Superior limbic keratoconjunctivitis is a chronic, often underdiagnosed inflammatory condition affecting the superior bulbar conjunctiva adjacent to the limbus. When patients aren’t responding to treatments for dry eye and blepharitis, clinicians should consider SLK. Here, ocular surface experts share how they diagnose and manage this condition.
Presentation
“SLK typically originates from chronic friction between the superior tarsal and bulbar conjunctiva,” explains Sezen Karakus, MD, of the Wilmer Eye Institute at Johns Hopkins. “Patients usually complain of a foreign body sensation that worsens with blinking. This chronic friction may be due to irregularities on the tarsal conjunctiva, such as scars or papillae, or redundant bulbar conjunctiva that moves and causes irritation with every blink.”
Dr. Karakus says that SLK can originate from or be exacerbated by dryness, such as when there’s an inadequate quantity or quality of tears to lubricate conjunctival surfaces in contact. “Conjunctival redundancy, or chalasis, can also stem from chronic friction if it wasn’t the original reason that initiated the irritation,” she says. “Initially, redness may be limited to this area and might not be noticeable unless the upper lid is lifted to examine the region. However, inflammation can spread to the adjacent limbus and superior cornea as the condition worsens, causing epithelial changes, filaments and abrasions. This leads to a worsened foreign body sensation, light sensitivity and more redness that’s apparent in other quadrants. SLK can affect one eye or both eyes, though in bilateral cases, the severity is usually asymmetrical.”
 |
|
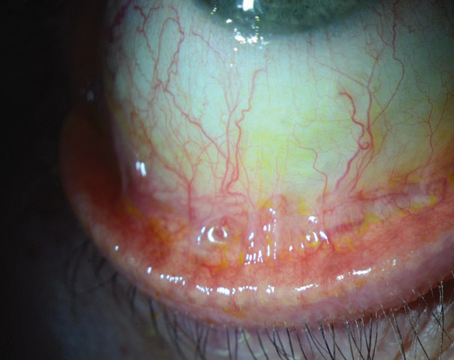
Figure 1A. A patient with SLK showing injection of the superior bulbar conjunctiva with engorgement of vertically oriented blood vessels. (Image courtesy of Sezen Karakus, MD) |
Making the Diagnosis
SLK presents with distinctive clinical features, although its diagnosis can be challenging due to similarities with other ocular surface diseases. “Redness, irregularities, papillae, follicles, scars, or vital dye staining of the tarsal conjunctiva help diagnose the ocular surface disease correctly,” Dr. Karakus says.
When evaluating suspected SLK in the clinic, a slit lamp exam using vital dyes is essential for making the diagnosis (Figure 1). “The involved area of abnormal conjunctiva in SLK is always from 11:00 to 1:00 and may extend pretty far superiorly depending on the severity,” says Christopher J. Rapuano, MD, of Wills Eye Hospital in Philadelphia. “The conjunctiva in SLK will stain with fluorescein or lissamine green. It’s also rather thickened, loose and mobile. There may be some extension onto the superior cornea, possibly with some filaments. Upper lid eversion may demonstrate a velvety pattern.”
“Redness of the superior conjunctiva can be referred to as the hallmark of this condition,” Dr. Karakus says. “This can be observed sometimes macroscopically without using the slit lamp. Conjunctival blood vessels may appear radialized in this area, stretching towards the limbus. Lissamine green staining is particularly helpful for visualizing the affected area, especially in the early stages [before conjunctival injection develops]. This stage can be easier to miss if one looks only for conjunctival redness, but it’s also easier to treat as the inflammation may not be severe yet, allowing for a simpler disruption of the inflammatory cycle. Using lissamine green dye, affected superior bulbar conjunctiva and superior tarsal conjunctiva in contact with it can be easily identified in a mildly symptomatic patient before conjunctival injection appears.
