Presentation and Initial Work-up
A 67-year-old male presented to the Wills Eye Hospital as a referral from an otolaryngologist for evaluation of left periocular edema and blurry vision. The patient reported that for the past nine months he had been experiencing swelling around his left eye which had started to affect his vision. When he was first evaluated by his primary care physician, he was given a course of oral azithromycin with little improvement in his symptoms. He was subsequently referred to an allergist who prescribed an additional course of oral antibiotics. Due to continued symptoms, the patient was seen by a comprehensive ophthalmologist, who ordered neuroimaging, as well as an otolaryngologist because of several episodes of left epistaxis.
Upon initial evaluation, the patient had a visual acuity of 20/25 on the right and 20/30 on the left. Intraocular pressure was 10 mmHg in the right eye and 11 mmHg in the left eye. There was no relative afferent pupillary defect. Confrontational visual fields were full. Extraocular motility was full. He was noted to have proptosis on the left, measuring 4 mm by Hertel exophthalmometry.
Additionally, there was periocular edema with mild erythema, but no tenderness to palpation. Ptosis of the left upper eyelid was noted. No lagophthalmos was observed. No masses were readily palpated. Resistance to retropulsion was increased on the left. Apart from nuclear sclerotic cataracts in both eyes, slit lamp exam was unremarkable. On fundus exam, RPE changes were noted in both eyes, but the optic nerves appeared to be healthy. Review of CT imaging at that time was notable for a multilobulated cystic mass centered around the frontal and ethmoid sinuses on the left, with erosion through the orbital roof and into the orbit laterally (see Figure 1 below).
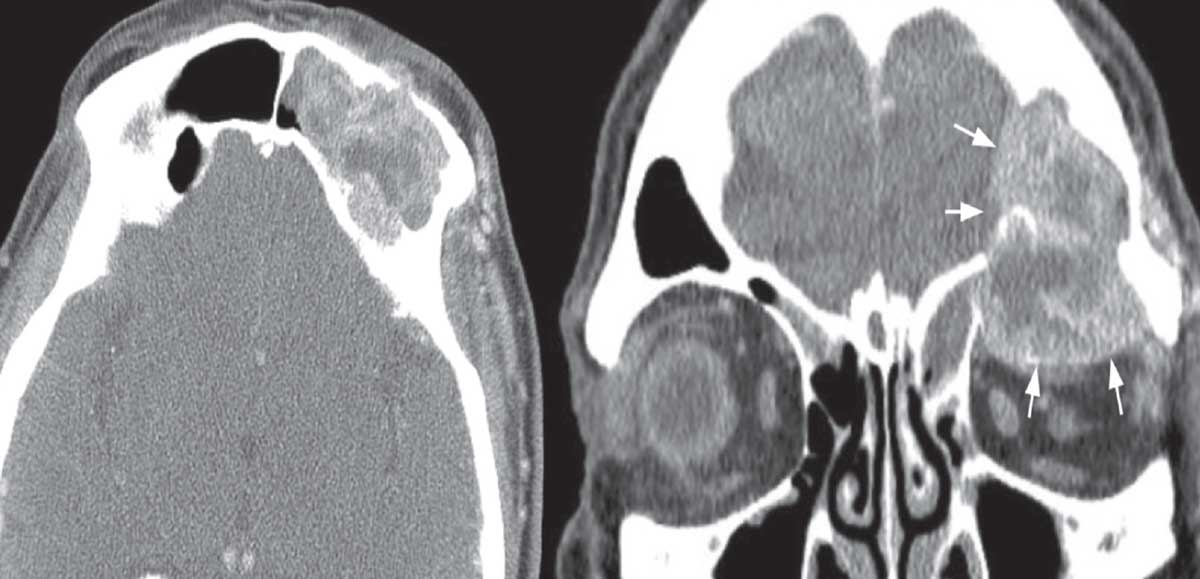 |
| Figure 1. CT imaging. Axial (left) and coronal (right) soft tissue windows of the left skull base lesion. Note extension into the anterior cranial fossa and orbit (arrows) and extensive bone erosion. |
Medical History
Past medical history was notable for coronary artery disease status post multiple stents and four prior myocardial infarctions, atrial fibrillation requiring ablation, diabetes mellitus, hypertension and hyperlipidemia. Ocular history was notable for an eyelid cyst that was removed in childhood.
Family history was notable for a brother with lung cancer. Social history was significant for past tobacco use, the patient having quit 40 years prior to presentation (his pack-year history was unclear). The review of systems was unremarkable.
Current medications included atorvastatin, clopidogrel, gabapentin, glimepiride, insulin, lisinopril, metformin, metoprolol, oxycodone, warfarin and fish oil.
