Presentation
A 69-year-old Caucasian female was referred to the Wills Eye Emergency Room for suspected neuroretinitis in her right eye. Three years prior, she had a “strange round rash” on her leg, which was associated with bilateral knee pain and swelling. Six months earlier, she noticed off-and-on joint pain in her left wrist. About one week prior to presentation, she noticed flashing lights and blurry vision in her right eye. She was diagnosed with neuroretinitis and treated with doxycycline. She then was referred to the Wills Eye Emergency room after her blurry vision worsened and her clinical picture remained uncertain.
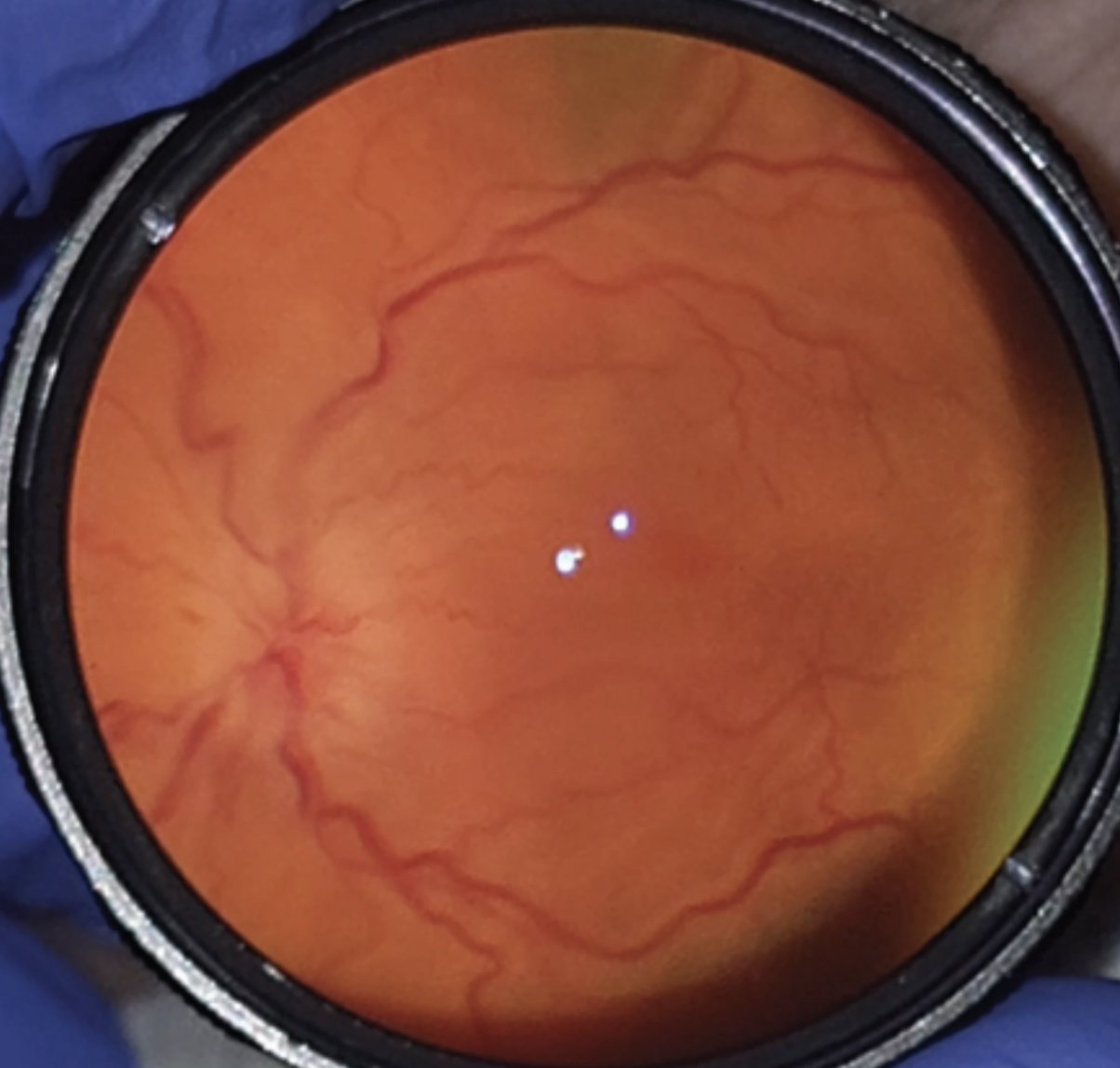 |
| Figure 1. Clinical photo. |
Medical History
The patient had no significant past ocular history. Past medical history included hypothyroidism for 40 years. Family history included glaucoma in multiple family members, age-related macular degeneration in her mother, hypertension in her father, brother and sister; and rheumatoid arthritis in her mother.
