Though LASIK is still the most popular refractive surgery for clinical investigators to research, this year's ARVO meeting offers a potpourri of other refractive surgery abstracts that look at many other facets of correcting refractive errors. These run the gamut from preop tips to handling steroid-induced glaucoma post-LASIK. For a look at what's hot this year in refractive surgery, read on.
LASIK
In a small, prospective, randomized, double-masked pilot study from London, researchers say that, at least in average patients, current wavefront-guided LASIK algorithms don't provide a significant benefit over conventional ones.
The researchers randomized 24 eyes of 12 patients to receive either conventional LASIK (preop spherical equivalent: -4.86 D) or wavefront-guided LASIK (preop spherical equivalent: -5.08 D) using the Visx Star S4 laser with version 3.1 software.
At three months, all eyes achieved an uncorrected acuity of 20/20 or better with no loss of lines of best-corrected vision or significant differences in logMAR acuity or Pelli-Robson contrast scores. However, the manifest spherical equivalent refraction for the conventional group (-0.28 D) was significantly lower than that of the wavefront group (-0.55 D; p<0.05). At three months, total root mean square error, vertical and horizontal coma, trefoil and spherical aberration values weren't significantly different between the two groups.1101
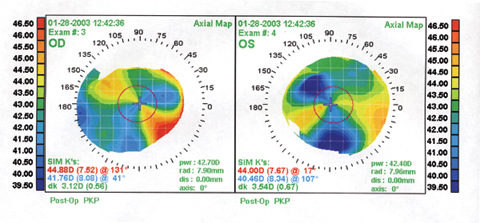 |
| Physicians from New York say that bilateral LASIK can be helpful in treating bilateral PK patients. In the study, the patients' average pre-LASIK sphere was -4.15 D, with an average cylinder of -3.15 D. Shown here is a PK patient's topography just before his LASIK. |
Using the same patients, the British researchers also looked at their visual performance in different lighting and contrast conditions.
Two of the study's 12 patients didn't make the last follow-up visit so the doctors reported on 20 eyes of 10 of the patients.
The physicians say that both groups showed a statistically significant increase in photopic and mesopic contrast-acuity thresholds at one month, but this reduction in visual performance was no longer significant by the third month.
Photopic and mesopic contrast acuity thresholds, along with Pelli-Robson scores, revealed no difference in visual performance between the wavefront and conventional treatment groups, at either one or three months. Unlike the contrast acuity assessment test, pre- and postoperative Pelli-Robson scores did not reveal any significant change in visual performance over time.202
Korean researchers, however, say that wavefront-guided LASIK treatments result in less decrease in functional vision compared to conventional treatments for at least the first six months postop.
In the study, the doctors analyzed 96 eyes of 52 patients. Forty-six eyes of 25 patients underwent wavefront-guided LASIK, and the remainder had conventional treatments. The researchers measured patients' acuity, glare disability and contrast sensitivity each month for six months.
Differences in glare disability and contrast sensitivity showed a statistical significance between the two groups until six months, with wavefront patients having less decrease in function when compared to preop levels and to conventional patients (p<0.05). Wavefront patients had better visual acuity for the first three months, but both groups were similar by six months.1102
Researchers from the University of Rochester performed a study to help estimate the extra tissue necessary to correct higher-order aberrations in order to assist other surgeons in selecting patients.
In their study, the researchers calculated an ablation thickness profile to correct various higher-order aberrations, in addition to defocus and astigmatism, based on the eye's aberrations and the refractive index of the cornea. They then used this profile to calculate the maximum ablation thickness and volume of the total ablation with and without higher-order aberration correction. They measured aberrations in a pre-LASIK population of 208 myopic eyes (mean: -3.35 D sphere, -1.01 D cylinder) and 36 hyperopic eyes (mean: +2.7 D sphere, -0.88 D cylinder). The average higher-order RMS value in the myopic and hyperopic groups was 0.41 µm and 0.48 µm, respectively, for a 6-mm pupil. The surgeons used a 6-mm optical zone with no transition zone.
After surgery, in both groups the maximum ablation thickness when correcting higher-order aberrations was, on average, 2.5 µm larger than without higher-order correction. Total ablation volume was significantly increased when correcting higher-order aberrations through the 4th order compared to when correcting only 2nd-order aberrations. The increase in ablation volume for myopic and hyperopic customized corrections through the 4th order was 0.097 mm3 (an incease of 13 percent) and 0.046 mm3 (a 10-percent increase), respectively. In both groups, there was no significant difference between correcting through the 4th order or 5th order.
