Presentation
A 57-year-old otherwise healthy woman presented for a second opinion of recently diagnosed Fuchs’ endothelial corneal dystrophy. She noted blurry vision that declined over the course of the day, worse in the left eye compared to the right eye. She was using sodium chloride 5% drops three times daily in both eyes and a hairdryer in the morning (the drying action of which can improve vision for a time) with minimal improvement in vision.
Medical History
 |
| A postop DMEK eye. (the image is from a different patient than the one described in this month’s case). |
The only medical history of note was the patient had a history of hypertension.
Exam
The patient had a best-corrected visual acuity of 20/25 in the right eye and 20/60 in the left. Anterior segment exam was notable for 2+ guttae in the right eye and 3+ confluent guttae and mild edema in the left eye, as well as 2+ nuclear sclerosis cataracts in both eyes. Dilated fundoscopic exam was noted to be within normal limits. Pachymetry showed a central corneal thickness of 523 um in the right eye and 611 um in the left eye. Specular microscopy showed an endothelial cell count of 2,212 cells/mm2 in the right eye and 2,469 cells/mm2 in the left eye. The remainder of the ocular examination was within normal limits.
What is your diagnosis? What further workup would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
For her FECD and visually significant cataract in the left eye, the patient elected to undergo combined Descemet’s membrane endothelial keratoplasty and cataract extraction with intraocular lens implantation. The early postoperative course was routine, and the patient was managed with topical prednisolone acetate 1%, moxifloxacin 0.5%, and ketorolac 0.5% as per standard protocol. At postoperative month one, the patient had an uncorrected distance visual acuity of 20/40 with a well-positioned graft and a clear cornea, and prednisolone acetate 1% was continued four times daily.
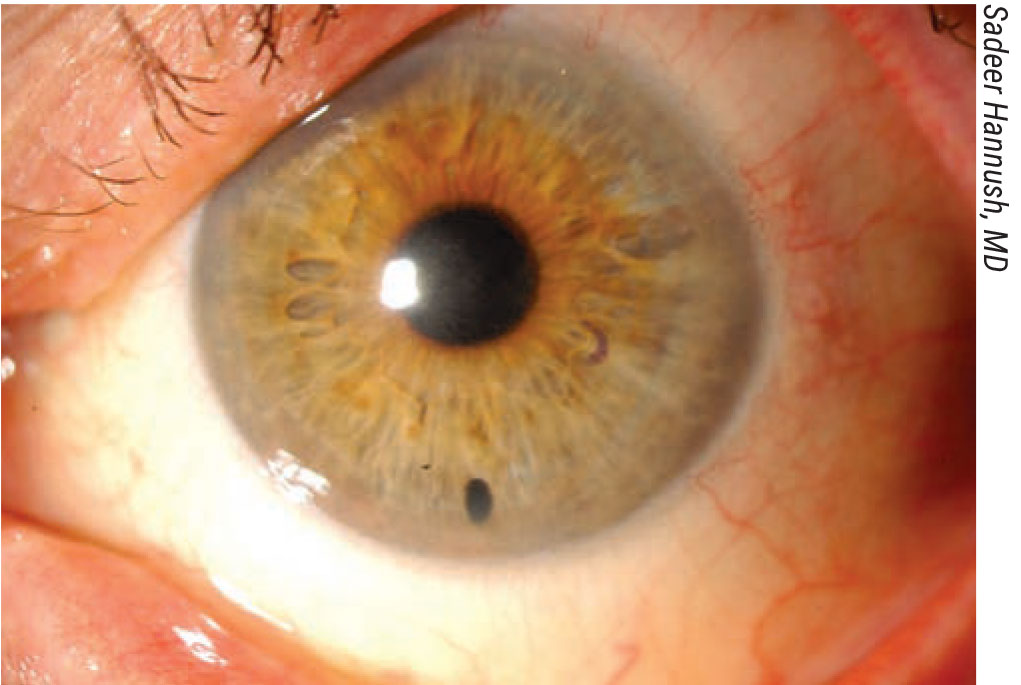
The patient returned at postoperative week seven with new symptoms of photophobia and tearing, describing a migrainous left-sided headache. Examination at that time was notable for a worsened UDVA of 20/125. Anterior segment examination was notable for new DMEK graft interface haze, with clinical photos and anterior segment optical coherence tomography (AS-OCT) presented in Figure 1 (below).
 |
| Figure 1. Postoperative week seven anterior segment imaging. A) AS-OCT showing extensive graft interface haze. B) External photograph showing appearance of patchy inferior haze. C) Slit beam photograph showing a magnified view of the interface haze. |
Given that the interface opacity did not feature any characteristics of fungal interface keratitis (see Discussion), the patient was managed with difluprednate 0.05% every two hours and cyclopentolate 1% twice daily. She experienced improvement in photophobia, although she did report persistent tearing.
