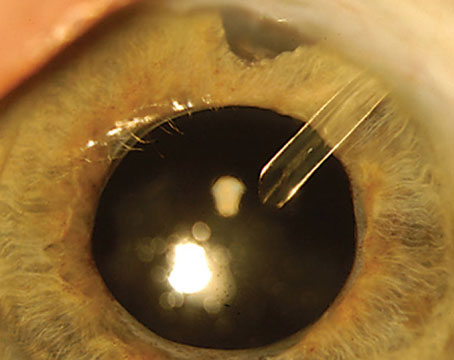
A recent analysis found that uveitis developed in about half of individuals with herpes zoster ophthalmicus, with diagnosis occurring most often in the second week after the rash appeared. This research, published in the American Journal of Ophthalmology, also showed that eyes affected by uveitis were more likely to experience additional ocular complications and vision loss.
 |
In this retrospective, cohort study, which included individuals with acute herpes zoster ophthalmicus, investigators sought to determine the timing of uveitis onset as well as the frequency of associated complications.
The primary outcomes measures included the proportion of individuals who developed uveitis and the time to uveitis diagnosis after HZO onset. Secondary outcome measures were the complications associated with HZO-related uveitis and the impact of early antiviral treatment (within 72 hours) on outcomes.
Of the 869 study participants, 413 (47.6 percent) developed uveitis. Data showed that the median time from onset of rash to uveitis diagnosis was 10 days. Among the 658 patients examined within the first week following rash appearance, 17.6 percent (116/658) were diagnosed at that initial presenting exam and an additional 24.9 percent (164/658) received a diagnosis at a subsequent visit.
Complications, including moderate or severe vision loss, corneal scarring, neurotrophic keratitis, band keratopathy, corneal melt, elevated intraocular pressure, glaucoma and cataract, were higher in eyes with uveitis. Prompt antiviral treatment was correlated with a lower rate of moderate vision loss among patients with the condition, according to the researchers.
“In summary, uveitis is a common complication of herpes zoster ophthalmicus and is associated with other ocular complications. Prompt antiviral treatment did not appear to prevent onset of uveitis in this cohort but was associated with a lower risk of vision loss in those that did develop uveitis. The diagnosis of uveitis was most frequently made during the second week following the rash onset,” the study authors noted in the AJO paper.
“Individuals examined during the first week after onset of HZO rash may still develop uveitis after that visit, and a follow-up examination within the first month should be considered or they should be warned of the symptoms of uveitis that would prompt a repeat examination,” they concluded.
Am J Ophthalmol. September 19, 2024 [Epub ahead of print].
J Meyer JJ, Liu K, Danesh-Meyer HV, et al.
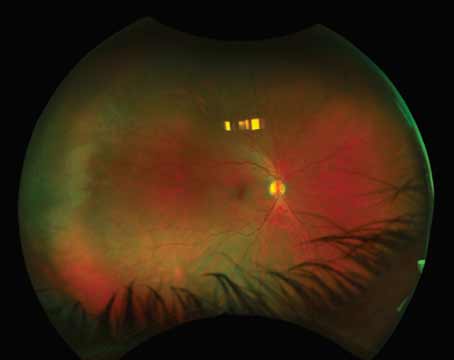
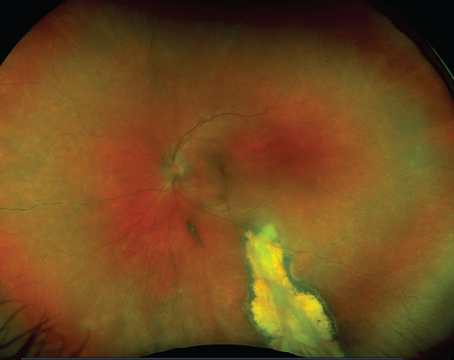
Risk for RD with ARN Studied
Recently published research showed that retinal detachment is a frequent and serious complication of acute retinal necrosis (ARN), influenced by several risk factors such as the extent of initial retinitis involvement and the initial intraocular viral load.
“Active local antiviral therapy may reduce the risk of late-onset RD. The antiviral medication should be adjusted according to the inflammatory state,” the study authors noted. “Therefore, timely detection of causative viruses and intensive systemic and local antiviral therapy is crucial for preserving visual function in acute retinal necrosis patients.”
This retrospective, observational analysis, which examined the risk and prognostic factors that impact the long-term clinical outcomes of ARN, included patients with the condition who underwent treatment and completed follow-up from 2011 to 2021.
