Every cataract surgeon understands the role the cornea plays in refractive outcomes for their patients. The more pristine, the better measurements can be obtained and the more likely patients will be happy. One condition that can interfere with this process is a pterygium.1 Not all pterygia are created equal, though, and surgeons should consider several factors to determine whether or not to remove one, and when.
“A pterygium is basically scar tissue that can be very small and mild and not really cause much problem at all,” says Christopher J. Rapuano, MD, Chief of Wills Eye Hospital’s Cornea Service. “It can be stable over time, or it can progress slowly, and more so when people are younger and not as much when people are older. Pterygia can sometimes run in families but oftentimes they are related to ultraviolet exposure, chronic trauma, chronic dry eye, and exposure to environmental factors, including sun, wind and sand. They tend to be more common in those who live closer to the equator.”
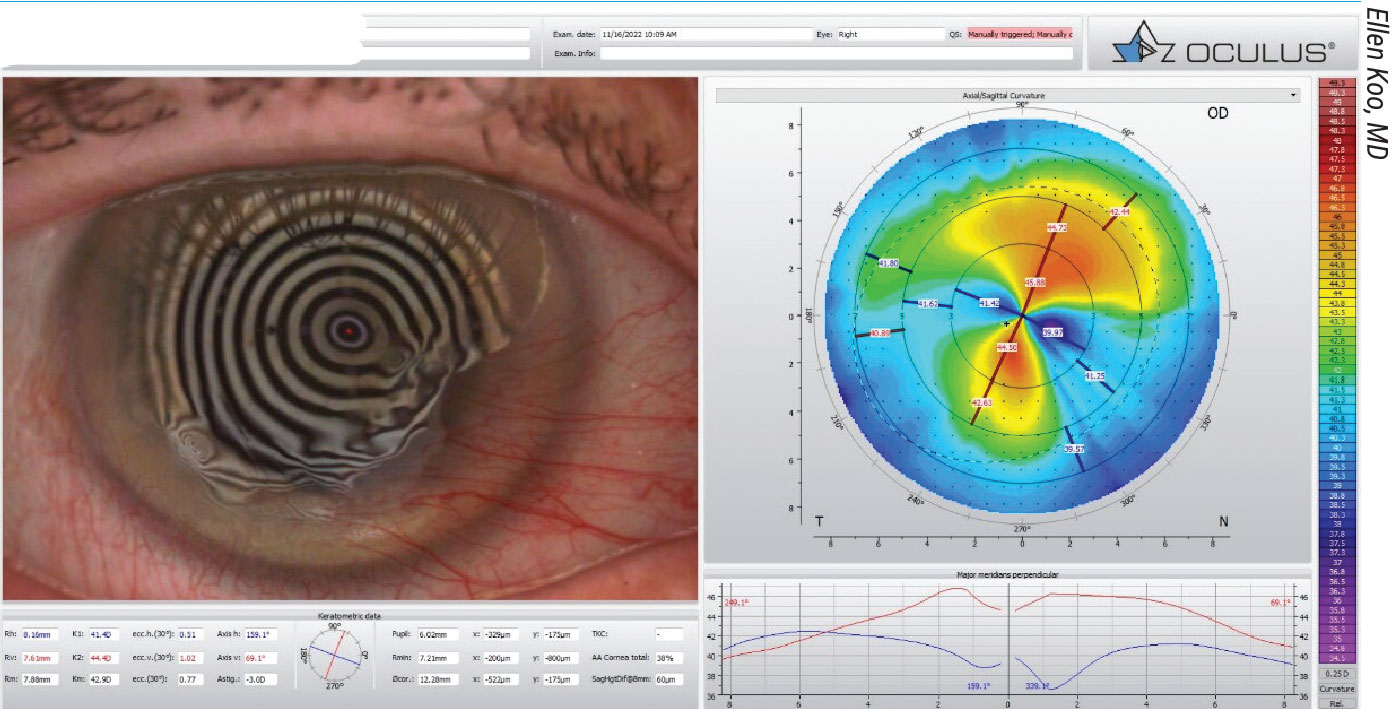 |
|
Topography showing a large nasal pterygium and the resulting irregular astigmatism. |
Pterygia are most commonly found on the nasal side of the eye. “They can be temporal, but they’re usually either at the 3 or the 9 o’clock position and occasionally they can be both nasal and temporal,” continues Dr. Rapuano. “In some severe cases you’ll see nasal and temporal pterygia that connect in the middle. Because they’re elevated, pterygia can cause some irritation and extra dryness, which causes inflammation, redness and irritation. Patients’ eyes will appear red all the time. It can cause discomfort and cosmetically it doesn’t look good.”
