Presentation and Initial Work-up
An 84-year old Caucasian female was transferred to our institution for left eye redness, pain and discharge. Eight months prior to her presentation, she had a left lower lid abscess which was managed with systemic antibiotic therapy resulting in improvement in symptoms. However, she had a resultant ectropion, for which she underwent surgical repair about one month prior to her presentation. During this procedure, there was notable mucopurulent discharge that was concerning for infection. She was treated with another round of both topical and oral antibiotics. With worsening drainage, conjunctival injection and pain with extraocular muscle movement, she presented to a local emergency room. A CT scan showed orbital cellulitis and myositis, so she was treated with intravenous broad-spectrum antibiotics. An MRI was performed due to her lack of improvement and showed possible abscess formation in the orbit. She was transferred for management of orbital cellulitis.
Medical History
 |
| Figure 1. External photograph showing a well-defined pink atrophic plaque on the patient’s right hip, with a central focus of ulceration and drainage, consistent with a clinical diagnosis of pyoderma gangrenosum. |
Ocular history was only notable for the above lid abscess and ectropion. Past medical history included hypertension, depression and pyoderma (See Figure 1). Family and social history were unremarkable. Medications included atenolol, amlodipine and sertraline.
Examination
Ocular examination demonstrated visual acuity of 20/30 in the right eye and 20/25 in the left. There was no relative afferent pupillary defect. Intraocular pressures were 16 and 20 mmHg in the right and left eye, respectively. Confrontational visual fields were normal in both eyes. Extraocular motility was full in the right eye, and restricted in all gazes in the left eye. Anterior segment examination of the right eye was normal. Anterior segment examination of the left eye revealed lower lid ectropion with mucopurulent discharge from the inferior fornix, trace lid edema and erythema, and conjunctival injection and chemosis (See Figure 2). Dilated fundus examination was unremarkable in both eyes.
What is your diagnosis? What further work-up would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
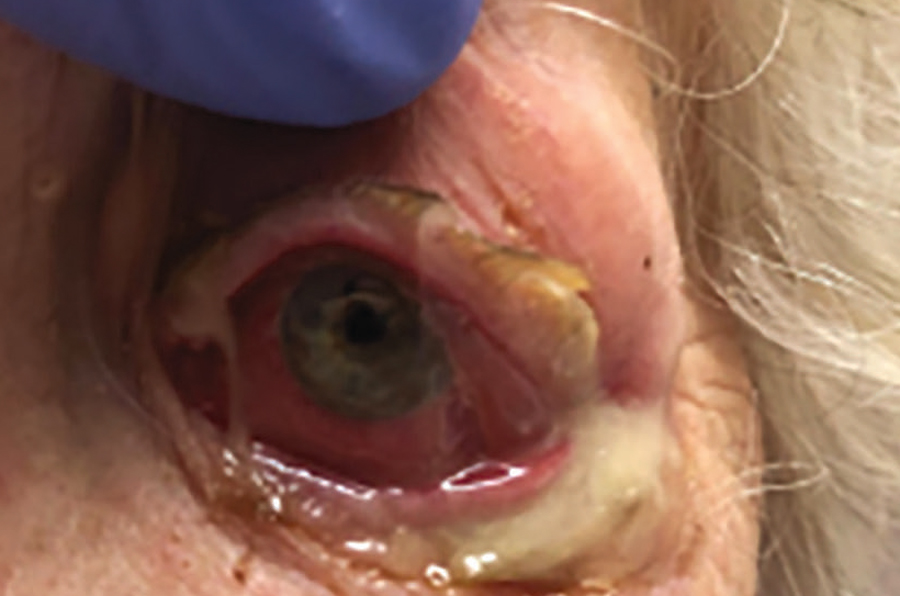 |
| Figure 2. External photograph demonstrating lower lid ectropion, mucopurulent discharge and conjunctival injection of the left eye. |
Repeat CT was obtained to further characterize the orbital process (See Figure 3). CT demonstrated an enhancing mass in the inferolateral left orbit that deformed to the surface of the globe, without frank abscess. MRI further defined this as a soft tissue mass in the left orbit with homogeneous contrast enhancement.