Current medications included levothyroxine, vitamin D3, desloratadine, magnesium chloride and doxycycline.
Examination
Ocular examination demonstrated visual acuity of 20/400 in the right eye and 20/20 in the left eye. Pupils were pharmacologically dilated at the time of examination, but no APD was noted by the referring physician. Intraocular pressure was 12 and 15 mmHg in the right and left eyes, respectively. Confrontation visual fields were notable for inferotemporal and superonasal deficits in the right eye. Extraocular motility was full bilaterally. Color plates were 0/8 without recognition of the test plate in the right eye, and 8/8 in the left. Anterior segment examination was notable for decreased tear breakup time and 2+ nuclear sclerosis bilaterally.
Dilated fundus examination of the right eye demonstrated 360 degrees of disc margin blurring, peripapillary edema extending into the macula, and tortuous vessels in the right eye. A small flat nevus was noted near the inferior arcade in the right eye (Figure 1).
What is your diagnosis? What further work-up would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
Brain and orbital MRI with and without contrast revealed mild bilateral perioptic enhancement. The updated differential diagnosis included vascular, inflammatory, infectious and neoplastic etiologies.
The laboratory work-up included ACE, ANCA, Quantiferon Gold, syphilis, Lyme, toxoplasma, and Bartonella serologies, all of which were negative. A lumbar puncture was negative for infectious etiologies, as well as NMO and MOG. A chest X-ray was unremarkable.
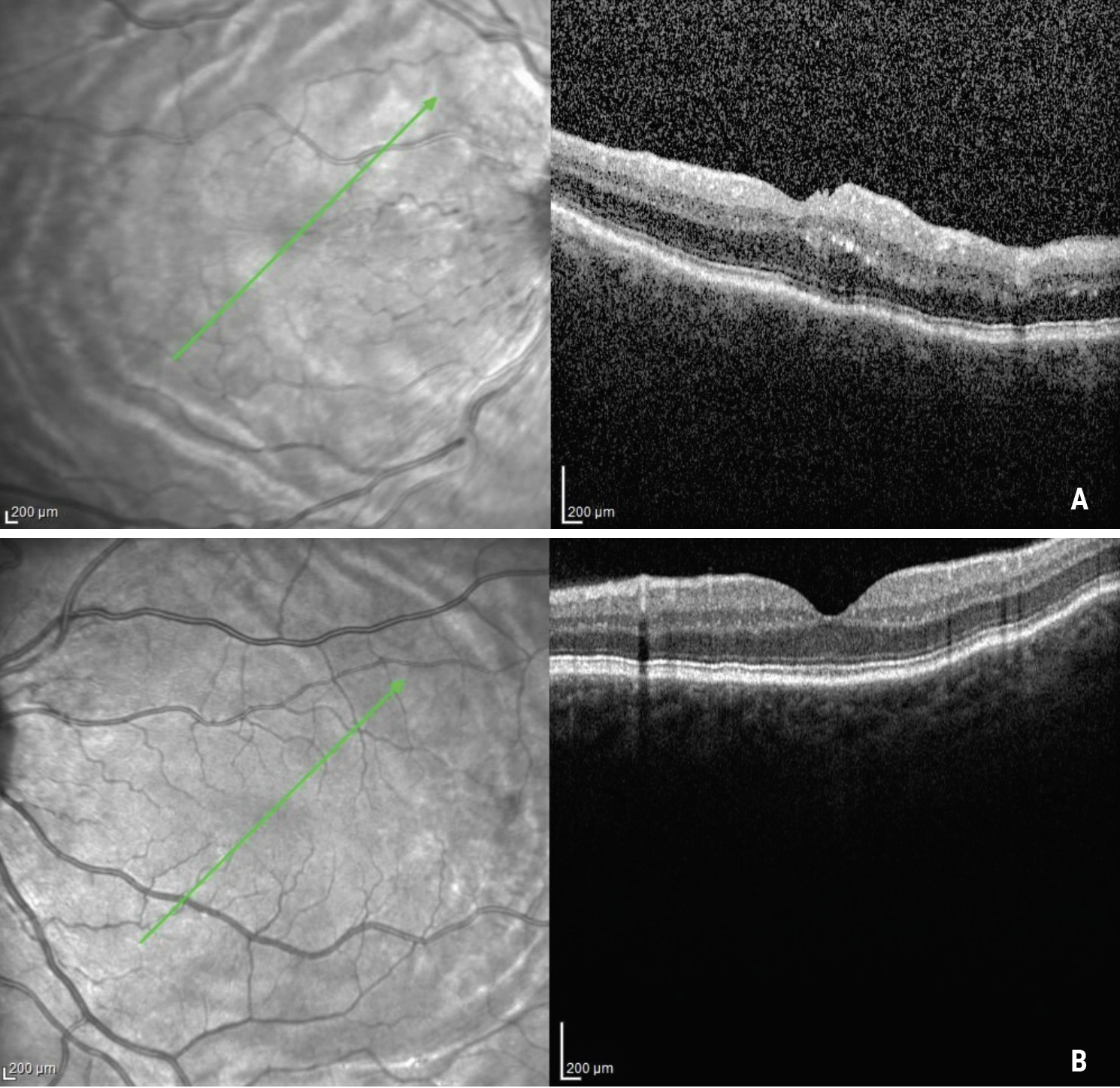 |
| Figure 2. OCTs of the right (A) and left (B) eyes demonstrating choroidal folds. |
She was admitted to Wills Eye Hospital for intravenous methylprednisolone 250 mg every six hours. During admission, the patient’s visual acuity improved from 20/400 to 20/200. Optical coherence tomography and B-scan ultrasound images were obtained. Optical coherence tomography demonstrated optic disc edema with significant thickening of the peripapillary retina in the right eye, and choroidal folds in both eyes (Figure 2). B-scan revealed a “T” sign in the right eye, and sclero-choroidal thickening in the left eye (Figure 3).
A diagnosis of posterior scleritis in the right eye was made and she was started on an oral prednisone 60 mg taper. The patient was referred to a rheumatologist who ordered an extensive laboratory workup which was unrevealing. CT scan was performed without evidence of lung parenchymal abnormalities.
Based on the patient’s family history of rheumatoid arthritis and personal history of arthralgias and joint swelling, suspicion for an undifferentiated autoimmune disease remained high despite a negative work-up.