What is your diagnosis? What further work-up would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
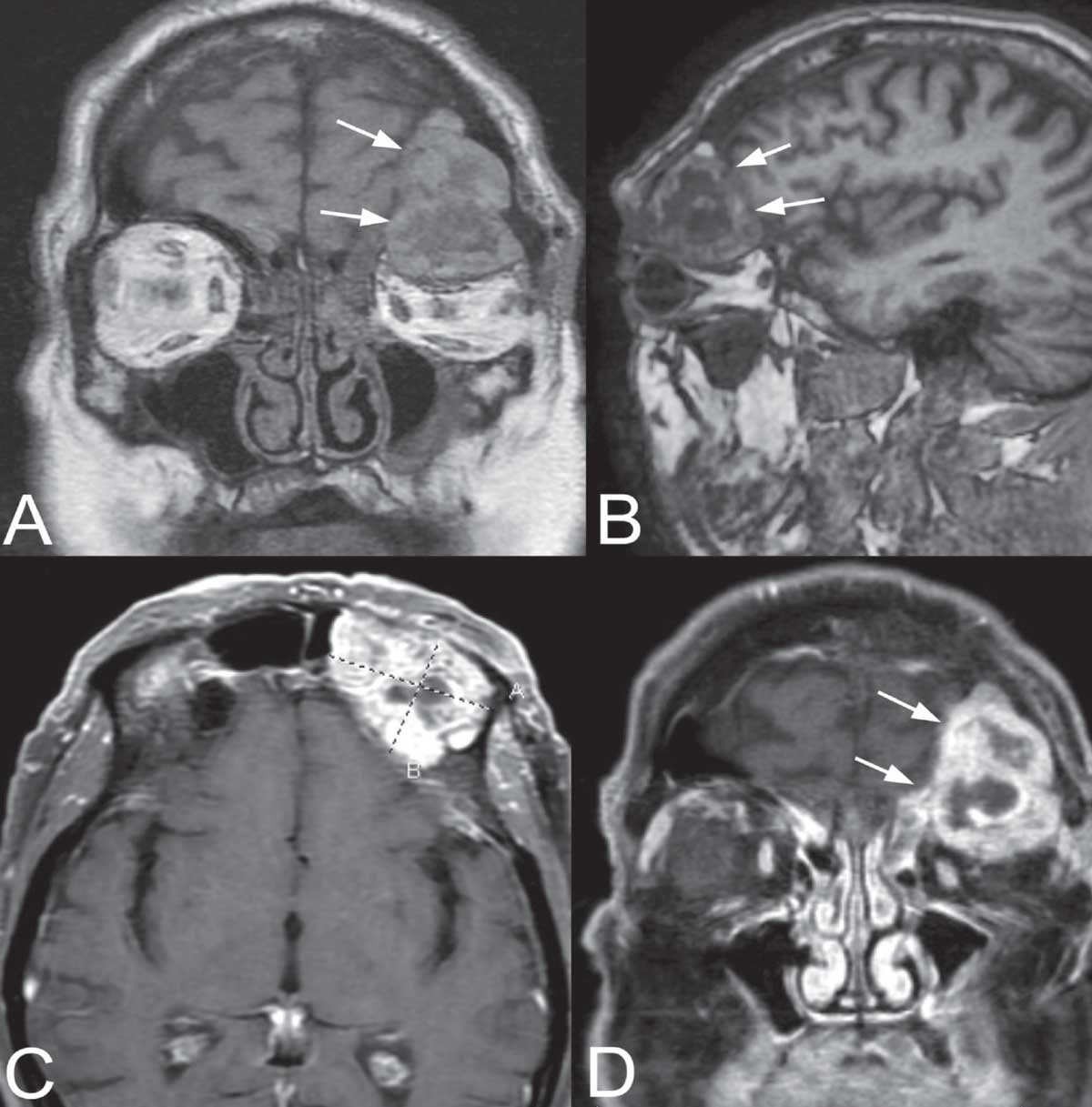 |
| Figure 2. MR imaging. Coronal (A) and parasagittal (B) T1-weighted, pre-contrast views of the left skull base mass (arrows). Note the heterogenous signal within the mass. Axial (C) and coronal (D) T1-weighted, post-contrast views with fat suppression. The mass enhances with contrast, but contains multiple lucencies suggestive of degenerated or necrotic tumor. Click image to enlarge. |
Magnetic resonance imaging was obtained to evaluate the skull base in more detail; the scan showed a markedly expansile lesion (4.4 x 2.3 x 3.9 cm) centered in the left frontal sinus, with erosion into the extraconal superior left orbit and left frontal extra-axial space (Figure 2 on the right). Based on the clinical and neuroimaging findings, the differential diagnosis included fungal sinusitis (especially aspergillosis), mucocele, primary paranasal sinus malignancy, metastatic disease (especially prostate carcinoma), primary orbital mass (especially lacrimal gland malignancy), and aggressive lymphoproliferative disease (diffuse large B-cell lymphoma, mantle cell lymphoma, multiple myeloma). The patient underwent functional endoscopic sinus surgery for attempted biopsy with neurosurgery and oculoplastics on standby, but multiple specimens revealed only nonspecific inflammation on frozen sections. The lesion was then approached via a lateral brow incision into the superolateral orbit. Intraoperatively, the lesion was noted to be discohesive and bled profusely. Erosion of several of the bones of the orbit was noted. Frozen sections revealed a cellular lesion consistent with neoplasia, suspicious for malignancy. Vision, pupillary examination and extraocular motility were noted to be stable postoperatively. Toward the end of the case, the anesthesia team also noted blood in the patient’s Foley bag, initially thought to be secondary to a traumatic Foley catheter insertion. A postoperative urology consultation was obtained.