The differential diagnosis of this patient with worsening left eye discharge, conjunctival injection and pain with extraocular muscle motility included infectious, neoplastic and inflammatory etiologies. Infectious causes included bacterial or fungal etiologies. Inflammatory causes included orbital pseudotumor, vasculitis, sarcoidosis or IgG4-related disease. Neoplastic causes, which were less likely, included hematolymphoid tumor, soft tissue tumors or orbital metastasis. Given the patient’s lack of improvement despite prolonged broad-spectrum intravenous antibiotic therapy and history of pyoderma gangrenosum, there was suspicion for inflammatory etiology. A bedside conjunctival biopsy was performed, and intravenous corticosteroid therapy was started.
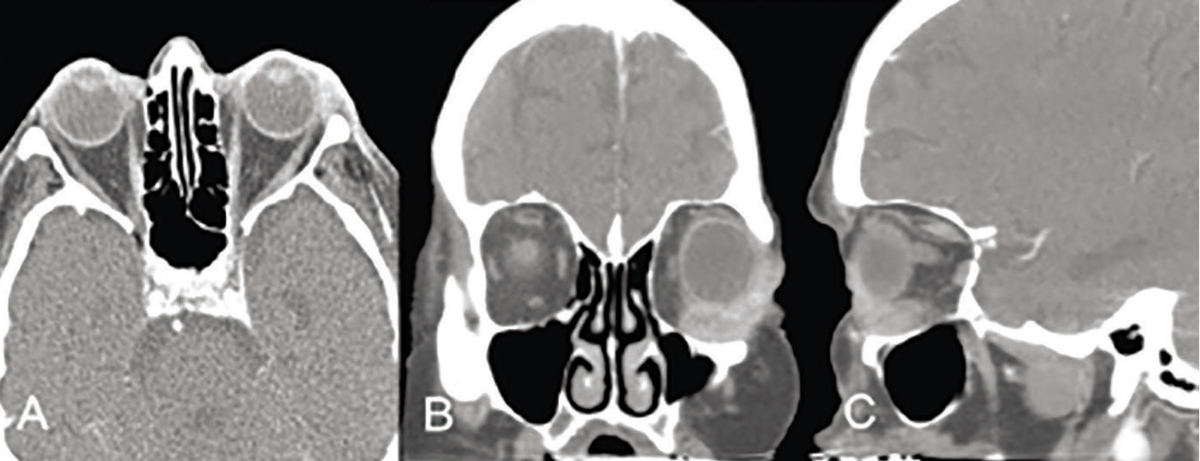 |
| Figure 3. Axial (A), coronal (B), and sagittal (C) cuts of CT imaging showing an enhancing mass in the inferotemporal left orbit that deforms to the surface of the globe, with preseptal soft tissue swelling. |
The patient initially improved on IV steroid therapy and was discharged from the hospital on oral steroids. However, two weeks later, she developed worsening discharge and conjunctival injection. Examination showed possible dellen formation in the inferior cornea. Conjunctival biopsy had shown only nonspecific chronic inflammation, so orbitotomy and biopsy of deeper orbital tissue was performed. This showed palisading granulomatous inflammation and granulomatous vasculitis (See Figure 4). Laboratory studies revealed elevated CRP (2.6), positive ANCA (1:40, nl <1:20), and positive rheumatoid factor (19). Chest X-ray and chest CT showed a right middle lobe infiltrate with irregular margins. With this constellation of findings, granulomatosis with polyangiitis (GPA) was suspected and the patient was started on intravenous rituximab along with daily trimethoprim-sulfamethoxazole (TMP-SMX) and oral prednisone.