Researchers enrolled 59 ARN patients (65 eyes) with an average follow-up of 48.9 months. During the follow-up period, retinal detachment was reported in 34 eyes (52.3 percent). The risk factors for RD included the quadrants of involved retinal necrosis and the initial intraocular viral load. The analysis revealed an independent association between early intravitreal antiviral treatment and a reduced risk of late-onset retinal detachment.
Factors independently linked to an increased risk of final vision loss included poor initial visual acuity and late-onset RD, according to the investigators, who also measured the viral load reduction ratio following the first intravitreal antiviral injection (IAI) and found it strongly correlated with initial intraocular IL-8 concentration and moderately correlated with the initial degree of aqueous flare.
Discussing their research in BMC Ophthalmology, the study authors reiterated that these findings indicated that the initial viral load and the early extent of retinitis were linked to an increased risk of retinal detachment. These factors, they noted, may reflect the severity and progression of the infection, which can lead to retinal necrosis and detachment.
“Our study also showed that late-onset RD may increase the risk of final vision loss related to other factors, such as low initial vision,” the research team wrote. “Therefore, timely detection of viral type and aggressive systemic and local antiviral therapy are crucial for preserving visual function. The shorter interval of IAI application was associated with a reduced risk of late-onset retinal detachment, which suggests that IAI can effectively suppress viral replication and inflammation in the vitreous cavity and prevent further damage to the retina.
“Therefore, eyes with low initial vision and more extensive retinitis or initial viral load at high risk of RD may require closer monitoring for final vision loss,” the study authors concluded. “In addition, early combined systemic and local antiviral therapy in these high-risk patients may reduce the risk of late-onset retinal detachment and final vision loss.”
BMC Ophthalmol. September 15, 2024 [Epub ahead of print].
Li Y, Chen L, Li P, et al.
The Dermatitis/Keratoconus Connection
The literature on atopic dermatitis explains how this condition is sometimes associated with risk of keratoconus, and that higher incidence rates of keratoconus have been reported in patients with eczema. However, not enough has been reported on potential causal relationships between the two diseases. To further investigate this association, researchers from China recently conducted a Mendelian randomization study.
 |
|
Researchers say that atopic dermatitis may have a causal relationship with keratoconus. (From: Atopic Dermatitis. Copyright 2024, StatPearls Publishing, Used under the Creative Commons License). Photo: O.Chaigasame, MD. |
What is a Mendelian randomization study? According to the researchers, this unique statistical method uses single nucleotide polymorphisms, the most common type of genetic variation in people, to estimate whether there’s a causal relationship between the exposure (atopic dermatitis) and the outcome (keratoconus). This allows investigators to limit the influence of confounders and/or reverse causation that may happen regularly in more common observational studies.
After identifying a total of 22,474 cases for their dataset, the researchers began their analysis. Basically, the researchers plugged their data into a statistical analysis package designed for such purposes. This program made all causal inferences for the relationship between the exposure and outcome, and further strengthened the study by using a host of Mendelian randomization study methods in a two-sample approach. The analysis revealed significant evidence that atopic dermatitis has a causal effect on keratoconus and displayed consistent results to that effect throughout the study. Only after performing a reverse Mendelian randomization analysis did the researchers discover that keratoconus does not have a causal effect on eczema.
“We recommend that individuals with atopic dermatitis undergo regular ophthalmic examinations, such as corneal thickness and cornea topography, to detect any early signs of keratoconus,” suggested the researchers in their study, published recently in Translational Vision Science & Technology. “Especially for young patients, receiving ophthalmic examinations and treatment upon the diagnosis of atopic dermatitis can help to prevent permanent ocular damage threatening vision.”
In their paper, the researchers cite evidence in previous studies suggesting that some combination of eye rubbing, systemic inflammation and genetic factors present in those with atopy conspire to induce corneal shape changes characteristic of keratoconus.
There were some limitations that may have skewed the results in this study. The researchers cited that their dataset didn’t have a diverse population, and that all participants were of European decent. Further genetic data will need to be analyzed in future studies. Additionally, this investigation ruled out possible pleiotropic effects even though they are important to recognize in a clinical setting. They were removed by the Mendelian randomization program during analysis.
“In conclusion, using a two-sample Mendelian randomization approach, our study strongly supported previous observational studies suggesting that atopic dermatitis has unidirectional causal effects on keratoconus,” concluded the researchers in their paper on the study.
Ophthalmol Retina 2024; Apr 24. [Epub ahead of print].
Abbasgholizadeh R, Habibi A, Emamverdi M, et al.