|
EOMs : Anatomy and Biomechanics
The eyes lie in the orbits, two symmetrical bony cavities of the skull that are situated on either side of the nasal root (See Figure 1). The standard set of six extraocular muscles (EOMs) move the eye in the horizontal, vertical, oblique and rotary planes. The medial rectus (MR) and lateral rectus (LR) course forward from the orbital apex along the medial and lateral aspects of the globe, respectively, to adduct and abduct the globe in all positions of horizontal gaze.
The superior and inferior recti and the superior and inferior oblique eye muscles have more complicated actions, depending upon the starting position of the eye in the orbit. Figure 2 shows the anatomic orientation of the SR muscle.
It courses forward at an angle of 23 degrees to the medial wall of the orbit and attaches to the globe superiorly. With the eye abducted 23 degrees, the plane of the SR parallels the vertical anterior-posterior plane of the globe. In this position, contraction of the SR elevates the eye. With the globe adducted 67 degrees, the plane of the SR muscle becomes perpendicular to the visual axis, and its contraction intorts the eye. In the primary position of gaze the movement is combined elevation and intorsion plus slight adduction; the adduction results from the midline of the muscle belly being medial to the center of rotation of the globe with the eye in primary position.
|
The SO muscle originates in the orbital apex and courses forward along the superior-medial wall of the orbit to the trochlea, where it becomes tendinous (See Figure 3). After passing through the trochlea, the tendon reflects back temporally at an angle of 51 degrees with the medial wall of the orbit. It passes dorsally over the globe, ventral to the SR muscle, and inserts in the posterotemporal sclera. Since the reflected tendon delivers the direction of force to the scleral surface, the movement of the eye varies with respect to the plane of the superior oblique's tendinous insertion. Starting from a position of 51 degrees of adduction, where the plane of the superior oblique muscle tendon parallels the visual axis, the superior oblique pulls the eye downward. In the primary position, the movement is combined intorsion and slight abduction; the abduction results from the tendon being posterior to the rotation center of the globe. Starting from an eye position of 39 degrees abduction, where the visual axis is perpendicular to the superior oblique muscle plane, the superior oblique will intort the globe.
The course of the IR parallels the SR muscle and the IO parallels the tendinous portion of the SO muscle. The superior and the inferior recti muscles play a more important role in moving the eyes in the vertical plane. The superior and the inferior oblique muscles have a stronger torsional action on the globe.
A Single Paretic Vertical Eye Muscle
• Law of Projection of Images. This law establishes that an object that forms its image on any point in the retina is projected to a point in visual space directly opposite, and when a distant object is viewed with two normally seeing eyes, the visual axes are parallel. Conjugate gaze up and to the right, for example, is accomplished by conjugate movement of the eyes to the right and simultaneous and equal innervation to the right SR and the left IO muscles. Each EOM moves the eye in the same distance and at the same speed to attain precise "foveation." If there is an interocular difference in the speed or extent of eye movement, the fixational target falls on non-corresponding points in the retina and diplopia results. It follows that conjugate movement of the eyes further into the field of the weakened eye muscle will increase the amount of retinal non-correspondence and, therefore, increase the distance between disparate images.
• History-Taking. Utilizing the Law of Projection of Images, gathering the history from the patient should include these four questions:
1) Is your double vision present in straight-ahead gaze?2) Do the images separate more when you look to your right or left?3) If it worsens in right gaze, does it worsen in gaze right and up or gaze right and down?4) What happens if you tilt your head to the right or left shoulder?
An affirmative response to question 1 delimits the differential diagnosis of double vision to the four pairs of EOMs that move the eyes vertically. These include the right and left SR, IR, SO and IO muscles. If diplopia worsens in right gaze, for example, the number of suspect EOMs narrows from eight to four, since only the right SR, right IR, left IO and left SO move the eye vertically in right gaze. Greater diplopia with eyes to the right and up implicates the right SR or left IO, while worsening of diplopia to the right and down points to the right IR or left SO. If diplopia worsens in right head tilt, the right eye intorters or the left eye extorters are underacting; just the opposite applies if diplopia worsens in left head tilt.
