A recent cross-sectional population-based study has found that more than 16 million American adults have been diagnosed with dry-eye disease. Prevalence is higher among women than men and increases with age.1 Unfortunately, an ideal treatment modality has yet to be found, but a number of new therapies are in various stages of development. “Dry eye is a huge problem. Everyone wants to be that billion-dollar Restasis (cyclosporine ophthalmic emulsion, 0.05%, Allergan) product,” says Robert Latkany, MD, who is in practice in New York City.
In this article, we’ll take a look at what the pipeline holds for dry-eye therapy.
Devices
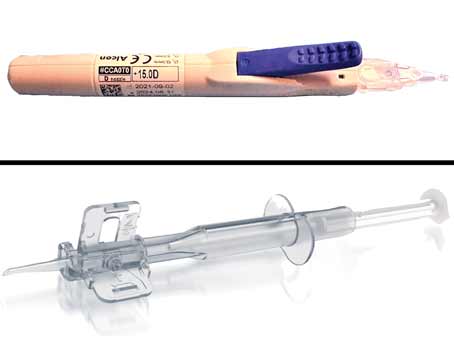
Karl G. Stonecipher, MD, and his colleagues are conducting a retrospective review combining low-level light therapy with intense pulsed light using a new device. The device is known as Eye-light outside of the United States and Epi-C PLUS in the United States (Espansione Marketing S.p.A., Bologna, Italy). “We performed the original physician proof-of-concept study and have followed that up with a four-site, five-surgeon data review to evaluate the effects of this type of therapy on the treatment of dry-eye disease,” explains Dr. Stonecipher, who is in practice in Greensboro, North Carolina.
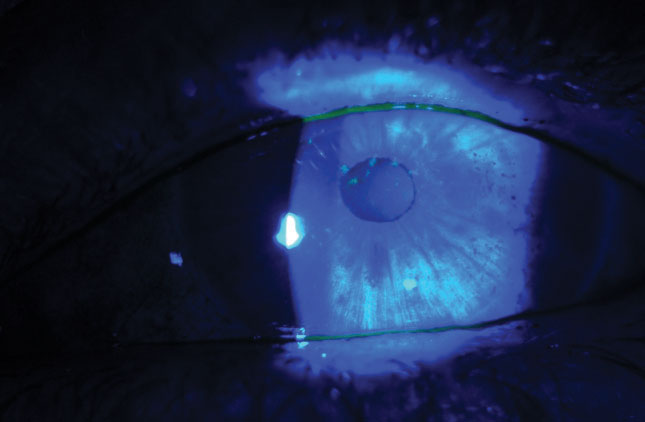
The study focuses on evaporative and mixed-mechanism dry eye. Most of the patients included in the study were diagnosed with Grade 4 meibomian gland disease and had already failed multiple treatments. (Grade 4 corresponds to no expression from the glands, despite multiple attempts.) The study group they reviewed had Ocular Surface Disease Index scores that were at the severe level (>33), and their tear breakup time were less than six seconds. “The low-level light therapy or photobiomodulation basically heats the glands endogenously, and it’s combined with no-gel IPL,” Dr. Stonecipher says. “The results have been exceptional.”
He presented the results of the study at the recent meeting of the European Society of Cataract and Refractive Surgeons in Vienna. “We found that 86 percent of the patients do well with one treatment with one year of follow-up,” he explains. “Fourteen percent of patients required more than one treatment, and, on average, they needed two to three treatments over the course of a year at three- to four-month intervals. But remember, these patients had been treatment failures with multiple [previous] treatments in all cases.”
He presented the results of 310 eyes in 155 patients. Patients’ OSDI scores went from 40.2 down to 21.8 between one and three months postoperatively. The average tear breakup time was 3.58 seconds preoperatively and 7.98 seconds between one to three months postop. MGD grading decreased from 4 to 2 (glands expel cloudy or opaque fluid with digital pressure) postoperatively.
“We’ve been really excited by these findings,” Dr. Stonecipher says. “We have taken it one step further. In patients who have meibomian gland disease and rosacea, we now perform Epi-C Plus. This is no-gel IPL plus low-level laser therapy. There’s a red mask for the MGD (633 nm) and a blue mask for acne rosacea (419 nm), which helps reduce the telangiectasias.”
