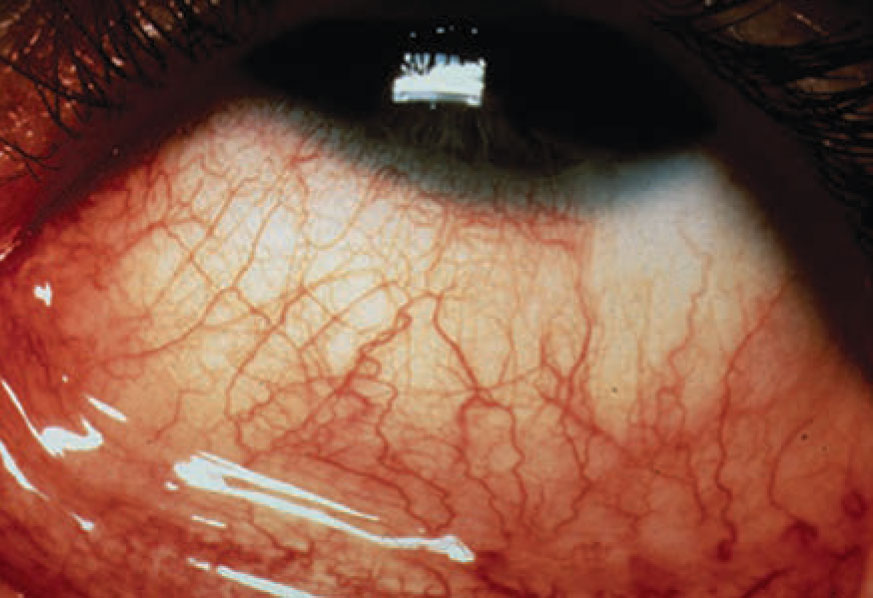
Because the eye is in constant contact with the environment, it is vulnerable to irritants. Allergic conjunctivitis affects approximately 40 percent of the population,1 and treatment involves a comprehensive, stepwise approach, according to experts. Here’s a look at how clinicians approach allergy patients with today’s modalities.
First-line Approaches
 |
|
Working with an allergist can help root out the source of the problem, clinicians note. |
Seasonal allergic conjunctivitis and perennial allergic conjunctivitis are the most common ocular allergies, affecting 15 to 25 percent of the population.1 Atopic keratoconjunctivitis, vernal keratoconjunctivitis and giant papillary conjunctivitis are more severe conditions and more challenging to treat.
Treatment typically begins with nonpharmacological agents, such as cold compresses, and progresses to a variety of topical and oral medications. Of the pharmaceutical agents available, antihistamines, mast cell stabilizers, and dual-action agents are the most common.
Tears are often the initial treatment to rinse allergens from the eye. “When a patient presents to my office with ocular allergy symptoms, I first use refrigerated, preservative-free tears, specifically a watery, non-viscous variety like Refresh Plus,” says Robert Latkany, MD, who is in practice in New York City. “Patients can refrigerate the tears and rinse the eyes with them a few times a day. Patients like the cold drops, and they tolerate them well because they are preservative-free. Any watery, non-viscous, preservative-free drop will work well.”
Antihistamines and Mast Cell Stabilizers
To treat the source of the allergy, however, clinicians usually reach for an antihistamine or a mast cell stabilizer.
Cetirizine ophthalmic solution 0.24% (Zerviate, Eyevance) is the most recent addition to the topical antihistamine armamentarium, having been launched for allergic conjunctivitis last year.2 It’s been approved for b.i.d. dosing.
Single-center and multicenter, double-masked, randomized, vehicle-controlled, parallel group conjunctival allergen challenge studies were conducted over approximately five weeks and four study visits. Approximately 100 people were randomized in each study. Primary endpoints were ocular itching and conjunctival redness 15 minutes and eight hours post-treatment, post-conjunctival allergen challenge.
