TECs can enhance a practice by drawing in new clientele who are frustrated by the lack of effective dry-eye resources. Furthermore, TEC networks can gather considerable specialized data about the frequency and severity of dry-eye signs and symptoms, their triggers, and the quality of life of patients, all of which are essential to the effort to develop a standard set of effective diagnostic tools. Finally, seeing patients sequentially with similar conditions allows for novel observations regarding dry-eye's characteristics.
A clinical practice will need to have five components in place to establish an effective Dry Eye TEC:
• appropriate patient selection and outreach;
• advanced and varied diagnostic techniques;
• a complete arsenal of treatments available to treat dry-eye disease;
• a nurse or technician who understands dry eye to serve as a sympathetic advocate who can spend time discussing dry-eye management with patients; and
• comprehensive and comprehensible dry-eye literature.
Patient selection and outreach can begin with the clinician's own patients, but the potential patients who can be targeted as TEC clients extend far beyond those.
For example, a recent study found that 43 percent of soft contact lens wearers experienced dry-eye symptoms, compared to 15 percent of non-contact lens wearers who experienced them.1 LASIK and other refractive surgery patients commonly experience dry-eye symptoms.2 Refractive procedures disrupt the enervation of the cornea, resulting in reduced corneal sensitivity, decreased tear production and stability, and decreased blink rate until recovery approximately six months after surgery, and sometimes longer.3,4
Patients with autoimmune diseases such as diabetes, Sjögren's syndrome, rheumatoid arthritis, scleroderma and lupus may also experience dry eye.5 Pamphlets in the offices of internal medicine, autoimmune and endocrine physicians can inform patients who are at high risk for dry eye that resources are available.
Dry Eye TECs also might target individuals at risk for situational dry eye. Visual tasking activities and poor air quality are two situational dry-eye inducers. Media outlets and community-based events can be a way to reach those with less severe dry eye and situational sufferers while also providing an opportunity to generate broader public awareness about the resources and services the TEC provides.
The materials made available to these populations should be of varied media and should be engaging, readily accessible and educational. Posters, pamphlets, websites and in-office videos could explain the lacrimal system, diagnostic tests, how patients can minimize their exposure and maximize their treatment success, and address frequently asked questions such as why a dry-eye patient's eyes might tear excessively. The better informed patients are, the more likely that they will comply with recommended treatment regimens. Patients who understand their dry eye will feel more in control of it.
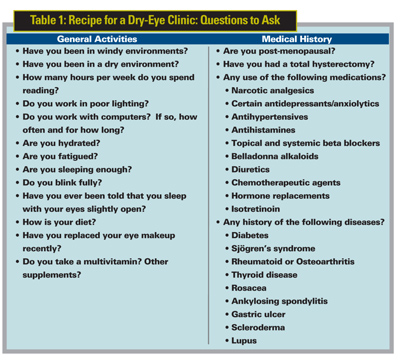
While many diagnostic tests are used for evaluating dry eye, a treatment center should adopt a standard set of tools for diagnosis and detecting changes in severity. First, medical histories should include specific questions about conditions or medications that may contribute to dry eye.6,7 Medications that may be associated with dry eye include blood-pressure medications, antihistamines, decongestants, pain relievers and antidepressants.8
One example of a dry-eye questionnaire is the Dry Eye Investigation (DREI) Study Group's Dry Eye Questionnaire, which queries both symptom frequency and diurnal intensity for patients with aqueous-deficient dry eye.9 Allergan's Ocular Surface Disease Index can assist in identifying exposure factors.10 The Dry Eye Quality of Life Questionnaire, developed by Ophthalmic Research Associates, is another tool that, with further testing, may prove to be valuable. (Pollard S, et al. IOVS 2004;45:ARVO E-Abstract 82) Additionally, these surveys can be used periodically during the course of treatment to monitor improvement. Table 1 shows examples of questions to ask patients.
The clinician should record the patient's visual acuity and a baseline blink rate (number of blinks per minute) prior to any additional or invasive tests. Blink rates will help the clinician know whether blinking provides sufficient protection of the ocular surface.
A slit-lamp exam should be the next step. More advanced cases of dry eye will have redness due to inflammation. Conjunctival redness in these cases should be closely scrutinized and distinguished from the redness of allergy or bacterial conjunctivitis. Clinicians should look for ocular disease hallmarks or dysfunctions that might upset the lacrimal system.
Once the biomicroscopy is complete, the examiner could then perform fluorophotometry to assess the rate at which new tears are produced, which is a precise method for diagnosing tear-deficient dry eye. Schirmer's testing (both Type I and II) also can be used to diagnose tear-deficient dry eye, but fluorophotometry offers the advantages that it captures more accurate data regarding basal tear production without either adding anesthetics (in Schirmer's I) or causing additional reflex tearing (Schirmer's Type II).