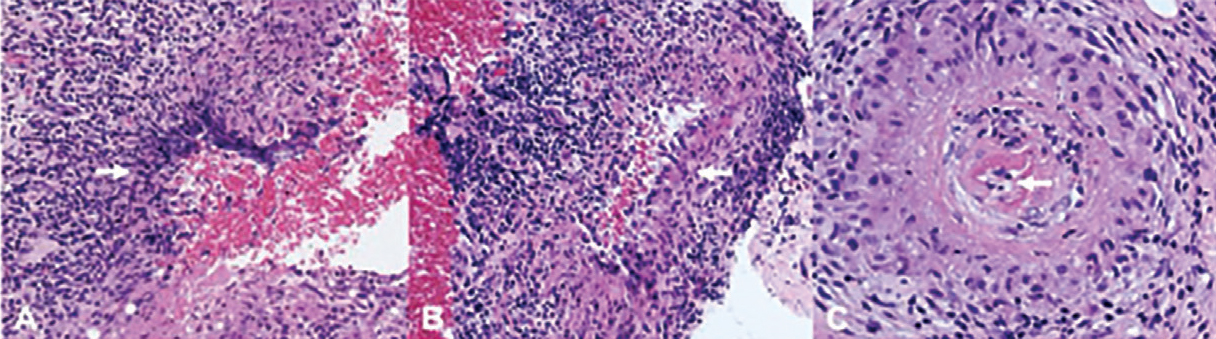 |
| Figure 4. Histopathologic evaluation revealing palisading granulomatous inflammation (A), epithelioid macrophages (B) and granulomatous vasculitis with fibrinoid necrosis (C). |
The patient’s symptoms began to improve with this treatment, and her orbital disease remained quiescent after initial rituximab therapy. She continued to have left lower lid ectropion necessitating lower lid reconstruction with a full thickness tarsal graft, and later developed lagophthalmos requiring release of upper eyelid retractors to allow better closure.
Discussion
GPA is an autoimmune disease characterized by granulomatous inflammation of small to medium-sized blood vessels, especially of the sinuses, lungs and kidneys.1 It’s most commonly found in Caucasian patients in their 40s and 50s, and has no specific gender predilection.2 GPA is associated with anti-PR3 antineutrophil cytoplasmic antibodies (c-ANCA), which have been found in more than 90 percent of patients with the disease and 30 to 50 percent of patients with local disease.3,4
A diagnosis of GPA can be made with high sensitivity (88.2 percent) and specificity (92 percent) with two of five clinical criteria: abnormal urinary sediment; abnormal findings on chest radiograph; oral ulcers; nasal discharge; or granulomatous inflammation on biopsy.5
Ophthalmologic involvement has been found in 50 to 60 percent of patients with GPA.6,7 Orbital involvement is most common (15 percent of patients), but nasolacrimal involvement, scleritis and peripheral ulcerative keratitis are also commonly found.6 Orbital disease is often thought to be spread from contiguous nasal and sinus disease, demonstrated by CT evidence of orbital masses with nearby sinonasal disease and bony erosion.8,9 However, the case presented here demonstrates that orbital involvement may also occur without adjacent sinonasal involvement.
Although our patient’s orbital biopsy proved to be helpful, the initial conjunctival biopsy was not as fruitful. Previous studies have also commented on the efficacy of orbital biopsies. In a study of 13 orbital biopsies from patients with known GPA, only 54 percent of cases demonstrated the classic histopathologic triad of vasculitis, tissue necrosis and granulomatous inflammation.10 In contrast, up to 91 percent of lung biopsies from patients with GPA demonstrate all three features.6 Deeper tissue biopsy, as in the case of our patient’s orbitotomy, may be the key in finding diagnostic tissue.
In addition to the orbital and possible lung involvement, our patient also presented with a necrotic skin lesion that carried a clinical diagnosis of pyoderma gangrenosum. This lesion was never biopsied, but it also showed clinical improvement on steroid and rituximab therapy. Review of the literature reveals that necrotizing skin rash may be a manifestation of cutaneous GPA. In a study of 244 patients with GPA, 14 percent had skin involvement, including palpable purpura and necrotizing ulcers resembling pyoderma gangrenosum.11 Interestingly, studies have also shown patients with GPA to have coexisting biopsy-proven pyoderma gangrenosum.12 Thus, the finding of a skin rash can be evidence of skin manifestation of GPA or another coexisting inflammatory condition.
Once the difficult diagnosis of GPA has been made, immediate treatment is imperative. Although previously treated with cyclophosphamide, the mainstay of treatment is now rituximab.13,14,15 TMP-SMX has also been shown to prevent relapses and reduce risk of infection in ANCA-associated vasculitis.16,17 Both therapies were used in our patient, and showed a favorable outcome.