In the study, cetirizine administered 15 minutes or eight hours prior to conjunctival allergen challenge resulted in significantly lower ocular itching scores compared to vehicle at all time points post-conjunctival allergen challenge. Investigators measured conjunctival redness and found that it was significantly lower after cetirizine treatment compared to vehicle at seven minutes post-conjunctival allergen challenge at both 15 minutes and eight hours post-treatment in both studies. Cetirizine also resulted in significant improvement in chemosis, eyelid swelling, tearing, ciliary redness, and episcleral redness, as well as nasal symptoms after conjunctival allergen challenge. No safety concerns were identified.
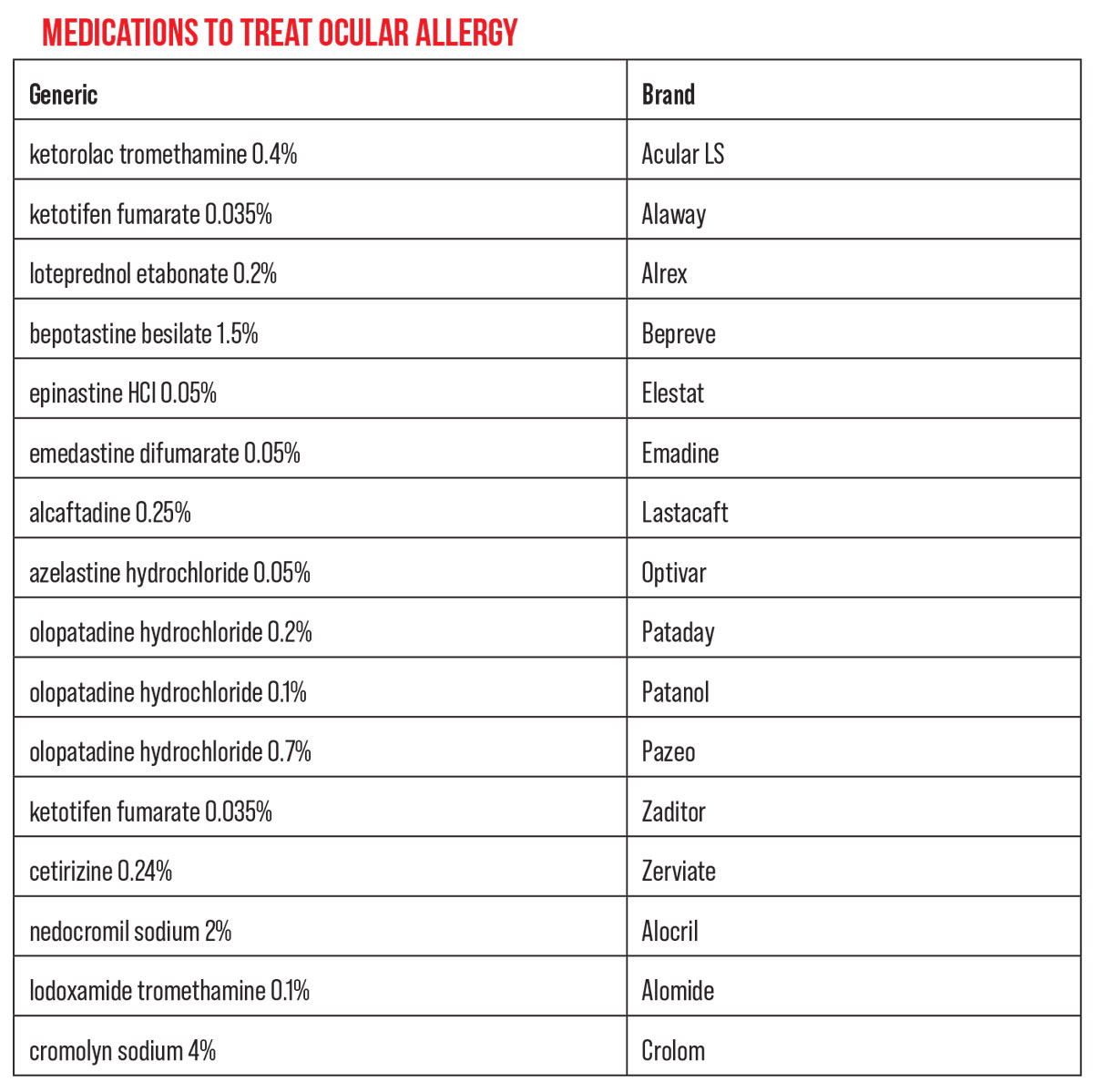
According to Francis Mah, MD, who’s in practice in San Diego, some of the more popular medications in this category now have generic and over-the-counter options. “Alcon has made the decision to put Patanol (0.1% olopatadine), Pataday (0.2% olopatadine) and then Pazeo all over-the-counter under the Pataday name,” he says. “That’s significant because those were the most popular prescriptions that we were writing in eye care, and now they’re all OTC. The other medication that ophthalmologists are writing for is Zerviate, so that’s kind of the last man standing for prescription medications.”