Following fluorophotometry, the physician should instill additional fluorescein to measure tear-film breakup time. The tear film forms during blinks and provides protection to the corneal surface by forming a continuous layer of tear.11 Tear-film instability or insufficiency causes the tear film to break prematurely, exposing the ocular surface cells in this area to the air, which can ultimately lead to dry eye.12 TFBUT measures the interval between the last complete blink and the breakup of the tear film, which appears as a black streak, spot or blob on the otherwise confluent fluorescent green tear film.13 Five microliters of 2% unpreserved sodium fluorescein can be used without artificially lengthening the TFBUT.13 Observation of tear-film breakup patterns (TFBUPs), or the pattern in which the tear film separates during TFBUT assessments, is emerging as another method for indicating the underlying cause of the tear-film instability.14
A few minutes after the fluorescein has been instilled, the ophthalmologist can further assess the cornea and conjunctiva. Fluorescein stains epithelial cells that are damaged or desiccated, thus highlighting areas of damage. This staining also might yield significant clues. For example, evidence of inferior punctate keratitis might indicate that the patient does not blink completely,15 or possibly that the patient does not fully close her eyelids when asleep. Lissamine green also allows visualization of areas that have been irritated or damaged by staining cell junctions adjacent to damaged cells in the cornea and conjunctiva.
TEC clinicians can use the TFBUT values and the blink rate to calculate the Ocular Protection Index. The OPI is obtained by dividing the TFBUT by the blink rate (blinks/60 seconds). A TFBUT that is greater than the inter-blink interval (OPI >1) indicates that the tear film completely protects the ocular surface until the next blink. (Ousler GW, et al. IOVS 2002 43: E-Abstract 56) If the TFBUT is shorter than the IBI (OPI <1), the ocular surface will be exposed to the environment until the next blink. An increase in OPI after dry-eye therapy is an endpoint that suggests therapeutic efficacy.
Patients can assess their tear-film breakup time at home with the Symptomatic Non-Invasive Break-Up Test. Patients should be instructed to stare at an object and count the seconds until the first sensation of ocular discomfort. (Pollard S, et al. IOVS 2003;44: E-Abstract 2489) This technique can help patients gain situational awareness of their dry eye.
TEC clinicians may also collect tear samples for osmolarity measurements. This should be done by using a capillary tube, which minimizes the risk of inducing reflex tearing, which can skew the osmolarity assessment. Tear osmolarity is generally higher in patients with dry eye due to evaporation of the tear film and the higher osmolarity of fluid produced by the lacrimal glands.16,17 Increase in tear osmolarity should be addressed with a hypotonic artificial tear, since high osmolarity may be toxic to the epithelium.18
There are many sub-types of dry eye (e.g., lipid deficient, aqueous deficient, mucin deficient, inflammatory), yet over the counter, non-targeted tear substitutes are the mainstay of treatment.19 Systane (Alcon), Soothe (Alimera), and Refresh Liquigel (Allergan) are examples of next-generation artificial tears that have unique properties designed to work with existing tears. Restasis (Allergan) is the only prescription ophthalmic emulsion available for dry eye and may help patients whose dry eye has an inflammatory component.20,21
Use of tear substitutes can help treat the symptoms of dry eye, slow the condition's progression and prevent related ocular surface damage. Just as it's necessary to water a houseplant on a regular basis in order to keep the soil from drying and the plant from dying, the dry-eye patient should use tear substitutes regularly, even when the sensation of dryness is not present, so that discomfort and surface damage can be prevented.
Finally, humidifiers can help combat the dry air that aggravates dry eye, and they may especially be helpful during the colder months when home heating decreases the humidity further. When choosing a humidifier, it's important to find one with an ultraviolet light system that prevents bacterial growth, such as the two-gallon tank humidifier system from Brookstone ($99).
Other options are available for serious cases. Punctal plugs or scarring the tear duct closed by cauterization decreases or stops the passage of the tears into the ducts. For patients who experience meibomian gland dysfunction, daily hot compresses can help clear capped or blocked meibomian glands, allowing the lipid component of their tears to be replenished. A clinician may also suggest meibomian gland expression, a procedure that extracts lipid from the glands to temporarily increase tear-film lipid and prevent evaporation.
It's critical to begin management of dry eye early; most dry eye begins with symptoms, but over time the signs will follow. Effective treatment for dry eye is in high demand, and as the numbers of older people rise, the demand is likely to increase. Easy access to dry-eye education, diagnosis and treatment through a Dry Eye TEC may result in effective treatment and fewer sequelae, however.