 |
|
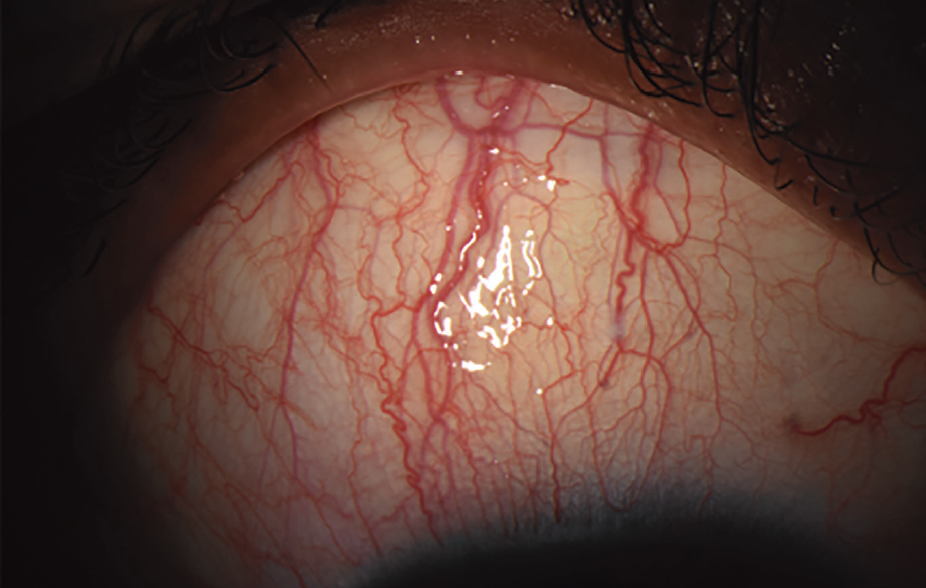
Figure 1B. The affected area is visualized with lissamine green staining. (Image courtesy of Sezen Karakus, MD) |
“Lissamine green dye is also helpful in examining lid margins to visualize keratinization, observe the Marx line, and identify lid wiper epitheliopathy, often present with SLK,” she continues. “These patients frequently complain of significant burning, and the cornea may not show considerable dryness explaining the symptoms. The only finding may be lissamine green staining of the lid wiper area and superior bulbar conjunctiva.”
Fluorescein staining may reveal punctate epithelial erosions, minor abrasions, and filaments, according to Dr. Karakus. She notes that “in patients with SLK, the superior limbal area would look swollen and bumpy and stain with fluorescein that would become more apparent after a few minutes.”
Dr. Rapuano says that having the patient look down and examining the superior conjunctiva is a key part of making an SLK diagnosis. “Whenever I examine a patient with the broad category of ocular surface complaints, I always examine the upper conjunctiva while holding their upper lid up and always evert the upper lid and lower lid. Even if you aren’t suspecting SLK, by always examining the upper conjunctiva, you won’t miss it. If you always examine the fornices and flip the lids, you also won’t miss giant papillary conjunctivitis, floppy eyelid syndrome and mucous membrane pemphigoid. As an added bonus, you might save someone’s life by diagnosing the rare but potentially fatal sebaceous carcinoma.”
Dr. Karakus adds that SLK has been associated with thyroid disease, so it’s essential to rule this out. “If there’s no apparent local reason, such as a tarsal conjunctival scar, chronic allergies resulting in redundant conjunctiva or papillae causing chronic friction in the area and inducing inflammation, a workup should be done to rule out autoimmune diseases causing keratoconjunctivitis sicca and conjunctival inflammation, such as Sjogren’s disease or rheumatoid arthritis.”
Medical Management
Successful management of SLK involves a combination of medical and sometimes surgical interventions aimed at alleviating symptoms, reducing inflammation and improving ocular surface health.
“My main goal of management is improved comfort,” says Dr. Rapuano, who uses a step-wise approach to treatment. “I start with lubrication with preservative-free tears, gels and ointments. Cyclosporine 0.05 to 1% q.i.d. and topical allergy drops are often helpful. If the eyes are dry, punctal plugs may be helpful. If filaments are present, you can use acetylcysteine 10% drops q.i.d. Rarely, I’ll use a short course of topical steroids. I used to use an application of silver nitrate solution 0.5% to the involved area for about 30 seconds, but I haven’t used this in years since silver nitrate solution is no longer readily available.”
Dr. Karakus says she also starts with lubrication using preservative-free tears and ointments as well as punctal plugs. “I prefer vitamin A eye ointment due to its lubricating properties and positive effects on epithelial cell regeneration,” she says. “It also provides support for the goblet cells, which are essential for mucin production.
“In severe cases involving the cornea, a bandage contact lens may be beneficial,” she continues. “If filaments are present, they should be removed before placing the bandage contact lens. Soft steroids are usually helpful in calming the eye in the short term, while immunomodulatory eye drops such as cyclosporine or lifitegrast are typically necessary for long-term management. This condition is often associated with chronic inflammation, and long-term steroid use isn’t preferred.
