. J Cataract Refract Surg 2006;32:162-165.
9. Fagerholm P, Molander N, Podskochy A, Sundelin S. Epithelial ingrowth after LASIK treatment with scraping and phototherapeutic keratectomy. Acta Ophthalmol Scand 2004;82:707-713.
10. Taneri S, Koch JM, Melki SA, Azar DT. Mitomycin-C assisted photorefractive keratectomy in the treatment of buttonholed laser in situ keratomileusis flaps associated with epithelial ingrowth. J Cataract Refract Surg 2005;31:2026-2030.