On our annual cataract surgery technique survey, safety and efficiency rule the day, with many surgeons choosing their nucleofractis technique and astigmatism-management method with these factors in mind. Also, surgeons who use femtosecond cataract say it enhances their results, but half of the respondents still aren’t sold on it.
This year, 1,688 of the 12,055 surgeons receiving the survey opened it (14 percent open rate), and 109 completed the survey. To see how your favorite techniques compare with theirs, read on.
Phaco Technique
 |
| Click image to enlarge. |
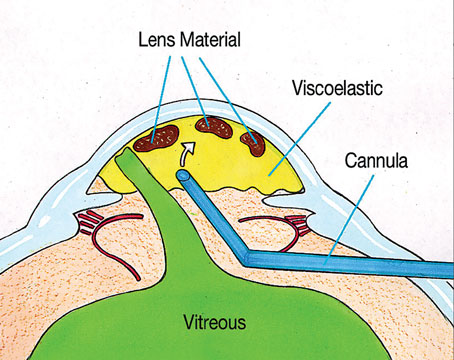
Surgeons shared their thoughts on the best way to break up the nucleus.
Quadrant division remained the most popular method, chosen by 38 percent of the respondents. Twenty-one percent prefer to use stop-and-chop, and 12 percent like a vertical phaco chop maneuver. The rest of the results appear in the graph on the opposite page.
“I prefer quandrant division for its simplicity, the fact that it’s tried-and-true, reliable and very rarely predisposed to complications,” says a surgeon from Minnesota. Curtin G. Kelley, MD, of Columbus, Ohio, says quadrant division is “efficient and safe in nearly all cataract types.”
Ligaya Prystowsky, MD, of Nutley, New Jersey, likes to use quadrant division together with other methods. “I combine it with other techniques depending on the density of cataract and zonular dehiscence. I have a good comfort level with it, since performed it for over 30 years,” she says.
“Quadrant division uses less phaco energy near the cornea,” says a surgeon from Michigan.
Many surgeons who like the stop-and-chop technique say it’s safe and efficient. “I use stop-and-chop because it’s easy when approaching any kind of cataract,” says one surgeon. A surgeon from Utah likes stop-and-chop for specific maneuvers. “It gives the surgeon better control of nuclear removal with initial groove and crack, then vertical chop,” he says. A surgeon from San Antonio