The researchers say that, though there isn't a significant increase in maximum ablation thickness in wavefront ablations compared to conventional ones, the total ablation volume increases significantly. This increase in volume in myopic custom ablations is approximately twice as large as that for hyperopic ones. The study doctors say this disparity is mainly due to increases caused by correcting trefoil and coma.222
Physicians from Westchester Medical Center in Valhalla, N.Y., say that bilateral LASIK can be effective in patients who have undergone bilateral penetrating keratoplasty for keratoconus.
Two years following PK, eight eyes of four patients underwent LASIK using the Visx Star S3 to correct their residual refractive error. The average spherical error was -4.15 D (range: -10 D to +0.75 D), and the average cylinder was -3.15 D (range: -1.75 D to -4.5 D). Mean keratometry was 45.4. The uncorrected acuity averaged 20/320. Best-corrected acuity averaged 20/22. The surgeons used the cycloplegic refraction as the target, and separated the surgeries of the two eyes of each patient by three weeks. One eye had a buttonhole during surgery and didn't undergo an ablation; the patient had no complications from the buttonhole, however.
 |
With an average follow-up of six months, the mean postop refraction in the remaining seven eyes was +0.53 D (range: -0.5 to +1.75 D). Uncorrected vision averaged 20/23, with the worst being 20/25. Best-corrected acuity improved slightly to 20/21, and no one lost any lines of acuity.228
LASEK
A team of researchers from Saudi Arabia compared laser epithelial keratomileusis to LASIK and found some trade-offs with each.
The doctors performed LASEK on 86 eyes with a preop spherical equivalent ranging from -1 D to -13.75 D. Sixty-one eyes with errors ranging from -0.75 D to -17.35 D underwent LASIK. They used the Bausch & Lomb Keracor 217Z laser.
Seventy-one (83 percent) of the LASEK eyes were within 1 D of their target refraction, and 16 (19 percent) were within 0.5 D. Fifty-one eyes (59 percent) saw 20/20 or better uncorrected, and 71 (83 percent) saw better than 20/30. Two eyes (2.3 percent) had mild haze. Nineteen percent of the patients reported severe pain on the first day postop, but there was no loss of corneal sensation or contrast sensitivity when compared to preop levels.
In the LASIK group, 56 eyes (92 percent) were within 1 D of their target and 26 (43 percent) were within 0.5 D. Forty-one eyes (67 percent) saw 20/20 or better uncorrected, and 56 (92 percent) saw at least 20/30. The researchers say the differences in acuity values between LASIK and LASEK weren't statistically significant. Though the LASIK group had no haze or pain, they did have decreases in corneal sensation and contrast sensitivity compared to preop.1106
A group of German researchers found no difference between LASEK and PRK for high myopia other than a reduction in postop pain with LASEK.
In the study, surgeons performed PRK on 45 eyes with a mean spherical equivalent refraction of -7.6 D (range: -6 D to -15.4 D). Forty eyes with a mean error of -7.4 D (range: -6 D to -14.25 D) underwent LASEK. The surgeons used either the Schwind Keratom MultiScan laser or the Schwind Esiris.
The researchers found no advantage to LASEK in terms of faster visual rehabilitation or reduced haze. Though the study doctors didn't give actual numerical data, they say that predictability and uncorrected and best-corrected vision were comparable between the two groups. They postulate that their low level of haze with PRK, when compared to the more hazy PRK results of years ago, may be related to the postop drug regimen and the homogenous beam profiles of more modern excimer lasers. The LASEK patients tended to have less pain in the initial postop period, however.170
Preliminary data from Ioannis Pallikaris, MD, and his colleagues in Greece shows that their variant on LASEK, epi-LASIK, is safe and effective for myopia up to -7 D.
The epi-LASIK procedure involves using a special instrument, the Centurion Epikeratome (CIBA Vision Surgical, Duluth, Ga.) to mechanically separate an epithelial sheet from the cornea. Dr. Pallikaris developed the device to avoid using alcohol, which some doctors think is too toxic to the corneal cells. The procedure also avoids the deep lamellar cut performed in LASIK, and therefore may help decrease the chance for ectasia. The exposed bed is then ablated and the epithelial sheet repositioned on the cornea.
In the study, 44 eyes of 32 patients underwent epi-LASIK. Another fifty-one eyes of 40 patients had their epithelial sheets excised for histologic evaluation, effectively converting their procedures to PRK. The preop error of the epi-LASIK group ranged from -1.75 D to -7 D.