Outside of the United States, ophthalmologists are using white and yellow masks. The white mask is similar to light therapy for seasonal affective disorder. “The yellow mask stimulates the lymphatics and allows an increase in lymphatic drainage,” Dr. Stonecipher says. “The yellow is 519 nm, the red is 633 nm, and the blue is 419 nm.”
 |
|
|
However, Dr. Stonecipher has noticed that some patients are poor responders to IPL, so he also uses TempSure (Cynosure), a radiofrequency device for aesthetic applications, for the off-label treatment of MGD. “It’s approved for wrinkles around the eye and on the forehead. We’re now using that in addition to low-level light therapy to see if it will heat and stretch the glands even more than IPL,” he says.
According to Dr. Stonecipher, Epi-C low-level light therapy and IPL are both FDA-approved, but combining them for the treatment of dry eye is off-label. “There are different wavelengths that trigger the endogenous heating of the eyelids,” he says. “We are basically heating these fats or this meibum from the inside out.”
Medications
Many new medications are in various stages of development. Last year, Cequa (cyclosporine 0.09%, Sun Pharma) was approved by the FDA to treat dry eye, but it hsn’t yet come to the market. The company is currently planning to start distributing it this summer, according to Dr. Latkany.
“This drug has a different mechanism of action than Restasis with regard to how it penetrates the eye,” Dr. Latkany says. “The company says that it has a faster onset of action than Restasis. Whereas Restasis might take four months or more to reach its maximal peak level of efficacy, this one could start working a few weeks into the treatment.”
According to John Sheppard, MD, who is in practice in Norfolk, Virginia, Cequa has a better side-effect profile than Restasis, while looming generic cyclosporine preparations will undoubtedly reveal a more frustrating side-effect profile than Restasis.
He believes that one of the more exciting products in the pipeline right now is Novaliq’s CyclASol A, which is a preservative-free ophthalmic solution of 0.1% cyclosporine A in EyeSol, Novaliq’s water-free technology. “Because of its molecular characteristics, the drops are only 10 µm in diameter, it has excellent adherence to the surface of the eye, it’s comfortable, it doesn’t sting, and it doesn’t require a preservative,” says Dr. Sheppard. “It has great shelf life, and the risk of infection is low.”
Stephen Pflugfelder, MD, professor and James and Margaret Elkins Chair in Ophthalmology at the Baylor College of Medicine in Houston says that future comparative studies should help ophthalmologists get a clearer picture of where the various new drugs fit in the treatment algorithm. “Unfortunately, right now, there aren’t any head-to-head comparisons between the cyclosporine products, which is really what’s going to be needed in the future to determine where drugs would be used,” he says. “This would include the type of dry eye, the type of profile of signs and symptoms, and the relative efficacy of those things. Additionally, I think a generic cyclosporine will probably come out soon.”
In addition to the new formulations of cyclosporine, Dr. Latkany adds that several versions of loteprednol are in Phase III trials. “Ophthalmologists have been using steroids to treat dry eye for more than 10 years, but everything we are using is off-label,” he says. “Lotemax (loteprednol etabonate ophthalmic gel, 0.5%, Bausch + Lomb) is a higher concentration of loteprednol than Alrex (loteprednol etabonate ophthalmic suspension, 0.2%, Bausch + Lomb), and the side-effect profile of Lotemax is not as high as a stronger steroid, such as prednisolone acetate. Even though it has a low side-effect profile, I don’t feel comfortable letting patients use long-term steroids because of the side effects of glaucoma and cataracts. Alrex is a weaker concentration, and I haven’t seen a lot of side effects with Alrex, even though it is still a steroid. This invites the possibility of weaker concentrations of steroids in the future having some potentially beneficial effect on the treatment of dry eyes without the side effects of cataracts and glaucoma.”
Inveltys (loteprednol etabonate ophthalmic suspension 1%) from Kala Pharmaceuticals was recently approved by the FDA for the treatment of postoperative inflammation and pain following ocular surgery. It’s the first twice-daily ocular corticosteroid approved for this indication. Kala also continues to advance KPI-121 0.25% for dry-eye disease. It’s currently in its third Phase III clinical trial.
“KP-121 [was studied against dry eye’s] signs in both of the first two Phase III trials, but one of the trials missed symptoms, so that earned them a third trial,” explains Dr. Sheppard. “We hope it will be available early next year because it truly addresses an unmet need for prescribers and patients. How that might change things is difficult to say because we already use Lotemax for dry eye. Some doctors with very restrictive insurance companies will welcome a true indication. However, like all new medicines, it’s going to be expensive for some insurance plans. But, then again, Lotemax is expensive, too, and we all know that steroids work great for dry eye.”