One very important point to emphasize is to not assume that a limitation of eye movement is related to EOM weakness. Always use the word underacting rather than weakness of an eye muscle, to remind yourself that incomplete excursion of the globe can result from weakness of the agonist EOM, tethering of the antagonist EOM or inhibition of the contralateral antagonist.
• Anomalous head postures. Since binocular diplopia either worsens or improves in different positions of gaze, the symptomatic patient may adopt a compensatory head, face or chin posture that gives him best binocular single vision (BSV). With horizontal eye muscle weakness the patient tends to turn her face to the side of the underacting horizontal rectus muscle to relieve diplopia. A turn of the face to the right involuntarily throws the eyes to the left and avoids the diplopia in right gaze caused by underaction of the right lateral rectus muscle. Underaction of the superior or inferior rectus muscles, which primarily moves the eye in a vertical plane, is compensated for by chin flexion or extension.
Figure 4 depicts a patient's head posture with underaction of the right SR muscle. To avoid the gaze position that engenders action of the paretic right SR, i.e., elevation in abduction, she lifts her chin backward and to the right (toward the action of the right SR), which via the Doll's eye reflex moves the eyes down and to the left, away from the field of maximum action of the paretic right SR.
|
The 12 o'clock point on the cornea is conventionally taken as the vertical pole. If the 12 o'clock point is pulled nasally the eye movement is referred to as intorsion or incycloduction; when the 12 o'clock point is rotated outward the globe is said to be excycloducted or extorted. Torsional diplopia is characterized by one image being rotated clockwise or counter-clockwise away from the other. It is almost always caused by underaction of a superior or inferior oblique eye muscle, since the main action of these EOMs, at least in the primary position of gaze, is to intort and extort the globe, respectively. Torsional diplopia can be relieved by an angular tilt of the head to the right or left shoulder. Normally as the head is tilted to the left shoulder, the left eye intorts and the right eye extorts. In this case, left eye intorsion is accomplished by cocontraction of the left SO and left SR, and right eye extorsion by contraction of the right IO and IR. Figure 4 depicts the pattern of diplopia and the compensatory head position assumed by a patient with a left superior oblique muscle palsy.
Red-Glass, Double- Maddox Tests
The subjective red-glass and double-Maddox rod tests allow the patient to articulate the relative positions of the disparate images. Assuming that the normal, non-paretic eye is used to fixate, the image projecting into the paretic eye will fall onto extrafoveal retina. The amount of retinal non-correspondence increases as the eyes moves further into the field of action of the compromised eye muscle.
The patient interprets this non-correspondence as double vision. By putting a red lens before one eye, the locations of the two disparate and different-colored images can be described in all nine cardinal positions of gaze and in head tilt to the right and left shoulder (See Figure 5).
|
The double-Maddox rod test, a variation of the red-glass test, utilizes a red and a white Maddox lens to document torsional diplopia in a patient with suspected weakness of a superior or inferior oblique muscle (See Figure 6). As an example, a person with a right superior oblique muscle palsy, in whom the red lens covers the right eye, will describe the red line to be lower than the white line and intorted, because the right eye behind the red lens is relatively hypertropic and extorted. The examiner or patient then turns Maddox rod until the two lines are parallel. The magnitude of cyclotropia can be read off the trial frame, and the direction of deviation is indicated by the displacement of the scratch mark on the Maddox rod from the 90-degree mark on the trial frame.
Pitfalls
|
Ocular Ductions and Versions
When a patient follows your finger through the full range of eye movements, check the speed and extent of each eye while both eyes move together (versions). Then cover one eye and observe the monocular movements of the uncovered eye (ductions). If one eye shows a limitation of vertical movement, for instance, be careful not to assume there is weakness of the elevator or agonist muscles in the right eye. Do not forget the other two possibilities, tethering of the antagonist or inhibition of the contralateral antagonist.