Some cornea specialists say a small, asymptomatic pterygium that doesn’t bother the patient could be left alone and may not affect refractive outcomes after the cataract surgery. “Typically, lesions smaller than 3 mm don’t tend to create irregularities of the cornea,” says Ellen Koo, MD, an associate professor of clinical ophthalmology at Bascom Palmer Eye Institute.
However, Dr. Rapuano says it’s important to closely look at corneal curvature before making this decision. “In those who have small pterygia that aren’t causing redness, pain or decreased vision, the question is, should they be removed prior to cataract surgery? And the answer generally is, if it seems to be affecting the corneal curvature, then they should be removed,” he says. “You really want a good, stable, regular corneal curvature for cataract surgery.”
Although larger pterygia are more likely to cause a change in astigmatism, it’s not always about the size of the lesion.
“You can have a smaller pterygium that’s causing more astigmatism than you expected and a larger one that may not be causing much, so we can be a little bit deceived just by the size of it,” says Leela V. Raju, MD, a clinical associate professor at NYU Langone Eye Center. “I don’t believe we generally need a rule of addressing all pterygia before cataract surgery because some can look very fine and thin, and those may not cause as much astigmatism as some of the thicker-looking pterygia. I wouldn’t base it on size, but I would look at how—for lack of a better word—‘beefy’ the pterygium looks. Some that look very thick or red, they might have an increased chance of causing more astigmatism than these very thin ones that you can almost see through at the slit lamp.
“However, if you look at the tomography and it doesn’t show a large amount of astigmatism and it’s not bothering the patient, you could have a discussion about leaving it alone or removing it at the time of cataract surgery, with the understanding that it’s likely we won’t be able to correct all of the astigmatism,” she continues. “Some people are very happy wearing glasses afterwards, and they prefer it in some cases, so make sure that they know their options and make sure you’ve documented the conversation really well.”
Techniques for Removing the Pterygium
Excising pterygia doesn’t prevent them from returning in the future and the chosen surgical technique for removal can impact the recurrence rate.
“The recurrence rate can be as low as 5 percent in the best of hands and in some studies it’s 10 or 15 percent,” says Dr. Rapuano. “The standard technique that most cornea specialists will use is a conjunctival autograft placed in the area where we just removed the pterygium. We’ll use some fibrin glue and oftentimes a few dissolvable sutures to secure it in place. If you do that it has a very low recurrence rate, less than 5 percent.”
Removing Tenon’s fascia is another component of success in this technique, says Dr. Koo. “With the excision, usually we start with the blunt dissection of the lesion and it often peels off without much effort once you find the right plane,” she says. “During the harvest of the conjunctival autograft, it’s important that there’s minimum Tenon’s in the autograft to ensure optimal healing, as well as the cosmesis aspect afterwards. Some people do use the conjunctival pedicle rotation technique, meaning you leave a little pedicle that’s still attached from the harvest site and simply rotate that to the site of excised pterygium. The principle of that is to provide a viable autograft and that’s also a great technique.”
Dr. Raju also uses a conjunctival autograft as her primary technique. “I do a decent amount of Tenon’s resection,” she says. “I think it’s important to remove Tenon’s, even hooking the muscle. Getting the Tenon’s around the edges of the muscle is important.”
An amniotic membrane graft is another technique some choose to perform. “Excision of the lesion with amniotic membrane graft is also considered acceptable, especially in cases where there’s not enough viable conjunctiva or there’s a need for glaucoma surgery, but the recurrence rate for that is thought to be higher than for the technique with a conjunctival autograft,” says Dr. Koo.