likes stop-and-chop’s versatility. “It’s good for a wide variety of lenses,” he says. Another surgeon chooses stop-and-chop because it, “Lets me do a quick debulking of the nucleus, and allows more spaces for subsequent chop.” A surgeon from California says, “I like stop-and-chop because of its consistency.”
Ben Mackey, MD, of Corbin, Kentucky, prefers a vertical phaco chop technique. “Low phaco power is needed [with this technique] and I can chop with a small pupil and still visualize the case,” he says.
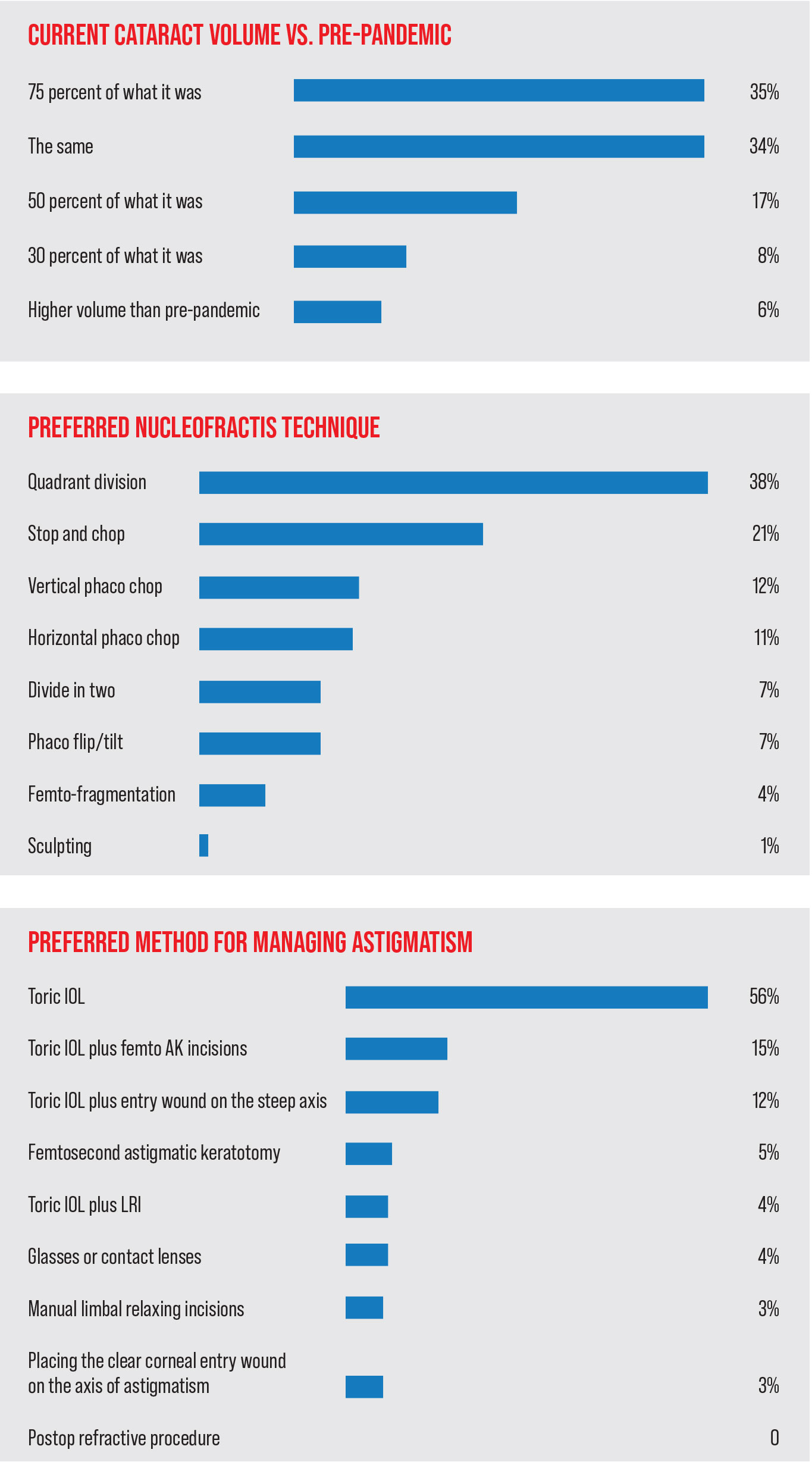
Managing Astigmatism
 |
| Click image to enlarge. |
Just like last year, a toric intraoacular lens is the preferred option for astigmatism management among our respondents (chosen by 56 percent of them).
“For over a diopter of astigmatism I use a toric IOL because it’s effective and predictable,” says Daniel Pluznik, MD, of Washington, D.C. “For less than one diopter I use femto LRI.” Jeffrey Whitman, MD, of Dallas uses the toric because, he says, “It’s the most accurate for getting rid of all of the astigmatism.” Many of the surgeons like the toric’s predictability. “[With it] I’m able to better predict lasting outcomes compared to an LRI,” says a surgeon from Oregon.
Dr. Prystowsky likes the options available for toric lenses. “There are more choices now with premium IOLs,” she says.
The next most popular option, a toric lens combined with femtosecond astigmatic keratotomy, was chosen by 15 percent of the surgeons.
“It works well. But this does depend on the amount of astigmatism,” says a surgeon from Ohio. A surgeon from California likes an IOL with femto AK because, she says, “It’s accurate and adjustable.” A surgeon from Texas says this approach is “Great for a wide variety of treatments.”
One surgeon voices the opinion of many on the survey, saying, “I use every method depending on whether there’s a small, medium or large amount of astigmatism. You customize the treatment—there is not typically one option.”