Inhibition of the contralateral antagonist describes an anomaly of ocular motility that results when a patient with an EOM palsy fixates with the paretic eye. It most commonly causes confusion between true paresis of a superior oblique and apparent paresis of the contralateral superior rectus. Figure 7 shows the pattern of ocular ductions and versions in an 18-year-old woman who presented with vertical diplopia 10 years after a motor vehicle accident. There was no history of strabismus, patching or surgical eye-muscle treatment. On examination, visual acuity was 20/15 in the right eye, 20/25 in the left. Ocular versions in gaze up and to the left showed a limitation of left eye elevation, suggesting a left superior rectus palsy. But, ductions of the left eye to the left and up were full.
|
The subnormal innervation to the right IO is simultaneously transmitted to its yoke eye muscle in the left eye, the left SR. Thus, with both eyes open and the right eye fixating, the left eye does elevate fully in gaze to the left and up, because of inhibition of the left SR. The examiner must not rely solely on versions to decide the underacting EOM. First determine which eye is used for fixation and then check ocular ductions in addition to ocular versions. While versions may show a limitation of eye movement, ipsilateral ductions will be full and the three-step test will correctly identify the weak eye muscle in a patient with inhibition of the contralateral antagonist.
Cover-Uncover Test
The monocular cover-uncover test may accomplish four goals: it determines fixational preference; it qualitatively identifies a heterotropia; it can be used to quantify the amount of deviation in various positions of gaze and head position; and it will identify a phoria of the eye behind the occluder.
The patient is encouraged to binocularly fixate on a target while the examiner occludes one eye at a time. As one eye is covered the movements of the uncovered eye are observed. If there is no movement of the uncovered eye—and the eye has good vision—it can be assumed to be accurately fixating. If the uncovered eye takes up fixation or refixates, it must not have been aligned with fixation under binocular conditions. Such a manifest deviation under binocular conditions is called a tropia. The eye with a manifest tropia will make a rapid or saccadic eye movement to take up fixation. If the movement of redress is downward, the eye under binocular conditions was hypertropic; if the movement is upward, the eye was hypotropic, if inward, exotropic and, if outward, esotropic.
The cover-uncover test test can also identify an ipsilateral phoria, if the eye under cover moves right, left, up or down. The most important use of the cover test is to identify the eye used for fixation and the presence of a manifest deviation (tropia). Remember that it does not determine which eye muscle is weak, since a patient may prefer to fixate with their paretic eye. A manifest deviation can be quantified either with the prism-cover test or the cover-uncover test. In the latter, the occluder is moved alternately from one eye to the next in rapid succession while the examiner adjusts the prism bar to neutralize any eye movement. The relatively rapid movement of the occluder prevents binocular fixation. Hence, both phorias and tropias are identified. Both the cover test and the alternate cover test can be used to quantify a tropia in all nine cardinal positions of gaze and in head tilt to the right and left shoulder. Both examinations are predicated on a patient's good vision and cooperation.
Pitfalls
These tests depend on good vision in each eye. Poor vision or inadequate cooperation diminishes their value. A deviation of less than 1 degree may escape detection, and a small-angle strabismus with eccentric fixation cannot always be diagnosed with these techniques, as the amblyopic eye may fail to perform a detectable fixation movement when the sound eye is covered.
The Three-Step Test
The three-step test simply is a variation of the cover-uncover test. It will quickly and accurately provide the diagnosis of a weakened vertical eye muscle. Each step reduces by one-half the number of muscles that could possibly be causing the vertical imbalance.
• Step 1. Determine whether there is a right or left hypertropia in primary position. With a right hypertropia, either the right globe is too high (hypertropic) due to weakness of the right eye depressor muscles (right IR and SO), or the left eye is too low (hypotropic) because of weakness of the left SR or IO.
• Step 2. Compare the amount of vertical deviation in right and left gaze. If the RHT increases in left gaze, either the right SO or the left SR is underacting, since these two muscles primarily move the eyes vertically in left gaze. At this point, note that the two muscles under suspicion are in different eyes, but both are intorters.
|
• Step 3. Compare the vertical deviation in right head tilt and left head tilt. If the vertical deviation increases with right head tilt (which reflexly causes incyclodeviation of the right eye and excyclodeviation of the left eye) the right SO must be underacting; if the hyperdeviation increases on left head tilt, the left superior rectus is underacting.