“If chronic friction and irritation are due to a tarsal scar, a scleral lens or PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) device may be considered as a long-term treatment option,” she explains. “In some cases, a surgical approach to smooth the tarsal conjunctiva, possibly using a mucosal graft, can be considered. Doxycycline is a helpful systemic agent to address inflammation, benefiting from its anti-matrix metalloproteinase-9 effect. In severe cases, I prefer using it at higher doses if tolerated.”
 |
|
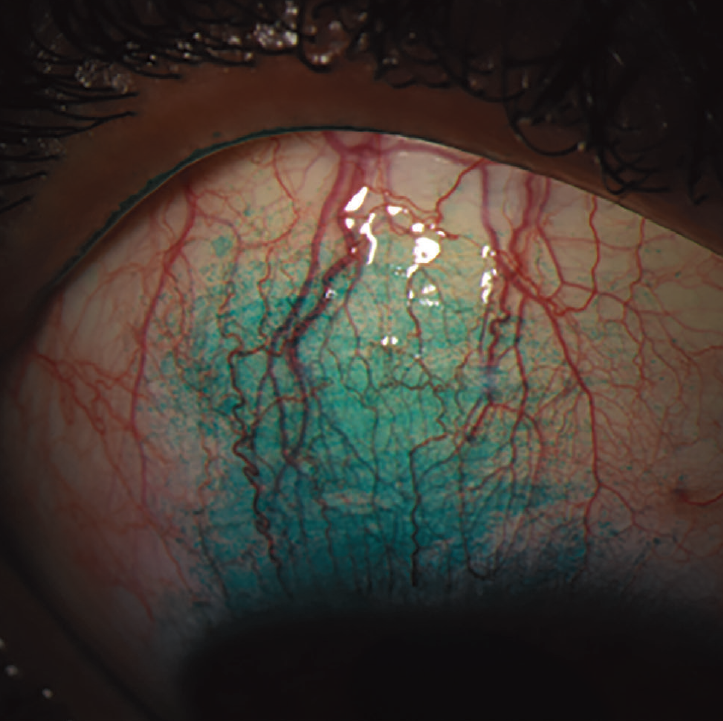
Figure 2. Top: The right eye with SLK demonstrates a thickened, injected leash of superior conjunctiva that stains with lissamine green. Bottom: The same eye has undergone a localized conjunctival cautery procedure to shrink and tighten up the superior conjunctiva. The conjunctival epithelial defects resolved within one week, and the patient’s SLK symptoms greatly improved. (Image courtesy of Christopher Rapuano, MD) |
Surgical Management
Surgical intervention is warranted if patients remain symptomatic despite medical treatment or if there’s frequent recurrence of the condition. Dr. Rapuano typically performs localized cautery to the involved area to shrink and tighten up the tissue (Figure 2). “In the office, I inject local anesthetic under the superior conjunctiva and then very carefully apply cautery to the involved conjunctiva,” he says. “I find it very helpful about 75 percent of the time. It may need to be repeated. Other surgical treatments include conjunctival resection or recession, but I don’t typically need to do those as conjunctival cautery works pretty well.”
For these patients, Dr. Karakus says she performs surgical resection of the superior bulbar conjunctiva with placement of an amniotic membrane. “Some patients also benefit from using autologous serum eye drops in conjunction with or without surgical approaches,” she adds.
Long-term Management
Regular follow-up visits are needed to monitor and assess treatment efficacy and make any necessary adjustments. “Patients should be seen frequently initially to ensure proper response to treatment and to manage any side effects,” Dr. Karakus says. “Once the condition is stabilized, follow-up intervals can be extended, but patients should still be monitored for recurrences or new symptoms. Educating patients about the chronic nature of the condition and the importance of adherence to treatment and follow-up schedules is crucial for long-term success.”
The Bottom Line
A thorough examination of the ocular surface to investigate the underlying cause is the key to successful SLK management. “In advanced cases, ongoing irritation and friction cause the conjunctiva to become more redundant, inducing more friction and inflammation,” Dr. Karakus says. “Reversing structural changes such as keratinization and scarring of the conjunctiva becomes more challenging at later stages, making early diagnosis crucial. Therefore, early detection and intervention are essential to prevent the progression of the condition and to manage it effectively before significant structural changes occur.”
Dr. Rapuano and Dr. Karakus have no related financial disclosures.