In the epi-LASIK group, epithelial healing was complete in 4.87 days, and the mean uncorrected acuity on the day of reepithelialization was 20/32. The patients' spherical equivalent averaged -0.33 D at one month and -0.21 D at three months. Seven eyes (30 percent) gained one to two lines of best-corrected acuity by three months and all the eyes had clear corneas. The researchers didn't compare the epi-LASIK results to PRK, however.
Histological evaluation of three separated epithelial sheets showed a normal stratification and a high percentage of morphologically viable epithelial cells. Some of the surgeons in this study have a financial interest in either CIBA Vision or the Centurion device.4898
Making a Flap
Surgeons from Spain say that, in their small, prospective study, the quality of the flaps created with the Moria M2 microkeratome (Moria, France) was better than that of flaps created with Bausch & Lomb's Hansatome or the older Bausch & Lomb Automated Corneal Shaper, according to confocal microscopy.
The surgeons performed two studies. Study 1 was a prospective analysis using confocal microscopy data from two groups: Group A (control) consisted of 20 non-operated eyes of 20 healthy volunteers; and Group B, 50 eyes of 30 patients operated on with the ACS. Study 2 was a prospective, randomized, double-masked study in which 40 eyes of 20 patients underwent myopic LASIK. The right and left eyes of each patient were randomly and alternatively assigned to two groups: Group C, which consisted of flaps made with the Hansatome; and Group D, which consisted of flaps made with the Moria M2. One month postoperatively, the researchers evaluated the patients' flap thicknesses and interface particle density.
The depth of the cuts made by the three microkeratomes was significantly different, with the ACS flaps being thinner than those made with the Hansatome or the M2. Overall, the researchers say that confocal microscopy showed that the quality of the cuts made by the M2 was better than those of the other two keratomes.194
A research team composed of doctors from Ohio State University and the Institute for Ocular Microsurgery in Barcelona, Spain, say that where you place the LASIK hinge will determine the type of aberrations the flap induces.
The researchers used a Moria M2 microkeratome to create a superior-nasal hinge in one eye and a superior-temporal hinge in the fellow eye. They then studied the topographic and wavefront patterns.
The creation of the LASIK flap produced a significant increase in vertical coma. The orientation of this vertical coma relative to the vertical axis depended on whether the hinge was nasal or temporal. There was also the indication of central flattening, or hyperopic shift, represented by the decrease in magnitude of 2nd-order defocus. The researchers say this information, especially the orientation of the oblique coma relative to hinge position, may help in planning customized ablations in the future.208
Postop Problems
Researchers at the University of Rochester have correlated the higher-order aberrations of patients with irregular corneas with their corneal topographic appearances.
The doctors measured postop wave aberrations for 33 symptomatic postop LASIK and/or PRK eyes. They averaged these measurements across patients with similar topographic diagnoses (central islands, decentered ablations, a new group they termed "baby bow ties," and irregularly shaped corneas) and compared them with 46 preop and successful postop LASIK eyes.
The average higher-order RMS wavefront error (3rd, 4th and 5th orders) for the symptomatic patients was 1.31, and was significantly elevated relative to both normal preop and successful postop LASIK eyes over a 6-mm pupil. Higher-order RMS wavefront error increased with pupil size, roughly doubling for each millimeter of increasing pupil diameter.
On average, eyes that had central islands (n=6) also had the most vertical coma (mean: -1.35 D) while eyes with decentered ablations (n=2) had the most horizontal coma (mean: -0.93 D). Both groups had elevated spherical aberration compared with other symptomatic patients and successful post-LASIK eyes. Eyes with a central topographic "baby bow tie" had the most secondary astigmatism (See figure).
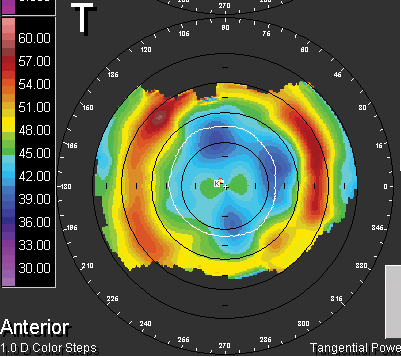 |
| In correlating higher-order aberrations of symptomatic patients post-LASIK, those with secondary astigmatism showed this "baby bow tie" appearance.218 |
In 10 symptomatic patients with bilateral laser refractive surgery, there was significant mirror symmetry between higher order Zernike terms in the fellow eyes, which the researchers say suggests a non-random reason for their undesirable outcomes. Also, the doctors say that, since pachymetry in 14 symptomatic eyes revealed an intense correlation between corneal thickness and higher-order RMS value, low residual corneal thickness may be a predictor of increased higher-order RMS wavefront error.218
Corneal specialists at Philadelphia's Wills Eye Hospital looked at the types of postop LASIK problems that drive unhappy patients to their clinic for help. They say that the results show not only what complaints surgeons can expect to come through their doors, but also reveal the level of these patients' unhappiness.