The explanation is simple. When the head is tilted to the right shoulder, the right globe normally intorts from the actions of the right SO and right SR. With weakness of the right superior oblique the right superior rectus acts alone to accomplish the intorsion. The right hypertropia becomes greater in right head tilt because the right SR receives a larger than normal innervational input to intort the right globe. Since the primary action of the right SR is to elevate the globe, the supernormal innervation not only helps to intort the right globe, but secondarily moves the globe higher, as the weak right SO does not oppose the elevating action of the superior rectus.
Pitfalls
Although the three-step test provides objective evidence of vertical muscle function, the results may be spurious in the face of certain causes of vertical strabismus.1 Example: a 52-year-old man complained of vertical and torsional diplopia after a mild head injury. Results of motility examination showed a 10 PD left hypertropia in primary position that increased to 24 PD in right gaze, and 15 PD on left head tilt, seemingly indicating a left SO muscle palsy. But, as a result of longstanding amblyopia in the left eye, the patient preferred to fixate with the right eye. On checking ocular rotations the right eye did not elevate well during version and ductional eye movement. Left eye movement was full. Forced ductions in the right eye were positive and orbital films showed a right orbital floor fracture with entrapment of the right IR muscle. After surgical repair the patient was orthotropic in primary position and his motility pattern no longer mimicked a left SO muscle palsy, according to the three-step test.
With entrapment of the right IR muscle, and the patient's preference to fixate with the right eye, the ipsilateral antagonist of the entrapped right IR, the right SR, enlists a supernormal innervational signal to maintain the right eye in primary position for fixation. Since the fixating right eye determines innervational input to both eyes, the supernormal innervation to the right SR is simultaneously transmitted to its contralateral yoke, the left IO. Hence, the left globe moves up in primary position. In right gaze, the right SR exerts an even stronger effort against the tethered right inferior rectus and the supernormal input to the left IO causes the left eye to elevate even further. In left head tilt, the left eye intorts via contraction of the left SR and left SO and the right eye extorts via the right IR and right IO. The tethered right IR pulls the right eye down; hence, the left eye is relatively higher, and the three-step test produces a LHT in primary position that worsens in right gaze and left head tilt—a pattern that usually indicates weakness of the left SO muscle.
Patients with tethering of an inferior rectus muscle may be mistakenly diagnosed as a superior oblique muscle palsy in the unaffected eye, if the examiner relies solely on the three-step test.2 Using the same algorithm, contracture of a superior rectus muscle, e.g., from thyroid ophthalmopathy, can produce a "pseudo-weakness" of the contralateral inferior oblique by three-step criteria.3 These diagnostic errors are more likely to occur if the patient fixates with the "tethered" eye. This case again emphasizes the importance of establishing which eye has better vision and which eye is primarily used for fixation.
A simple test for determining fixational preference involves the principles of primary and secondary deviation. Patients are asked to look at a fixation light while a red glass is placed before either eye, and they are instructed to report if the separation is greater when they look with their right or left eyes. Since secondary deviation is always greater than primary deviation and occurs with the paretic eye fixating, the patient's observations betray the fixating eye.
The mercurial ophthalmoplegia of myasthenia gravis can confound the most conscientious three-step tester. Myasthenic ophthalmoparesis can mimic a variety of ocular motility disorders, including brainstem gaze palsies, cranial neuropathies and primary orbital disease. Further confusion may arise because the extraocular muscle weakness tends to vary from one examination to the next. A history of acquired, highly variable diplopia, with or without ptosis, suggests the diagnosis of myasthenia. When in doubt, an intravenous Tensilon test should be performed.
Dissociated vertical divergence may bear several characteristics similar to an oblique muscle palsy.
• It may increase in adduction, particularly if there is an associated inferior oblique overaction.• A spontaneous head tilt is often present to fuse images.• It characteristically increases on forced head tilt (but usually to the contralateral side).
To avoid an erroneous diagnosis of dissociated vertical divergence, the examiner must assess the hypertropia by cover test rather than by light reflex alone. On cover testing, the dissociated nature of the deviation will be evident. In contrast to hyperphoria or hypertropia, in which the eyes move in different directions to refixate, each eye drifts upward in dissociated vertical divergence when the fellow eye is fixating.