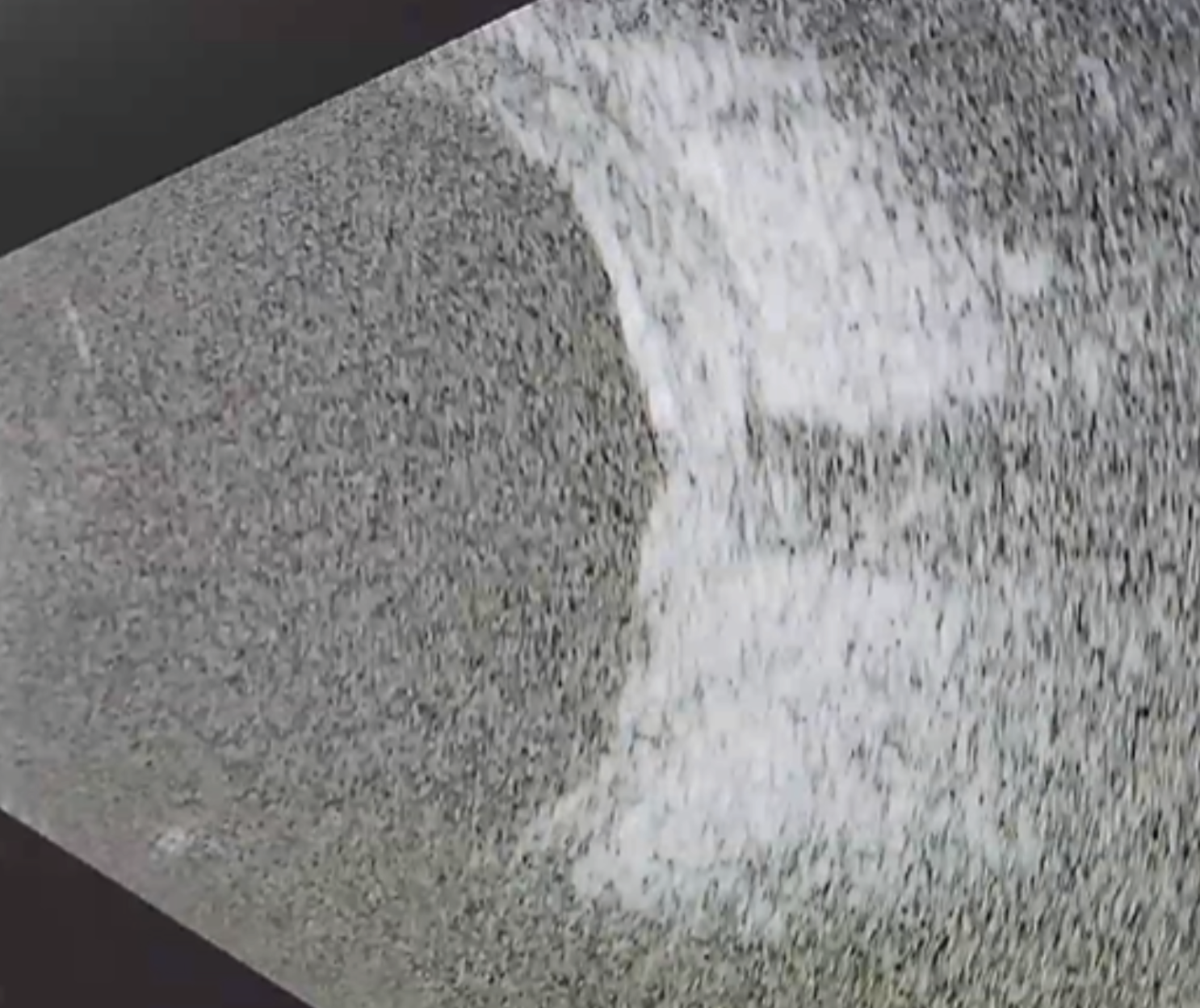 |
| Figure 3. B-scan ultrasonography of a representative patient with sclero-choroidal thickening and a “T” sign representing sub-Tenon’s edema. |
Discussion
As William Benson, MD, recalled in his review of posterior scleritis,1 Peter Watson once remarked “posterior scleritis must be one of the most underdiagnosed treatable conditions in ophthalmology, partly because its manifestations are so protean and partly because the diagnosis is rarely considered.”1 Dr. Benson notes some of the varied presentations of posterior scleritis, including a circumscribed fundus mass, choroidal folds, retinal striae, disc edema, annular choroidal detachment, exudative macular detachment, cystoid macular edema and peripheral retinal detachment. In many cases of posterior scleritis, pain may be minimal or absent.1-4 Diagnosis is usually made with B-scan ultrasonography when a “T” sign is noted, which is caused by edema in the sub-Tenon’s space near the optic nerve head; however, it must be noted that other causes of posterior inflammation such as inflammatory orbital pseudotumor can cause a “T” sign.5-7
Our patient had bilateral choroidal folds. While the right eye was symptomatic, the left eye didn’t have any decreased vision or pain. The differential diagnosis of choroidal folds includes posterior scleritis, neoplasms, papilledema, hypotony, Graves’ disease, macular degeneration and hyperopia.1,8-10
In a case comparison of unilateral to bilateral cases of choroidal folds by Alan Leahey, MD, and colleagues, the most common causes of bilateral choroidal folds included macular degeneration, hyperopia and “idiopathic.”11 It’s been hypothesized that “idiopathic” or “undifferentiated” choroidal folds actually may represent previous posterior scleritis or “silent” scleritis. Another study found that 83 percent of patients with “idiopathic” choroidal folds also had an underlying autoimmune condition such as rheumatoid arthritis, lupus or Crohn’s disease.12 Our patient’s asymptomatic choroidal folds may have been caused by a previous bout of silent posterior scleritis, especially since no hyperopia or macular degeneration were present.