In some cases, mitomycin-C could be appropriate, say experts. “Some of the pterygia that I see in New York are in patients who have grown up in much sunnier climates, and their pterygia can look very thick,” Dr. Raju says. “In those primary cases I will use mitomycin-C because they definitely have a higher risk of recurrence, even if you do a really good Tenon’s resection. Otherwise, I generally reserve any mitomycin-C for recurrent pterygia, or if it’s temporal I often do mitomycin-C and maybe even add in amniotic membrane along with a conjunctival autograft because that’s not the regular location for them, which makes me think there’s something else going on. Anything you can do to reduce inflammation after the procedure is going to help make sure that you’ll have better outcomes and less recurrences.”
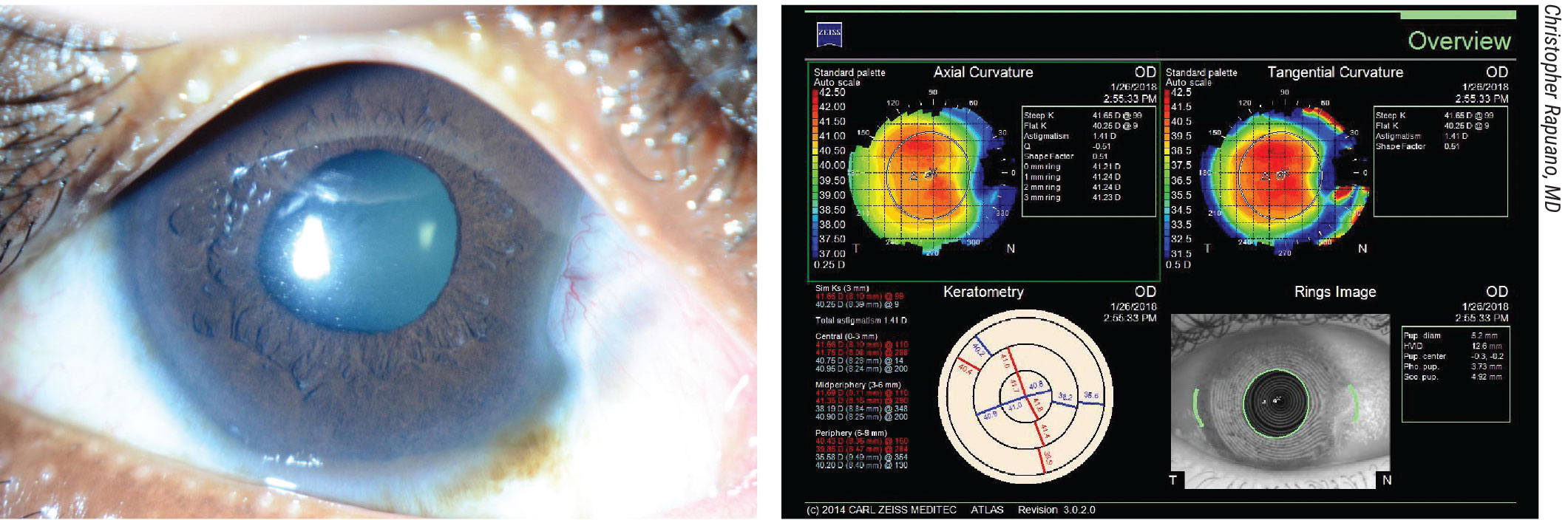 |
|
Slit lamp photograph showing a small- to medium-sized nasal pterygium in the patient’s right eye. He has no visual complaints. Even though the pterygium isn’t very large, corneal topography of the eye demonstrates some irregular astigmatism beginning to reach the visual axis. For the best results after cataract surgery, one should consider removal of this pterygium prior to cataract surgery. |
However, mitomycin-C comes with some risks, adds Dr. Koo. “If using mitomycin-C, you want to limit the concentration to 0.02% and limit the time usage, along with making sure that the ocular surface is flushed really well so that there’s no mitomycin-C remaining,” she says. “Mitomycin-C is associated with a lower recurrence rate, and is very helpful for cases of recurrent pterygia. That said, intraoperative usage of mitomycin-C does carry risks, and these include risks of delayed epithelialization, scleral thinning or even scleral melt.”