Some patients with neurogenic horizontal strabismus show small nonneurogenic vertical deviations on forced head tilting, with no evidence of actual vertical muscle paresis. Consider the example of an 11-year-old boy who had a large 50-PD esotropia in primary position. After neutralizing the horizontal deviation there was a 4-PD right hypertropia that increased on right gaze and on left head tilt. Yet, ductions and versions showed no overaction or underaction, and double-Maddox rod testing showed no signs of torsional weakness. By three-step criteria, the vertical extraocular muscle findings were compatible with underaction of the left inferior oblique. But this only represented a small, non-paralytic vertical deviation in association with a large horizontal strabismus.
Patients with esotropia typically have shown each eye elevating on contralateral head tilt and depressing on ipsilateral tilt.4 Patients with exotropia, in contrast, typically showed elevation on ipsilateral tilt and depression on contralateral tilt. This type of deviation can be differentiated from a true vertical muscle paresis in several ways: 1) The ocular rotations do not show substantial limitations or overactions of the vertical eye muscles, as seen with vertical muscle pareses. 2) Patients with an oblique muscle palsy tend to have a substantial difference in the vertical deviation between right and left gaze. 3) These patients do not spontaneously assume a head tilt to fuse, and they do not exhibit objective or subjective torsional diplopia.
Hirschberg and Krimsky Tests
While the patient is asked to view an illuminated light source, the deviation of the corneal light reflex from the center of the pupil is estimated. With the fixation light held 33 cm from the patient, a 1-mm decentration corresponds to 7 degrees of ocular deviation. Most examiners agree that if the abnormal pupillary reflex just touches the temporal pupillary border, that eye is approximately 15 degrees esotropic; if it lies in the center of the iris stroma, there are 30 degrees of esotropia, and if it is on the outer limbic margin, there are 45 degrees of esotropia.
Utilizing the same equipment, with the addition of a prism, the light reflexes can be made symmetric. Prisms of increasing power are placed before the fixating eye until the light reflex is centered in the deviating eye. The prism with sufficient power to achieve centration of the light reflex indicates the magnitude of the deviation. The examiner must sit directly in front of the deviating eye in order to avoid false readings caused by parallax. This is sometimes referred to as the Krimsky test.
Pitfalls
These tests estimate the size of the ocular malalignment by observing the deviation of the corneal light reflexes. Its disadvantages are obvious: the lack of precision obtained with this methodology; deviations up to 7 degrees may be overlooked; anatomic alterations of the pupillary opening, such as ectopically-placed pupils and ectopic foveation, can also obscure normal fixational reflexes.
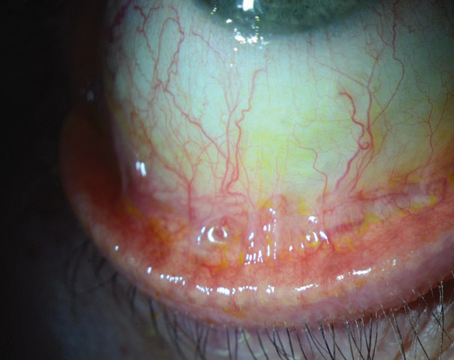
Forced Duction, Forced Generation
The forced duction test can be used to differentiate between limitation of eye movement from denervation of the agonist eye muscle and tethering of the antagonist eye muscle. If the examiner cannot move the globe in the direction of gaze limitation, forced ductions are said to be positive and it can be assumed that there is a mechanical or restrictive component.
Technique is important in performing the forced ductions test. It begins with putting a drop of topical anesthetic (proparacaine or tetracaine hydrochloride) on the conjunctiva, followed by holding a cotton swab soaked with 5 to 10% cocaine against the area of the conjunctiva for approximately one minute. The patient is then asked to move his eyes as far as possible in the direction of presumed weakness. Assuming there is an abduction paralysis of the right eye, the examiner, with a fine-toothed forceps, grasps the conjunctiva of the right eye near the medial limbus and attempts to abduct the globe. If no resistance is encountered, forced ductions are negative and the motility defect is not restrictive. Failure to passively move the globe is considered a positive forced duction, which indicates mechanical limitation of eye movement.