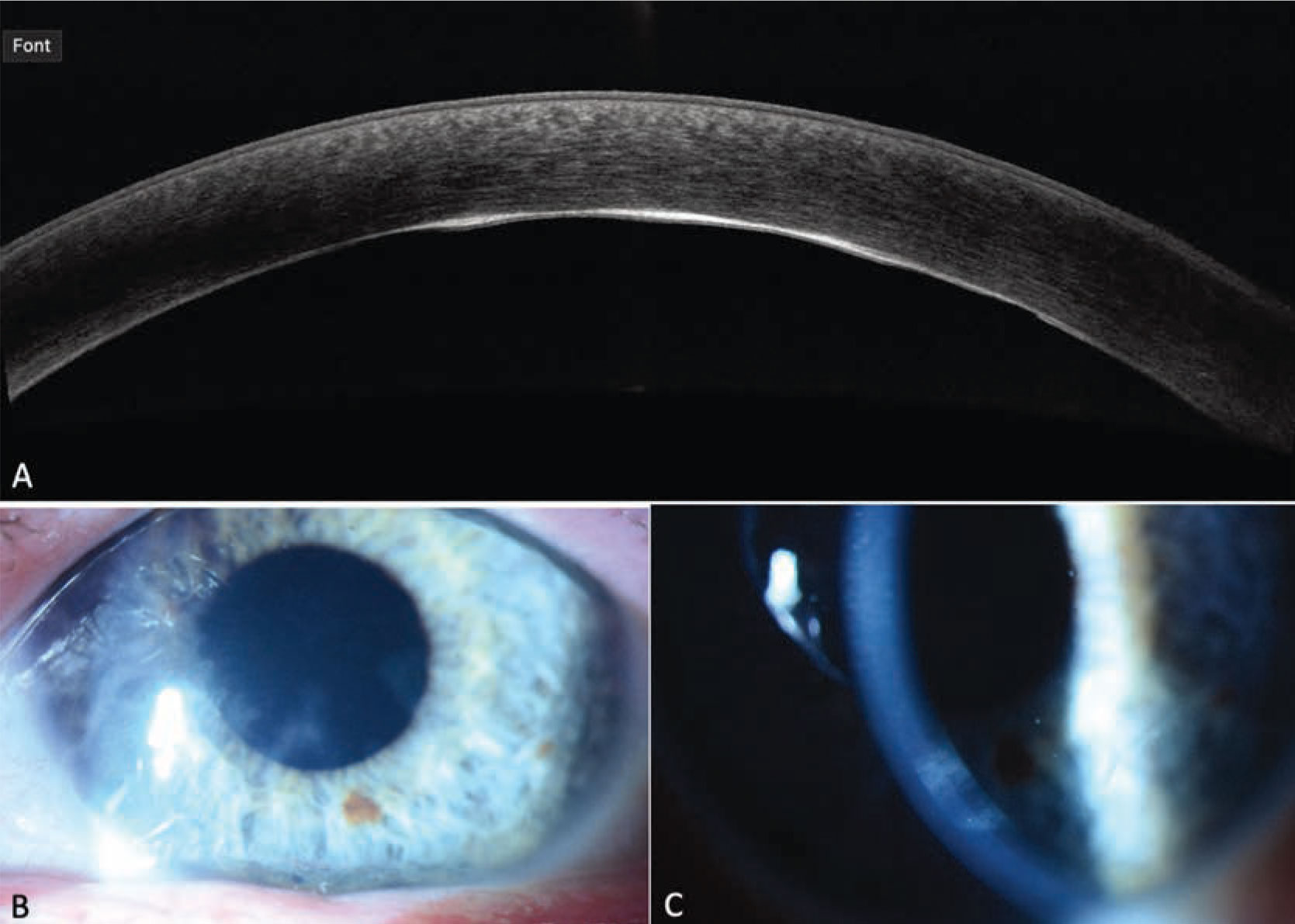
Topical corticosteroids were tapered over several months with improvement in graft interface haze. At postoperative month 11 the patient was noted to have persistent trace interface haze and UDVA 20/200, although BCVA was 20/25 with a refraction of +1.00 +1.50 x155. Figure 2 shows clinical photographs and AS-OCT from this visit, notable for persistent, though much improved, interface opacification. After discussion with the patient, the decision was made to continue monitoring the interface haze given its gradual improvement, and she was counseled that repeat DMEK could be considered in several months pending clinical progression.