After successful treatment and remission of active disease, our patient continued to have cicatricial ectropion due to fat necrosis. She had multiple surgeries to correct the ectropion, which demonstrates the refractory nature of the inflammatory condition.
She was later hospitalized for COVID, and discharged to a rehabilitation facility. During this time, she missed a maintenance infusion of rituximab, and had recurrence of discharge from her left eye as well as recurrence of the necrotic hip lesion. This emphasizes the importance of continued treatment in an inflammatory condition such as GPA.
1. Greco A, Marinelli C, Fusconi M, et al. Clinic manifestations in granulomatosis with polyangiitis. Int J Immunopathol Pharmacol 2016;29:2:151-159.
2. Gubbels SP, Barkhuizen A and Hwang PH (2003) Head and neck manifestations of Wegener’s granulomatosis. Otolaryngologic Clinics of North America 36:685–705.
3. Venning MC, Quinn A, Broomhead V, Bird AG. Antibodies directed against neutrophils (C-anca and p-anca) are of distinct diagnostic value in systemic vasculitis. Q J Med 1990;77:284:1287-1296.
4. Woo TL, Francis IC, Wilcsek GA, et al. Australasian orbital and adnexal Wegener’s granulomatosis. Ophthalmology 2001;108:9:1535-1543.
5. Leavitt RY, Fauci AS, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of Wegener’s granulomatosis. Arthritis Rheum 1990;33:8:1101-1107.
6. Pakrou N, Selva D, Leibovitch I. Wegener’s granulomatosis: Ophthalmic manifestations and management. Semin Arthritis Rheum 2006;35:5:284–292.
7. Tarabishy AB, Schulte M, Papaliodis GN, Hoffman GS. Wegener’s granulomatosis: Clinical manifestations, differential diagnosis, and management of ocular and systemic disease. Surv Ophthalmol 2010;55:5:429-44.
8. Kubaisi B, Abu Samra K, Foster CS. Granulomatosis with polyangiitis (Wegener’s disease): An updated review of ocular disease manifestations. Intractable Rare Dis Res 2016;5:2:61-69.
9. Tan LT, Davagnanam I, Isa H, et al. Clinical and imaging features predictive of orbital granulomatosis with polyangiitis and the risk of systemic involvement. Ophthalmology 2014;121:6:1304-1309.
10. Kalina PH, Lie JT, Campbell RJ, Garrity JA. Diagnostic value and limitations of orbital biopsy in Wegener’s granulomatosis. Ophthalmology 1992;99:120-4.
11. Daoud MS, Gibson LE, DeRemee RA, Specks U, el-Azhary RA, Su WP. Cutaneous Wegener’s granulomatosis: clinical, histopathologic, and immunopathologic features of thirty patients. J Am Acad Dermatol 1994;31:4:605-612.
12. de Boysson H, Martin Silva N, de Moreuil C, et al. Neutrophilic dermatoses in antineutrophil cytoplasmic antibody-associated vasculitis: A French multicenter study of 17 cases and literature review. Medicine (Baltimore) 2016;95:11:e2957.
13. Chung SA, Langford CA, Maz M, et al. 2021 American College of Rheumatology/Vasculitis Foundation guideline for the management of antineutrophil cytoplasmic antibody–associated vasculitis. Arthritis Care Res 2021;73:8:1088-1105.
14. Fauci AS and Haynes BF (1983) Wegener’s granulomatosis: Prospective clinical and therapeutic experience with 85 patients. Ann Intern Med 1983;98:1:76-85.
15. Hassan RI, Gaffo AL. Rituximab in ANCA-associated vasculitis. Curr Rheumatol Rep 2017;192:6.
16. Cohen Tervaert JW. Trimethoprim-sulfamethoxazole and antineutrophil cytoplasmic antibodies-associated vasculitis. Curr Opin Rheumatol 2018;30:4:388-394.
17. Monti S, Delvino P, Riboli M, et al. The role of trimethoprim/sulfametoxazole in reducing relapses and risk of infections in ANCA-associated vasculits: A meta-analysis. Rheumatology (Oxford) 2021;60:8:3553-3564.