Healing and Next Steps
“After surgery, patients are placed on steroids and carefully monitored in the ensuing weeks and we usually wait at least three months before obtaining biometry,” says Dr. Koo. “In that time period, when they’re coming back for their follow ups, I do obtain serial topography because you want to achieve stability at the time of cataract surgery consideration.
“With removal of the pterygium you should see a reversal of that induced corneal astigmatism,” she continues. “There are some instances where the pterygium itself affects the Bowman’s layer and can lead to some level of scarring even after excision. That may be reflected in the final topography, but most of the time we should see marked improvement of the irregular astigmatism. The main goal is to achieve stability and to make sure you can have at least a couple reproducible topographies.”
Dr. Raju looks for agreement in her measurements before proceeding with the cataract surgery. “Hopefully I’ve had measurements that have been agreeing with each other in a two-week period,” she says. “For instance, you could do measurements at four weeks and six weeks, or six and eight weeks after pterygium surgery to see that you’ve got agreement, but once again, I think it’s very important to let the patient know that we really want this to heal up properly so we get the proper measurements to pick the best implant for them.”
Patients who’ve had pterygium removed aren’t necessarily limited in their IOL choices, but there are caveats. “It depends on how normal the curvature is after the pterygium surgery,” says Dr. Rapuano. “If the cornea looks beautiful and perfectly smooth, and they have a low chance of recurrence of the pterygium, then you can pretty much use any IOL power you want. But a lot of these patients have some irregularity of the cornea and some corneal scarring after the pterygium is removed, and their vision might be very good after the cataract surgery but not necessarily perfect. For those patients, a multifocal lens is probably not ideal. If they have a lot of astigmatism because their cornea is still somewhat irregular, then they might do well with a hard contact lens after surgery. You probably don’t want to use a toric lens in some of those patients either because it’s much harder to fit a hard contact lens after a toric IOL. Those would be my main concerns. Again, some patients have a higher chance of recurrence, especially if it’s been a recurrent pterygium to begin with, or if there’s a lot of scar tissue. If there’s a high risk of recurrence, then you may not want to use a multifocal or toric lens because the recurrence will change the shape of the cornea.”
Cornea experts emphasize the ocular surface and if there are any signs of dry eye. “I do think it’s important to address any dry eye with these patients because of the amount of inflammation and solar changes that have led to the pterygium, you may want to be a little more careful in examining their ocular surface to make sure that it’s also not going to skew your keratometry, especially if a patient’s interested in one of these premium technology lenses,” says Dr. Raju. “Pterygium can also affect the tear film, so if a patient is really considering a premium technology implant, make sure you’ve done everything you can to ensure nothing is going to affect the tear film, because we know that can cause problems in patients without pterygium if not addressed appropriately.”
Patient Follow-Up
Moving forward, these patients should be closely followed for any signs of recurrence.
“I say this very often to our residents, it’s so important to remove pterygium appropriately the first time,” Dr. Raju says. “When you have to go back, the surgery becomes much more difficult. That initial technique is really important. We have to truly think about trying to make this a one-and-done type surgery. Not that it’s always possible, but that should be our goal.”
She routinely sees her patients monthly for the first four to six months postop. “I look for any increase in redness and help remind them to use their drops, protect their eyes from sun, wind or dryness, which can also exacerbate irritation and makes us more concerned for recurrence,” says Dr. Raju. “Especially in those really thick pterygia, obviously something has elevated inflammation on the surface for some reason so you have to watch those patients very carefully. I always ask them to come back if they’re noticing any redness after the initial couple of weeks because I’d expect that to have gone down pretty significantly at that point. We’d possibly increase their topical steroids or sometimes I’ll inject steroids subconjunctivally in order to really help target any localized areas of inflammation and hopefully I can prevent it from recurring.”
Drs. Koo and Raju report no relevant disclosures. Dr. Rapuano consults for BioTissue.
1. Sharma B, Bajoria SK, Mishra M, Iqubal N. Refractive outcomes of simultaneous pterygium and cataract surgery with fibrin glue. Cureus 2021;24:13:11.