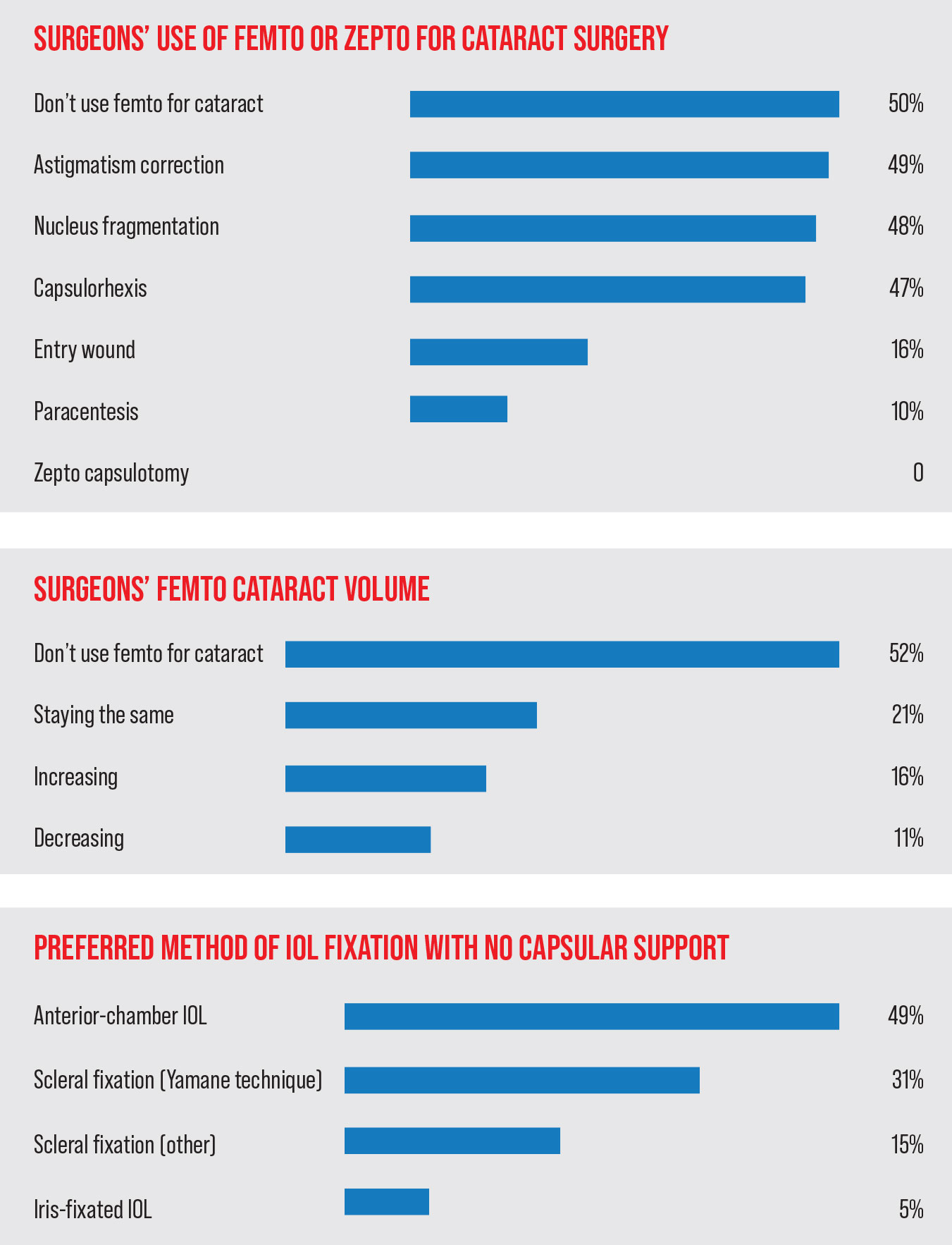
Femto or No?
 |
| Click image to enlarge. |
An often talked about but not often done variety of cataract surgery is femtosecond-assisted cataract. Half of the respondents don’t use the femtosecond laser in conjuction with surgery. For those who do use it, they use it mostly for correcting patients’ astigmatism (49 percent), fragmenting the nucleus (48 percent) and for creating the capsulorhexis (47 percent). (Surgeons were able to choose more than one answer regarding how they use the femtosecond, if at all) None of the surgeons on this year’s survey use the Zepto device for the creation of a capsulotomy.
Most of the surgeons (65 percent) who perform femtosecond-assisted cataract surgery say their volumes are either staying the same (45 percent) or decreasing (20 percent) in recent months. Thirty-seven percent of the respondents say their femto-cataract volume is increasing.
Surgeons opined on why they use the femtosecond. “It’s precise, reliable, and is good for marketing and for earning additional income,” says a surgeon from Tennessee. Alan Aker, MD, of Boca Raton, Florida, appreciates what the laser brings to his procedures. “It reduces energy and protects the cornea—especially in patients with dense nuclei and/or low endothelial cell counts,” he says. “A perfect capsulorhexis is helpful. Our goal is to do everything to optimize a patient’s outcome and achieve 20/20 for all patients one day after surgery. We always use femto with premium IOLs.” Jimmy Hu, MD, of New York City agrees, saying, “It gives a perfect capsulotomy every time, and provides good control of astigmatism correction.”
Then, there is a contigent that uses femto, but also sees room for improvement. “I like the reliable LRI’s and nuclear disassembly,” says Steven Pascal, MD, of Oakland, California. “I don’t like the unreliable incisions, and the fact that it makes cortex removal exponentially more difficult.”
