Presentation
An 11-year-old African-American male presented to the pediatric ophthalmologist with a chief complaint of headache and blurred vision for two weeks. The headache was concentrated around his right forehead and the right side of his neck. His father noted that he had recent deterioration in his handwriting and trouble recalling recent events.
Two weeks prior to presentation, the patient presented to his pediatrician with a headache. He was started on amoxicillin for presumed sinusitis. Two days later his father brought him to an emergency room for nausea and vomiting. The ER team felt he had an allergic reaction to the antibiotic, so they switched his treatment to cefuroxime and added a muscle relaxant for pain control. Over the course of the next 10 days, he developed progressive blurry vision in both eyes. He returned to the ER where a CT scan of the head was unremarkable. He was referred to a pediatric ophthalmologist for further evaluation.
Medical History
The patient was born at full term after an uneventful pregnancy. He had no prior hospitalizations or surgeries and his immunizations were up to date. His medications only included those prescribed in the ER, cyclobenzaprine and cefuroxime. He weighed 65.8 kg, giving him a high body mass index (BMI) of 29. His family history was negative for heart attack, stroke, malignancy, coagulopathy or collagen vascular disease. Review of systems was negative for fever, chills, weight loss or gain, rash, bruising, respiratory congestion, cough, gastrointestinal disturbance and sick contacts.
Examination
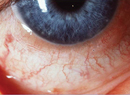
On initial pediatric ophthalmology examination, his vision was hand motions OD and counting fingers at 5 feet OS, with no improvement on pinhole. His pupils were 6 mm and sluggish to light on the right and 4 mm and brisk on the left, with a relative afferent pupillary defect on the right. His extraocular motility was full, finger tension was normal in both eyes, and a quick retinoscopic refraction demonstrated +5 D sphere OD and +1 D sphere OS. Slit lamp exam was unremarkable, but funduscopic exam showed papilledema with hemorrhage and exudates extending into the macula of each eye (See Figure 1a and 1b).
Diagnosis, Workup and Treatment
Differential diagnosis for a previously healthy boy with headache and visually significant papilledema includes elevated intracranial pressure due to a mass lesion, central nervous system infection, venous sinus thrombosis or idiopathic intracranial hypertension. Meningitis was considered, given the neck pain and behavioral change. He had no known history of malignancy or trauma to predispose him to venous thrombosis. His overweight BMI was consistent with idiopathic intracranial hypertension.
The ophthalmologist sent him to the ER for immediate MRI with venography. The study showed a central venous thrombus in the posterior portion of the superior sagittal sinus with no accompanying infarct or bleed (See Figure 2). The neurosurgical team subsequently performed a lumbar puncture. The opening pressure was high at 45 cm H20, and clear cerebrospinal fluid was obtained for analysis. The patient received diamox 250 mg IV and decadron 4 mg IV every six hours overnight until a lumboperitoneal shunt was placed the following morning in the operating room. Once the shunt was in place, he was started on lovenox 1mg/kg SQ b.i.d.
On two-week follow-up examination, the patient's vision improved to 20/400 OD and 20/80 OS. Laboratory evaluation of hypercoagulability by the hematologist revealed elevated factor VIII at 666 (normal 62 to 300), elevated plasminogen at 17 (normal 8 to 14), elevated lipoprotein A at 216 (normal <75) and low protein C at 49 (normal 70 to 180). Other studies were normal, including factor V Leiden, factor 2 mutation, beta2 glycoprotein, C3, C4, ANA, RF, SSA, SSB, SM, RNP-Ab, cardiolipin IgG, IgM and IgA, antithrombin III and protein S. At one month, vision had improved to 20/200 OD and 20/40 OS. Funduscopic exam revealed resolving optic disc edema and macular exudates (See Figure 3a and 3b).
Discussion
Cerebral venous thrombosis is a rare condition that can occur at any age. Improved imaging modalities, including MRI with venography have greatly aided in the identification of CVT. Presenting symptoms commonly include headache, decreased level of consciousness, cognitive deficits, focal neurologic signs and seizure. While headache is the most common presenting symptom, neuro-ophthalmic manifestations include papilledema, esodeviation, transient visual obscuration and vision loss.
Based on the Canadian Pediatric Ischemic Stroke Registry, the annual incidence of CVT is 0.67/100,000.1 Among the 160 identified cases, 18 percent presented with visual impairment and 22 percent were found to have papilledema. Of note, CT failed to make the diagnosis of CVT in 17 percent of cases in which both CT and MRI were performed. Similarly, in our case CT did not reveal the CVT. In another series of 20 cases of CVT with papilledema, visual acuity at presentation was 20/30 or better in all but one eye.2 Only two eyes had a final visual acuity of 20/400 or worse.