 |
| Click image to enlarge. |
Dr. Latkany agrees. “My favorite of the group is the Pataday Once Daily. “Patients seem to tolerate it well, and there is very little stinging,” he says. “It used to be a popular drop when it was a prescription, but it was often not covered by insurance. Another medication in that category is Bepreve. Others include over-the-counter Zaditor and Lastacaft. Cetirizine is now just a straight antihistamine drop, and some people use cromolyn sodium, which is a nice cheap drop.”
Dr. Mah notes that these topical agents can get the majority of seasonal allergy patients under control. “More than 90 percent of patients can be controlled with artificial tears, avoidance of the allergen, and then using topical antihistamines or mast cell stabilizers,” he says.
If the patient has allergy symptoms that extend beyond the eye, such as rhinitis, post-nasal drip or asthma, Dr. Mah recommends using a systemic medication. “You want to start simple,” he advises. “Allegra is a really good one because it has few systemic side effects, like drowsiness. Zyrtec and Claritin are also great. If a patient has lots of nasal symptoms, Flonase can be added, and you can also add a decongestant. Generally, for me, I tend to go to either Zerviate, which is a prescription, or topical Pazeo, which is OTC. Then, I add Flonase if the patient has a nasal component.”
Steroids
Steroids can be added if the eye is very inflamed or if there are significant ocular issues. “I’m not afraid to give a little steroid now that we have low concentrations of loteprednol,” Dr. Latkany says. “Because loteprednol is not a super-strong steroid, there are fewer side effects. Giving it to the patient for a couple of weeks seems to work better than just going to an antihistamine or mast cell stabilizer combo. If a patient has severe allergies, I might start off with the steroid and switch him or her to an antihistamine/mast cell stabilizer. Other products that I use off-label are in the NSAID category to help with some of the secondary inflammation. Some favorites in that category include Prolensa, BromSite, and Nevanac. I’m not a big fan of any of the generics in that category, but I have had some success with them.”
Patients who have severe cases of atopic keratoconjunctivitis may require a stronger steroid. “I might start off with a stronger steroid, such as prednisolone, and possibly Durezol, if the eye is very inflamed,” Dr. Latkany adds. “Once the eye has been quieted over a few days, I can convert to a less potent drug. In addition to drops, we can also use oral antihistamines for these patients.” Physicians’ steroid regimens usually consist of an initial high dose and then a quick taper.
Involve an Allergist
It’s important to determine the source of the allergy, so it can be helpful to involve an allergist. “Some ophthalmologists do their own testing in their offices to detect what allergens are the source of the patient’s symptoms,” Dr. Latkany explains. “I perform a prick test followed by an intradermal test, if necessary, to detect the specific triggers. If we can determine the source, patients can make lifestyle modifications, such as not allowing the dog or cat in their bed if they are allergic. Or, if a patient is allergic to pollen, he or she could shower before bed to remove any pollen. It’s nice to detect the exact allergen.”