“It prefragments pieces during phaco but can lead to bag rupture with the bubbles in the bag it causes,” says Naja Chisty, MD, of Columbia, Missouri. A surgeon from New Orleans agrees there are pros and cons to consider. “I don’t like the cost factor,” he says. “I’d prefer to use it for all NSC of 3+ or greater. I do like the precision of the capsulorhexis and nucleus fragmentation in denser NSC.”
Looking down the road, 20 percent of the surgeons say they’re likely to use femtosecond cataract surgery in the future, and 11 percent say they’re “somewhat likely” to do so. Sixty-six percent say they’re unlikely to start performing it.
For the group that doesn’t plan to use it (66 percent of respondents), the femtosecond has issues that are deal-breakers for them. “It increases the risk of capsulotomy tear compared to my manual capsulorhexis technique,” says Carl Clavenna, MD, of Birmingham, Michigan. A surgeon from California says the femtosecond “is too expensive and time-consuming.” A surgeon from New Jersey agrees, saying, “I stopped after 25 cases. There was no increase in complications, but it added too many steps, costs and time to patient care.” An ophthalmologist from Oregon believes his current methods serve him and his patients well. “Femto cataract surgery is a solution looking for a problem,” she says. “It’s just a way to jack up the bill to compensate for sub-$600 surgery. It’s no better or safer than conventional phaco. Patients pay for it out-of-pocket because they think it’s better and a ‘laser’ is used.” However, one surgeon appreciates femto’s efficiency. “I think it is excellent for nuclear fragmentation and capsulorhexis,” he says. Another surgeon likes femto-cataract because it “makes the surgery a little safer and it reduces phaco energy,” but, he says, “It costs too much.”
Technique Potpourri
The survey’s respondents also shared their views on several other aspects of surgery.
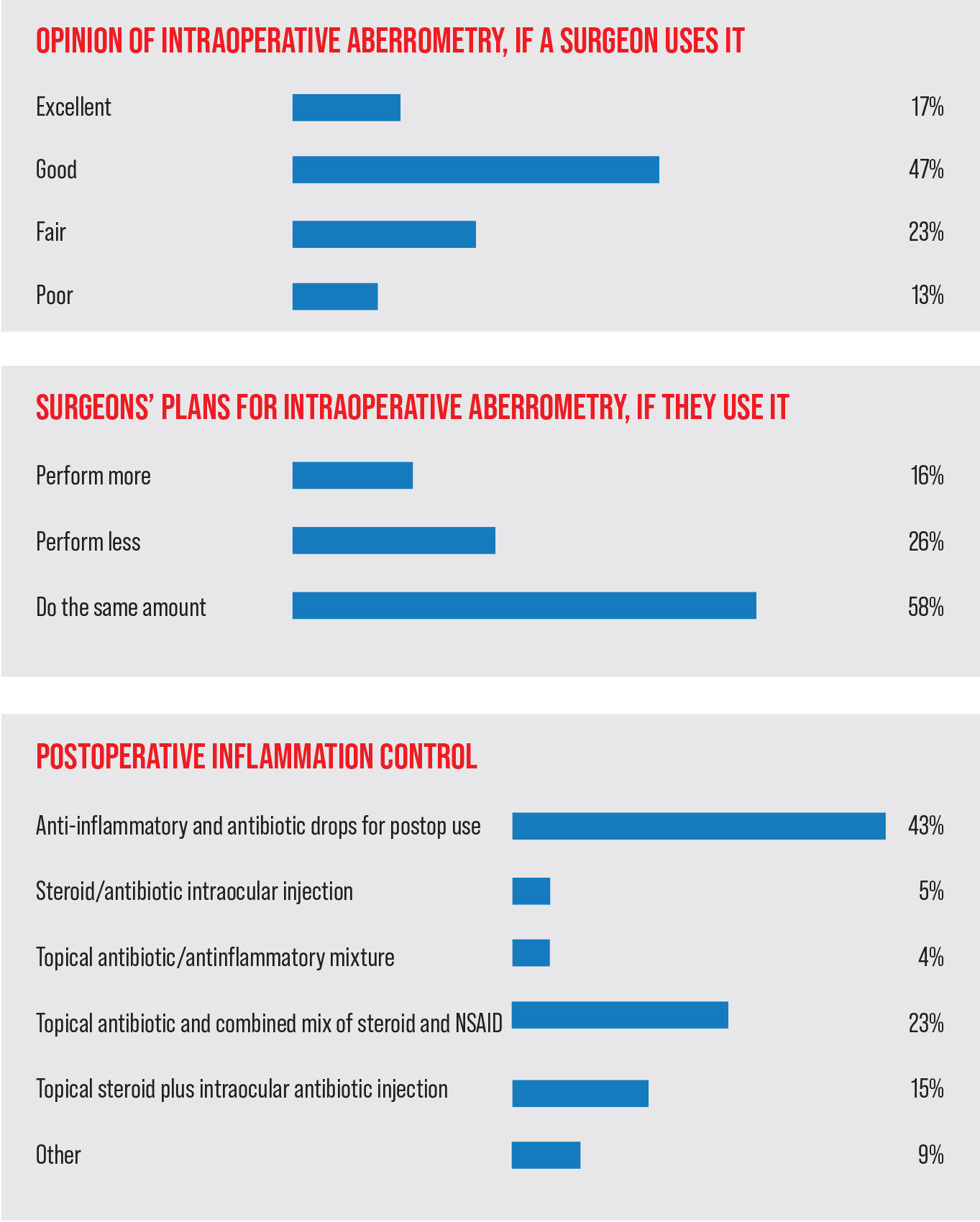
• Intraoperative wavefront aberrometry. Fifty-seven percent of the surgeons don’t use intraoperative aberrometry to select and place intraocular lenses. Of the ones who do use it, 17 percent say it gives them excellent outcomes, 47 percent say its outcomes are good, 23 percenthink they’re fair and 13 percent think the outcomes are poor.
“Intraoperative aberrometry is good for refining sphere, especially in post-refractive cases,” says a Tennessee surgeon. “But it’s not great for the toric IOL amount, and alignment is very touchy. Overall, it’s not ‘fun’ to use.” Dr. Pascal takes issues with the technology, as well. “It helps align the axis of astigmatism,” he says. “But, on some occasions, it chooses a lens that is less accurate than if I had relied on the biometry calculations instead.” A surgeon from Kentucky agrees, saying, “It either confirms your pre-op measurements or it recommends a change which half of the time is wrong.” A surgeon from South Carolina says it may not be helpful in the cases that really need it, saying, “It still doesn’t address outliers of effective lens position.”