Several types of positive forced duction tests have been described.5 1) If the globe can be rotated no further than voluntary gaze the restriction, in the author's opinion, is due either to scar tissue or to stiffness of the muscle itself opposite the gaze limitation, i.e., the antagonist. 2) Forced ductions may also be positive, on rare occasions, with restrictive conditions of the agonist extraocular muscle. 3) In patients with longstanding extraocular muscle palsy, in whom there may be foreshortening of the antagonist, forced ductions may reveal that the globe rotates farther than the patient's voluntary gaze, but stops short of full and free excursion.
Pitfalls
Pitfalls of the forced auction test: Several technical errors may invalidate the conclusions of the forced duction test. When rotating the globe, it is important to follow the natural arc of rotation, as this is the best way to detect increased resistance as compared to rotations in the uninvolved directions. If one unintentionally pushes the globe inward, the examiner can simulate full rotations by retraction of the globe. It is important to grasp the globe as close to the limbus as possible, where the conjunctiva and Tenon's connective tissue join into one layer. If the globe is held more posteriorly, the conjunctiva may stretch and the force of the forceps will not effectively rotate the globe. Good patient cooperation is mandatory. If the patient does not voluntarily look in the direction requested, the antagonist muscle may continue to be innervated, causing the examiner to feel resistance which does not represent true mechanical restriction.
There are also clinical situations in which the forced duction test may provide spurious information. For instance, when there is co-contraction of EOMs, as in aberrant regeneration of the third nerve or Duane's syndrome. In the latter, the effect of forced ductions is admittedly variable.
While the forced ductions test gives clinically useful information about the presence of a restrictive ophthalmopathy, i.e., the status of the antagonist extraocular muscle, the active forced generation test helps to establish the "strength" or amount of active force exerted by an agonist EOM. One author has described the use of an oculomyodynamometer to measure the strength of an extraocular muscle.6 Later modifications and investigations led investigators to conclude that 60 to 80 gm of force was produced by a normal rectus muscle during extreme horizontal or vertical gaze.
In studying patients with paralytic and restrictive ophthalmopareses,7 it was found that a paretic muscle generated only a fraction of this normal force, and muscles functioning against a tethered extraocular muscle seemed to generate supranormal forces. Such testing results have been used for determining the amount of residual inferior rectus paresis alter an orbital floor fracture8 and for surgical planning. If active forced generations reveal signs of a complete paralysis of an extraocular muscle, for instance, the surgeon may elect to perform a muscle transposition procedure rather than a simpler resection and recession.
In an upcoming issue, I will describe the differential diagnosis of vertical diplopia and the methodology of isolating the correct diagnosis.
Dr. Spector is in private practice. Contact him at 980 Johnson Ferry Road, Ste. 550, Atlanta, Ga. 30342. E-mail:
fstop007@bellsouth.net.
1. Kushner BJ. Errors in the three-step test in the diagnosis of vertical strabismus. Ophthalmology 1989;96:127-132.
2. Moster ML, Bosley TM, Slavin ML, Rubin SE. Thyroid ophthalmopathy presenting as superior oblique paresis. J Neuro Ophthalmol 1992;12:94-97.
3. Jampolsky A. Management of vertical strabismus. Trans New Orleans Acad Ophthalmol 1986;34:141-171.
4. Moore S, Cohen RL. The head tilt test in horizontal strabismus. Am Orlhopt J 1987;37:105-108.
5. Metz HS. Forced duction, active forced generation and saccadic velocity test. In: Ellis FD, Helveston FM. Strabismus Surgery. Boston: Little Brown, 1976.
6. Madroszkiewicz M. Oculomyodynamometry: the strength and work of extraocular muscles in squint. Ophthalmologica 1970;6:491-495.
7. Scott AB. Active force tests in lateral rectus paralysis. Arch Ophthalmol 1971;5:397-401.
8. Melt HS, Scott WE, Madson E, Scott AB. Saccadic velocity and active force studies in blowout fractures of the orbit. Am J Ophthalmol 1974;78:665-670.