In conclusion, posterior scleritis should be considered even in patients without the classic symptoms and signs on clinical examination. In addition, bilateral choroidal folds can be found in patients with macular degeneration, hyperopia and hypotony; however, it’s possible that some idiopathic causes of bilateral choroidal folds may represent silent or previous scleritis from an underlying autoimmune disease. When encountering a patient with undifferentiated posterior pathology, a B-scan can help rule in or rule out this under-considered and under-diagnosed condition.
1. Benson WE. Posterior scleritis. Survey of Ophthalmology 1988;32:5:297-316.
2. Gonzalez-Gonzalez LA, Molina-Prat N, Doctor P, Tauber J, Sainz de la Maza M, Foster CS. Clinical features and presentation of posterior scleritis: A report of 31 cases. Ocular Immunology and Inflammation 2014;22:3:203-207.
3. McCluskey PJ, Watson PG, Lightman S, Haybittle J, Restori M, Branley M. Posterior scleritis: Clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology 1999;106:12:2380-2386.
4. Lavric A, Gonzalez-Lopez JJ, Majumder PD, Bansal N, Biswas J, Pavesio C, Agrawal R. Posterior scleritis: Analysis of epidemiology, clinical factors, and risk of recurrence in a cohort of 114 patients. Ocular Immunology and Inflammation 2016;24:1:6-15.
5. Biswas J, Mittal S, Ganesh SK, Shetty NS, Gopal L. Posterior scleritis: Clinical profile and imaging characteristics. Indian J Ophthalmol 1998;46:4:195-202.
6. Munk P, Nicolle D, Downey D, Vellet AD, McKeown M. Posterior scleritis: Ultrasound and clinical findings. Can J Ophthalmol 1993;28:4:177-80.
7. Edo A, Harada Y, Kiuchi Y. Usefulness of B-scan ocular ultrasound images for diagnosis of optic perineuritis. American Journal of Ophthalmology Case Reports 2018;12:45-48.
8. Cassidy LM, Sanders MD. Choroidal folds and papilloedema. British Journal of Ophthalmology 1999;83:10:1139-1143.
9. Bird AC, Sanders MD. Choroidal folds in association with papilloedema. British Journal of Ophthalmology 1973;57:2:89-97.
10. Morris AT, Sanders MD. Macular changes resulting from papilloedema. British Journal of Ophthalmology 1980;64:3:211-216.
11. Leahey AB, Brucker AJ, Wyszynski RE, Shaman P. Chorioretinal Folds: A comparison of unilateral and bilateral cases. Archives of Ophthalmology 1993;111:3:357-359.
12. Olsen TW, Palejwala NV, Lee LB, Bergstrom CS, Yeh S. Chorioretinal folds: Associated disorders and a related maculopathy. American Journal of Ophthalmology 2014;157:5:1038-1047.e1.