The physicians reviewed the charts of 156 consecutive patients referred to the Wills Cornea Service between July 1996 and June 2003. Only 32 percent of the patients were referred by their surgeons. Twenty-eight percent were self-referred and 40 percent were referred by another doctor.
The most common diagnosis was irregular astigmatism, found in 49 percent of cases, followed by undercorrection or regression in 17 percent and anterior basement membrane dystrophy, epithelial defects or recurrent erosions in another 17 percent. Less common complications were ectasia in 7 percent and corneal ulcers in 1.24 percent.
The researchers say that almost 70 percent of the cases could be managed with conservative medical therapy. Thirty-five percent were offered contact lenses to wear and 22 percent were recommended spectacles. Penetrating keratoplasty was recommended in 5 percent of the cases.
The researchers note that, since only a third of the patients were referred by their actual surgeons, many of the patients were actually unhappy enough with their surgeons to seek an additional opinion.225
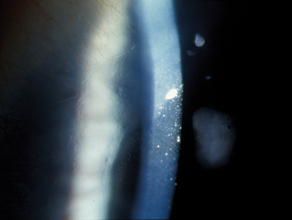 |
| This patient developed what may be the first reported case of Salzmann's-like nodular dystrophy post LASIK.4879 |
In their paper, they report on 20 eyes of 10 patients who had a loss of visual acuity within the first three weeks of uneventful LASIK surgery, after receiving topical steroids postop. The IOPs increased by 4-30 mmHg between postop day four and 20 and all eyes had a decrease in uncorrected and/or best-corrected acuity. All flaps except one had edema without evidence of inflammation in the interface or the rest of the cornea.
The doctors discontinued the steroids and started the patients on antiglaucoma medication, which decreased the IOPs to normal levels and brought about recovery of uncorrected and best-corrected vision. The change in spherical equivalent between the time of maximum IOP and after recovery of normal IOP was between zero and 2.34 D (mean: 1 D). The researchers found a highly statistically significant correlation between the net reduction of IOP and the absolute change in spherical-equivalent refraction.
Though steroid-induced glaucoma is a risk after LASIK, the surgeons say that rapid diagnosis and treatment can recover the vision that's lost.1105
Surgeons from the Moran Eye Center in Salt Lake City report what they believe are the first recorded cases of Salzmann's nodular-like dystrophy following LASIK.
They say that two female patients were referred to the cornea clinic for evaluation of multiple bilateral nodular lesions situated at the site of their LASIK flap margins. Both patients had undergone LASIK in the past year.
The lesions were raised and bluish-white in appearance, and resulted in ocular surface irritation and induction of irregular astigmatism with an associated loss of best-corrected vision. Though neither patient had a significant past medical history, both described a past ocular history of dry eye and subsequent contact lens intolerance. Neither admitted to regularly using ocular lubrication post-LASIK. After an aggressive regimen of topical lubricants, the symptoms resolved. Unfortunately, neither patient opted for lesion removal for histopathological confirmation.4879
Phakic Lenses
According to Spanish researchers, if you plan to implant anterior chamber phakic lenses such as the Artisan (Ophtec, the Netherlands), you should ensure that the lens has adequate endothelial clearance in the corneal periphery, and be prepared to follow Artisan patients closely.
The study is a retrospective review of 110 eyes that received Artisan lenses between 1998 and 2002 (15 for myopia and 95 for hyperopia). The mean follow-up was 21 months. The doctors measured anterior chamber depth, minimum optic-endothelium distance, anterior chamber angle and endothelial cell counts.
Over a period of five years, there was a 29-percent decrease in the number of endothelial cells in hyperopes and an 18-percent decrease in myopes in the first year, and 9 percent per year in the next two years. The researchers say that peripherally shallow chambers seem to be a decisive factor in the cell loss in hyperopes. They recommend long-term follow-up in these patients.337
Dr. Hannush is attending surgeon on the Cornea Service at Wills Eye Hospital, and assistant professor of Ophthalmology at Jefferson Medical College in Philadelphia.