Discussion
The patient in this case presented with dense and visually significant corneal guttae in the left eye despite using hypertonic saline drops during the day and a hairdryer in the morning. She elected to undergo a DMEK triple for FECD as well as for her visually significant cataract in the left eye. The early postoperative course was routine and the patient was recovering well until postoperative week seven when she presented with graft interface haze.
DMEK is a safe and effective treatment for corneal endothelial failure, with a mean rate of immune rejection of 1.9 percent.1 Fungal interface keratitis after DMEK is a rare but devastating complication, occurring in approximately 0.15% of cases,2 and there is a trend toward an increase in the rate of fungal interface keratitis.3 Many surgeons routinely perform donor corneal rim fungal cultures at the time of transplant.4 Although there is no consensus on appropriate management of patients with positive culture results in the absence of clinically evident fungal infection, surgeons who perform donor rim fungal cultures tend to follow patients with positive cultures more closely.4,5 The decision to prophylactically treat a patient with a positive donor fungal culture is not taken lightly, as topical therapy has not shown efficacy in preventing infection and alternatives include systemic azole antifungals or repeat transplant with intracameral antifungal therapy.5
 |
| Figure 2. Postoperative month 11 anterior segment imaging. A) AS-OCT showing persistent interface haze, though much diminished from the initial presentation (Figure 1). B) External photograph showing marked improvement in inferior haze. C) Slit beam photograph shows mild persistent interface haze, which was also much improved from the initial presentation (Figure 1). |
This patient’s clinical presentation was initially concerning for either fungal interface keratitis or non-infectious interface inflammation. The decision to treat the patient aggressively with antifungal therapy or to treat the interface haze as a non-infectious inflammatory process with topical corticosteroids was based solely on clinical evaluation and interpretation of AS-OCT. The interface haze seen in this case corresponded to a diffuse hyperreflective process along the graft interface as seen in Figures 1 and 2. In contrast, fungal interface keratitis presents with characteristic focal infiltrates and an otherwise non-inflamed interface on AS-OCT,6 and this patient’s AS-OCT was therefore not consistent with a fungal interface keratitis. The interface in this case was more consistent with previously described elongated textural interface opacities.7 While difficult to differentiate fungal infection from other interface inflammation based on slit lamp examination alone, AS-OCT was critical in suggesting that this inflammation wasn’t fungal in etiology and could therefore be treated with frequent topical corticosteroids, albeit with close follow up. The improvement seen in the graft interface haze during treatment with topical corticosteroids supports the diagnosis of an inflammatory, rather than fungal infectious, etiology. Interestingly, the hyperopic astigmatism the patient manifested may be due to posterior corneal changes induced by the haze over time.
AS-OCT is a relatively new imaging modality that is an excellent tool for evaluating endothelial graft morphology and function after routine endothelial keratoplasty.8 This report highlights another potential use of AS-OCT to manage postoperative complications after endothelial keratoplasty, including diagnosing (or ruling out) fungal interface keratitis. As we begin to perform AS-OCT more routinely on eyes after endothelial keratoplasty, we hope to further characterize the spectrum of graft interface changes and use this knowledge to improve patient outcomes.
1. Deng SX, Lee WB, Hammersmith KM, et al. Descemet membrane endothelial keratoplasty: Safety and outcomes. Ophthalmology 2018;125:2:295-310.
2. Augustin V, Weller J, Kruse F, Tourtas T. Fungal interface keratitis after descemet membrane endothelial keratoplasty. Cornea 2018;37:11:1366-1369.
3. Aldave, Anthony J., et al. Report of the Eye Bank Association of America medical advisory board subcommittee on fungal infection after corneal transplantation. Cornea 2013;32:2:149-154.
4. Ritterband, David. The role of corneal donor rim fungal cultures: Pro side. Cornea 2021;40:9:1085-1086.
5. Price FW. The role of antifungal prophylaxis after receipt of a positive donor rim fungal culture: The case for not routinely treating prophylactically. Cornea 2021;40:9:1096-1097.
6. Beckman KA, Milner MS, Majmudar PA, Luchs JI. Late-onset fungal interface keratitis following endothelial keratoplasty with positive donor fungal culture. American journal of ophthalmology case reports 2020;18:100707.
7. Vira S, Shih C, Ragusa N, et al. Textural interface opacity after descemet stripping automated endothelial keratoplasty: A report of 30 cases and possible etiology. Cornea 2013;32:5:e54-e59.
8. Graffi S, Leon P, Mimouni M, et al. Anterior segment optical coherence tomography of post-descemet stripping automated endothelial keratoplasty eyes to evaluate graft morphology and its association with visual outcome. Cornea 2018;37:9:1087-1092.