Chicago’s Jonathan Rubenstein, MD, however, says the technology is useful in challenging patients. “It yields increased IOL power accuracy in post-refractive-surgery patients,” he says. A Michigan surgeon appreciates intraoperative aberrometry in astigmats. “It’s very helpful in refining spherical power and lining up toric IOLs,” she says. Fellow Michigander Dr. Clavenna agrees, saying, “It helps me fine-tune the cylinder corrections.”
• Promoting a wide pupil during surgery. Surgeons have a variety of techniqes at their disposal for managing a patient’s pupil. Here are the ones they turn to the most.
Forty-eight percent of respondents use an intracameral injection of epinephrine and lidocaine, 26 percent use mechanical pupillary dilation and 10 percent use Omidria (phenylephrine and ketorolac injection). Eighteen percent say they don’t take any additional steps. For those who use mechanical means to ensure dilation, most choose a Malyugin ring, with a small number saying that they rely on iris hooks.
“I’ll use a pupil expansion ring if the patient isn’t adequately dilated with meds,” says a surgeon from Oregon.
• Surgical pearls. The surgeons on the survey also provided their favorite tips for getting good outcomes:
— “Spend time with each patient to create a proper plan for outcomes, then keep the ultrasound energy to its lowest level for a quicker recovery.” (Curtin G. Kelley, MD)
— “Clean the back of the anterior capsule to keep the capsule periphery clear long term.”
— “With the sole exception of an expulsive hemorrhage, there is no necessity for immediate action. Take your time and be cool.”
— “Don’t overestimate your skill level. Be friends with a highly skilled surgeon, refer readily and learn. There’s very little margin for error and patients have HIGH expectations today.” (Timothy Hodges, MD, Tucson, Arizona)
— “Use a pre-chopper for speed, and lower phacoemulsification energy.” (Bill Clifford, MD, Garden City, Kansas)
— “Watch out for loose zonules. If the lens is moving as you’re grooving, increase the phaco power and be gentle.”
— “In eyes with a previous trab and 360 degrees of posterior synechiae, place Viscoat through the PI to free up iris from the lens capsule, then pierce the cyclitic membrane with a cyclodialysis spatula to allow placement of a Malyugin ring.”
Overall, one surgeon advises not to try to do too much. “Perfect is the enemy of good,” he says.