A TEC can provide you with experience with the various forms of dry eye and foster treatment strategies, and TECs allow clinicians to test the validity of tests and treatments on a large scale. Also, patients at the TEC may be referred to your practice for other services, such as cataract surgery. Finally, after receiving such thorough care for their dry eye, TEC clients may refer their friends.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Langelier is a clinical research associate at ORA Clinical Research and Development in North Andover.
1. Guillon M, Maissa C. Dry eye symptomology of soft contact lens wearers and nonwearers. Optom Vis Sci 2005;82:9:829-34.
2. Solomon KD, Holzer MP, Sandoval HP. Refractive surgery survey 2001. J Cataract Refract Surg 2002;28:346-55.
3. Benitez-del-Castillo JM, del Rio T, Iradier T, et al. Decrease in tear secretion and corneal sensitivity after laser in situ keratomileusis. Cornea 2001;20:1:2030-32.
4. Lee JB, Ryu CH, Kim J, Kim EK, Kim HB. Comparison of tear secretion and tear film instability after photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg 2000;26:1326-31.
5. Sayjal LP, Lundy DC. Ocular manifestations of autoimmune disease. Am Fam Physician 2002;66:991-8.
6. Welch D, Ousler GW, Nally LA, Abelson MB, Wilcox KA. Ocular drying associated with oral antihistamines (loratadine) in the normal population - an evaluation of exaggerated dose effect. Adv Exp Med Biol 2002;506:1051-1055.
7. Mattox C. Table of Toxicology. In: Albert DM, Jacobiec FA, eds. Principles and Practices of Ophthalmology, vol 1, 2nd Ed. Philadelphia: W.B. Saunders Company:496-507.
8. Ousler GW, Wilcox KA, Gupta G, Abelson MB. An evaluation of the ocular drying effects of 2 systemic antihistamines: loratadine and cetirizine hydrochloride. Annals of Allergy, Asthma and Immunology 2004;93:460-464.
9. Begley CG, Caffery B, Chalmers, RL, Mitchell GL. Dry Eye Investigation (DREI) Study Group: Use of the Dry Eye Questionnaire to measure symptoms of ocular irritation in patients with aqueous tear deficient dry eye. Cornea 2002;21:7:664-670.
10. Allergan OSDI (Ocular Surface Disease Index). 2004. Allergan. Available at: http://www.dryeyeeducation.com/OSDI.pdf. Accessed March 21, 2006.
11. Cho P, Brown B. Reviews of the tear breakup time and a closer look at the tear breakup time of Hong Kong Chinese. Optom Vis Sci 1993;70:1:30-8.
12. Lemp MA. Report of National Eye Institute/ Industry Workshop on clinical trials in dry eyes. CLAO J 1995;21:221-32.
13. Abelson MB, Ousler GW, Nally LA, Welch D, Krenzer K. Alternative reference values for tear-film break-up time in normal and dry eye populations. In: Lacrimal Gland, Tear Film, and Dry Eye Syndromes 3. Sullivan D, ed. New York: Kluwer Academic/Plenum Publishers, 2002.
14. Ousler GW, Lemp MA, Schindelar MR, Abelson MB. Tear film break-up patterns (TFBUP) – a novel method of evaluating tear film stability (abstract). The Ocular Surface 2005;3:S100.
15. Abelson MB, Holly FJ. A tentative mechanism for inferior punctate keratopathy. Am J Ophthalmol 1977;83:6:866-9.
16. Gilbard JP. Tear film osmolarity and keratoconjunctivitis sicca. In: The Preocular Tear Film in Health, Disease and Contact Lens Wear. Holly FJ, ed. Lubbock, Texas: Dry Eye Institute, 1986.
17. Gilbard JP, Dartt DA. Changes in rabbit lacrimal gland fluid osmolarity with flow rate. Invest Ophthalmol Vis Sci 1982;23:250.
18. Gilbard JP, Carter JB, Sang DN, et al. Morphologic effect of hyperosmolarity on rabbit corneal epithelium. Ophthalmology 1984;91:1205.
19. Kunert KS, Tisdale AS, Stern ME, Smith JA, Gipson IK. Analysis of topical cyclosporine treatment of patients with dry eye syndrome: Effect on conjunctival lymphocytes. Arch Ophthalmol 2000;118:11:1489-96.
20. Kunert KS, Tisdale AS, Gipson IK. Goblet cell numbers and epithelial proliferation in the conjunctiva of patients with dry eye syndrome treated with cyclosporine. Arch Ophthalmol 2002;120:3:330-7.
21. Christensen MT, Stein JM, Stone RP, Meadows DL. Evaluations of the effect on tear film break-up time extension by artificial tears in dry eye patients. Presented at: 23rd Biennial Cornea Research Conference, October 3-4, 2003, Boston, MA.