Final pathology was consistent with metastatic renal cell carcinoma. The patient underwent systemic evaluation, including positron emission tomography, which revealed a 12-cm, hypermetabolic mass in the right kidney, as well as hypermetabolic lesions in the left frontal sinus and right proximal femur, consistent with stage 4 RCC. The patient underwent immunotherapy and palliative radiotherapy.
Discussion
Orbital tumors vary widely in their clinical, histopathologic and imaging features, as well as in their malignant potential and the tissue types from which they arise.1,2 Bone erosion can occur with paranasal sinus fungal infections and is a hallmark of frontal sinus mucoceles. However, primary sinus malignancy and metastatic disease also frequently present with extensive skull base bone changes.
The most common primary sites for tumors that metastasize to the orbit are breast, lung and prostate.1 Clinical presentations vary but commonly include exophthalmos, enophthalmos (in cases of scirrhous breast carcinoma), globe displacement, restriction of extraocular movements, ptosis, decreased vision and pain. Certain pathologies that affect the orbit tend be vascular and bleed extensively during surgery, including multiple myeloma; amyloidosis; and metastatic prostate, renal cell and thyroid carcinomas, as encountered in this case. Notably, these entities may also present with spontaneous bleeding and ecchymosis, narrowing the differential diagnosis for the clinician.
The incidence of RCC has been rising steadily.3-5 RCC is the most common malignant tumor that arises from the renal cortex. It occurs twice as frequently in men and predominantly affects individuals in their seventh and eighth decades of life. Cigarette smoking and obesity have been found to increase the risk of developing RCC. Most cases of RCC are sporadic, but some are associated with von Hippel-Lindau (VHL) disease, with 40 percent of patients with VHL disease developing RCC in their lifetime. Although classically associated with the triad of hematuria, pain and a flank mass, more than 60 percent of RCC cases are detected incidentally, and upwards of 25 percent of patients with RCC will have metastatic disease at the time of initial presentation.6 The most common sites for metastasis of RCC include the lung, brain, liver and bone. Patients with metastatic RCC have a median survival of a little over one year with a five-year survival rate of less than 10 percent.3
In patients without metastatic disease, nephrectomy is the mainstay of treatment. In patients with metastatic disease, surgical resection is considered if it’s likely to improve quality of life by reducing bothersome symptoms; however, patients with solitary metastases at the time of presentation generally do poorly, even if both primary and metastatic sites are treated aggressively.6
Orbital metastasis of RCC is rare, with only a few dozen cases described in the literature, likely by hematogenous spread.5,7 Metastatic RCC lesions tend to enhance on MRI with gadolinium.8 As in this case, orbital metastases may be the first presentation of an occult primary tumor. Other cases have been described in which metastases are delayed many years after initial diagnosis of RCC.7 Biopsy is often required to establish the diagnosis in patients with no known primary malignancy. Additional systemic evaluation with positron emission tomography/computed tomography (PET/CT) is warranted to identify other sites of metastasis.
Once diagnosed, the management of RCC with metastasis to the orbit entails a combination of surgery, radiotherapy, chemotherapy and immunotherapy. As mentioned previously, overall prognosis for patients with metastatic RCC, despite treatment, remains poor.5,7
In summary, RCC metastasis to the orbit is a rare occurrence and typically presents with unilateral proptosis, pain, ptosis and occasionally decreased vision. As was the case in our patient, the metastatic lesion is often the first presentation of RCC, as the primary tumor is often indolent until later in the disease course. A multidisciplinary treatment approach is used to treat patients with metastatic RCC with the aim of minimizing symptoms and improving quality of life. Unfortunately, the prognosis for patients with metastatic RCC is poor.
1. Shields JA, Shields CL, Scartozzi R. Survey of 1264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:5:997-1008.
2. Tailor TD, Gupta D, Dalley RW, Keene CD, et al. Orbital neoplasms in adults: Clinical, radiologic, and pathologic review. RadioGraphics 2013;33:6:1739-1758.
3. Cairns P. Renal cell carcinoma. Cancer Biomark 2010;9:1-6:461-73.
4. Jemal A, Siegel R, Ward E, et al. Cancer statistics 2009. CA Cancer J Clin 2009;59:4:225-49.
5. Magan T, Tuluk M, Bilyk JR, Milman T. Ocular adnexal metastases from renal cell carcinoma: An update and comprehensive literature review. Saudi J Ophthalmol 2021. In press.
6. Motzer RJ, Bander NH, Nanus DM. Renal-cell carcinoma. N Engl J Med 1996;335:12:865-75.
7. Shome D, Honavar SG, Gupta P, et al. Metastasis to the eye and orbit from renal cell carcinoma--a report of three cases and review of literature. Surv Ophthalmol 2007;52:2:213-23.
8. Allen RC. Orbital Metastases: When to Suspect? When to biopsy? Middle East Afr J Ophthalmol 2018;25:2:60-64.