The patient in this case suffered diffuse neurologic symptoms (headache, vomiting and papilledema), and his MRI did not show any signs of infarction or hemorrhagic transformation. His profound visual loss at presentation could be attributed to papilledema with with exudates tracking into the fovea. Fortunately, as the disc edema and macular exudates improved, so did his vision.
Known risk factors for CVT include prothrombotic states, both hereditary and acquired, and other conditions associated with hypercoaguability, including collagen vascular diseases, malignancy, oral contraceptive use and pregnancy. The most common prothrombotic conditions include deficiency of protein C, protein S, or antithrombin III, the presence of Factor V Leiden mutation, prothrombin mutation, hyperhomocysteinemia and antiphospholipid antibody. In addition, compressive mass lesions, trauma and surgery can lead to CVT. Among children in particular, head and neck infection, dehydration, malignancy and chemotherapy are associated with CVT. Our case represents a rare protein C deficiency presenting with acute, progressive visual deterioration and CVT.
Several small-scale studies have shown anticoagulation therapy to be safe and effective in resolving the thrombus. A randomized trial of 20 patients with CVT comparing heparin to placebo was discontinued after three months because of better rates of recovery with heparin.3 A second study randomized 59 patients to nadroparin, a low molecular weight heparin (LMWH), versus placebo and found fewer poor outcomes (13 percent versus 20 percent) in the treatment arm. Based on these small trials, it is standard practice to start anticoagulation in the acute phase with heparin or LMWH followed by oral anticoagulation for three to six months.4 A less-established treatment is direct infusion of a fibrinolytic agent via transfemoral venography. Given the lack of quality data, this practice is largely reserved for patients who deteriorate despite anticoagulation therapy.5,6
In addition to anticoagulation, patients are treated for intracranial hypertension. Venous pressure increases with thrombus formation, which can lead to cerebral edema and hemorrhage. Increased venous pressure impairs CSF absorption, which further contributes to increased intracranial pressure.7 Intracranial hypertension is initially relieved with a diagnostic and therapeutic lumbar puncture, followed by possible treatments such as oral acetazolamide, lumboperitoneal shunt and optic nerve sheath fenestration.
The majority of children treated for CVT have no long-term neurologic defects, but some are left with motor impairment, cognitive deficits, developmental delay and visual disturbance.8,9 Seizure and infarction are predictors of persistent neurologic deficits, while older age and the use of anticoagulation therapy predict positive cognitive outcome.10 Therefore, a high index of suspicion and improved imaging modalities may lead to early diagnosis of CVT, providing the opportunity for anticoagulation therapy and better outcomes.
The authors would like to thank Barry Wasserman, MD, for his dedication to resident education and his guidance in the preparation of this case report.
1. deVeber G, Andrew M, Adams C, et al. Cerebral sinovenous thrombosis in children. N Engl J Med 2001;345:417-423.
2. Purvin VA, Trobe JD, Kosmorsky G. Neuro-ophthalmic features of cerebral venous obstruction. Arch Neurol 1995;52:880.
3. Einhaupl KM, Villringer A, Meister W, et al. Heparin treatment in sinus venous thrombosis. Lancet 1991;338:597.
4. Albers GW, Amarenco P, Easton JD, et al. Antithrombotic and thrombolytic therapy for ischemic stroke. Chest 2001;119:Suppl 1:300S-320S.
5. Horowitz M, Purdy P, Unwin H, et al. Treatment of dural sinus thrombosis using selective catheterization and urokinase. Ann Neurol 1995;38:58-67.
6. Griesemer DA, Theodorou AA, Berg RA, et al. Local fibrinolysis in cerebral venous thrombosis. Pediatr Neurol 1994;10:78-80.
7. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005;352:1791-1798.
8. De Schryver EL, Blom I, Braun KP, et al. Long-term prognosis of cerebral venous sinus thrombosis in childhood. Dev Med Child Neurol 2004;46:514-9.
9. Buccino G, Cossu G, De Fanti A, et al. Cerebral venous sinus thrombosis in childhood: Clinical aspects and neurologic and cognitive long-term outcome in three cases. Neurol Sci 2004 Dec;25(5):296-300.
10. Sébire G, Tabarki B, Saunders DE, et al. Cerebral venous sinus thrombosis in children: Risk factors, presentation, diagnosis and outcome. Brain 2005 Mar;128(Pt 3):477-89.