When treating ocular allergy, Dr. Latkany takes a comprehensive approach. “I like to hit the allergy from many angles: cold compresses; cold tears; Pataday; include an allergist; identify the allergen,” he says. “Then, once you know the specific allergen, start with anti-allergy environmental changes, and then consider immunotherapy shots. Some people are even doing sublingual therapy, which includes tricking the immune system into thinking that the patient is not being exposed to something he or she is allergic to.”
Besides environmental allergens, patients can be allergic to products they use on their faces, such as certain moisturizers and cosmetics. “It’s important for patients to bring all face and eye products to an allergist,” says Dr. Latkany. “The allergist can do a patch test on the patient’s back. If the patient is allergic to a product, we want to know that rather than just giving him or her Pataday and a steroid, while they keep using the product. Identifying product sensitivities helps us treat them.”
Patients can also be allergic to medications they’re taking. “Patients can also be allergic to the preservatives in glaucoma drops or be allergic to the medication itself,” notes Dr. Latkany. “It’s important to identify this rather than treating the allergy with medication. In these cases, call the glaucoma doctor and ask if you can switch medications for a week to see if the allergy symptoms get any better. Lastly, contact lenses can cause allergy symptoms. The contact lens or the contact lens solution may be triggering an allergic or chemical sensitivity.”
Dr. Latkany adds that treatment will be much more successful once the source of symptoms is identified. “Take a comprehensive approach and attack the source of the problem rather than the symptom,” he advises.
The Future
Aldeyra has developed an anti-inflammatory drug called reproxalap that has been quite successful in reducing allergic conjunctivitis symptoms. The company announced positive results from a Phase III trial of 0.25% and 0.5% reproxalap topical ophthalmic solution in patients with allergic conjunctivitis. The clinical trial met the primary endpoint and the key secondary endpoint for both concentrations of reproxalap.3
The Phase III trial was a double-masked, randomized, vehicle-controlled, multicenter, parallel-group conjunctival allergen challenge that assessed the efficacy and safety of 0.25% and 0.5% concentrations of reproxalap topical ophthalmic solutions compared to vehicle in 318 patients with seasonal allergic conjunctivitis.
Compared to patients treated with vehicle, patients treated with 0.25% and 0.5% reproxalap experienced a statistically significant reduction in ocular itching. The investigators found that both concentrations of the drug exhibited an anti-inflammatory profile that’s distinct from standard-of-care antihistamine therapy and supports a differentiated mechanism of action for the treatment of allergic conjunctivitis.3
“I think the coolest line of potential topical drugs are the biologics,” says Dr. Mah. “They’re obviously strong anti-inflammatories. Because allergy is an inflammatory condition, I think that would be interesting. However, they haven’t even entered Phase II trials, so it’ll be a while before they are available. Everything else in the pipeline is either a topical antihistamine, a topical antihistamine/mast cell stabilizer, or a topical mast cell stabilizer, and we’ve had these medications for decades.”
While topical ophthalmic solutions are the most convenient treatment, the eye’s anatomy and physiology lead to decreased bioavailability of the drugs. Ocular drug-delivery systems are also being studied to overcome this limitation.
Dr. Mah is a consultant for Novartis, Allergan/Abbvie, Bausch + Lomb, Sun, Kala and Eyevance. Dr. Latkany has no financial interest in any of the products discussed.
1. Kimchi N, Bielory L. The allergic eye: Recommendations about pharmacotherapy and recent therapeutic agents. Current Opinion in Allergy and Clinical Immunology 2020;20:4:414-420.
2. Meier EJ, Torkildsen GL, Bomes PJ, Jasek MC. Phase III trials examining the efficacy of cetirizine ophthalmic solution 0.24% compared to vehicle for the treatment of allergic conjunctivitis in the conjunctival allergen challenge model. Clinical Ophthalmology 2018:12:2617-2628.
3. Aldeyra trial news. https://ir.aldeyra.com/news-releases/news-release-details/aldeyra-therapeutics-announces-positive-top-line-results-phase-3.