Additionally, Aldeyra Therapeutics has developed a new drug called reproxalap that has a completely different mechanism of action. In Phase IIb clinical trials, the drug demonstrated statistically significant improvement across multiple measures of symptoms and signs. Reproxalap is currently in a Phase III trial. “However, it still could be potentially two to four years before we have it in our hands,” Dr. Latkany adds.
According to Dr. Sheppard reproxalap is a new molecule. “[It’s] an entirely new product that blocks the formation of a wide variety of inflammatory mediators that are present in numerous disease states, including allergy, dry eye and uveitis in the anterior segment of the eye,” he says. Dr. Sheppard recently presented Phase IIb results from the use of the drug at the annual meeting of the Association for Research in Vision and Ophthalmology, and says the data were “quite encouraging.”
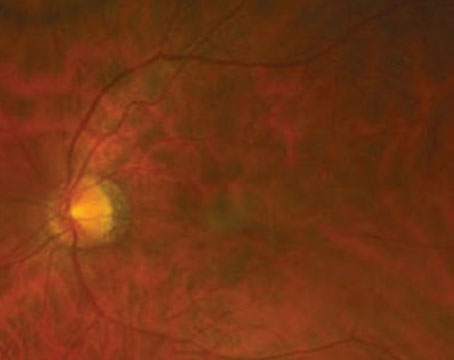
Dr. Sheppard is impressed at how far the industry has come over the past couple of decades. “It’s been a pretty amazing genesis when you think about the fact that, just 22 years ago, we had nothing that really treated dry eye other than tears,” he muses. “Even 10 years ago, we really didn’t appreciate what was going on with meibomian gland disease. So, we’re looking forward to a lot of new therapies. There are some exciting drugs in the pipeline for meibomian gland disease, which is responsible for approximately 84 percent of dry eyes.”
One of these is topical minocycline gel, which is being developed by Hovione. “It’s a large company that’s just beginning its first foray into eye care,” says Dr. Sheppard. “So, we’re just beginning a Phase IIb trial with well-established minocycline. It’s a highly insoluble drug, which basically has to be given in gel or ointment form. Oral medications, obviously, have their disadvantages, so we’re very excited about this trial. Gel seems to be an excellent compromise between an ointment, which most patients don’t like, and an oral therapy.”
Additionally, Azura Ophthalmics (Tel Aviv, Israel) has proprietary technology (AZR-MD-001) for the desquamation and rejuvenation of the anterior lid margin and squamous dermal epithelium. “We all know that the renewal of that epithelium occurs at a very closely regulated rate in normal patients, but the turnover can be accelerated in patients with inflammatory disease or lid margin disease,” says Dr. Sheppard. “This product has been established in dermatology and is being adapted for ocular preparation to control the symptoms and signs of both anterior and posterior blepharitis.”
Also, a pharmaceutical company based in London, TopiVert, has developed TOP1630, which is designed to treat the underlying inflammation that occurs with dry-eye disease. It produced promising results in a Phase I/IIa proof-of-concept study for the treatment of dry eye. “It applies kinase-inhibition technology to the ocular surface,” Dr. Sheppard explains. “Kinases are a universal signaler in inflammatory diseases of all types and all organ systems, including ocular surface inflammation for dry eye. So, these may be both proximal and distal to T cell activation on the ocular surface of the dry-eye patient.”
Another drug with a new mechanism of action is SJP-0035, which is a peroxisome proliferator-activated receptor delta agonist. SJP-0035 is being developed by Senju Pharmaceutical as an ophthalmic solution to promote corneal epithelial wound healing in patients with corneal epithelial disorders, and for the treatment of dry eye. It’s currently being studied in a Phase III trial.
The Future
“We have some exciting times ahead,” Dr. Sheppard says. “We have a couple of drugs that will be out in the next year or two, and then a slew of drugs will be coming out in the next three to five years.” Dr. Pflugfelder is more circumspect. “I think eventually there will be new classes of drugs that may be more effective than what we have right now,” he says. “But, again, it remains to be seen whether they get approved by the FDA. However, I do see drugs in clinical trials that have the potential to be more efficacious than what’s currently available.”
Dr. Stonecipher is a consultant to Allergan, Alcon, Bausch + Lomb, Espansione, Hologics, Kala and Shire. Dr. Sheppard is a consultant to Kala, Sun, Novaliq, Hovione, Azura and TopiVert. Dr. Pflugfelder is a consultant to Allergan, Shire, Kala and Senju. Dr. Latkany has no financial interest in the companies or products mentioned in this article.
1. Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol 2017;182:90-98.