Workup, Diagnosis and Treatment
 |
Given the patient’s clinical findings, a differential diagnosis included etiologies that could cause signs and symptoms of deficits in multiple cranial nerves or extraocular muscles, Horner’s syndrome, proptosis, resistance to retropulsion and downward displacement. This included inflammatory etiologies such as idiopathic orbital inflammatory syndrome, thyroid eye disease and orbital vasculitis, neoplastic causes such as benign or malignant intraorbital masses and vascular etiologies such as orbital varix, carotid-cavernous fistula, orbital arteriovenous malformations and veno-lymphatic malformations.
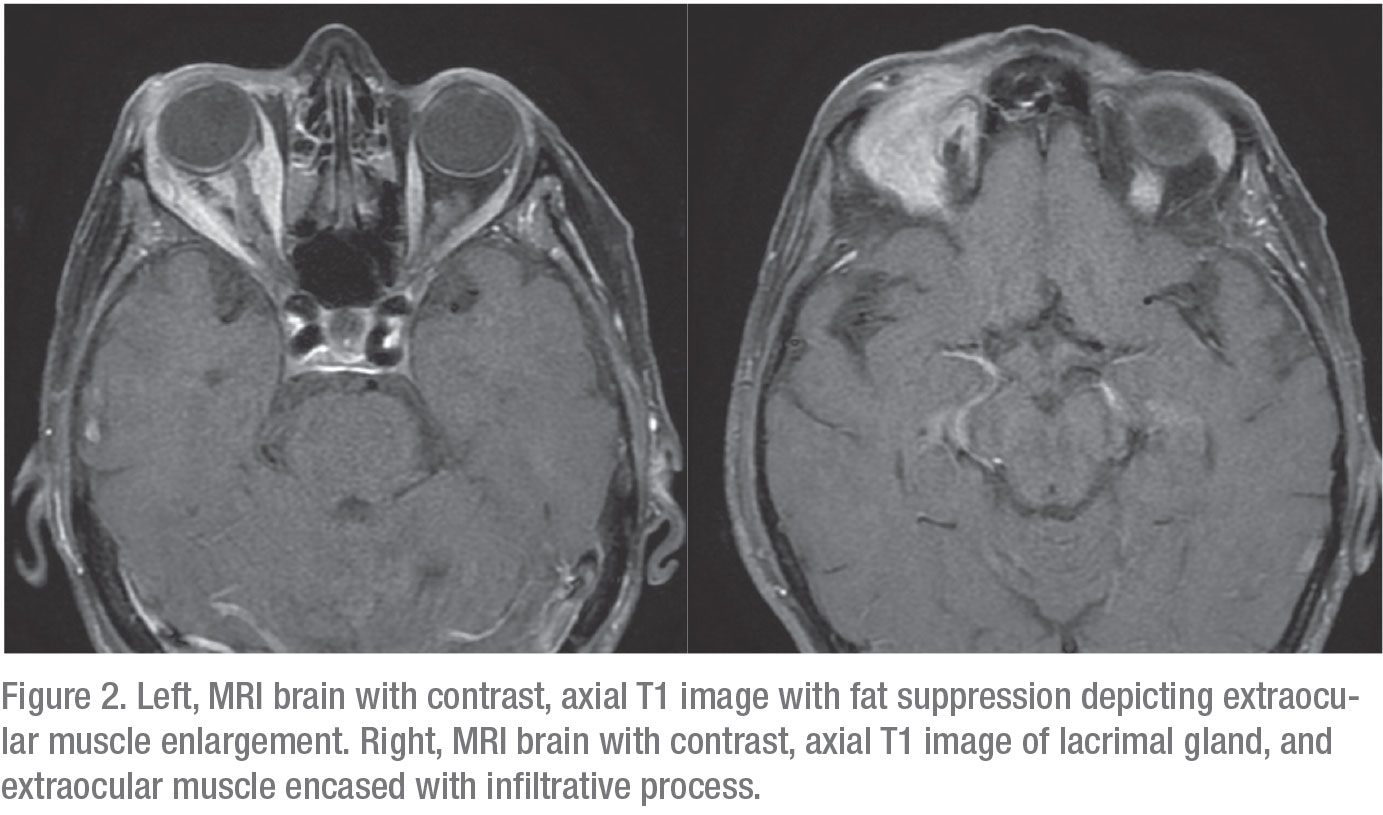
An MRI of the brain with and without contrast was indicative of a multispacial, infiltrative and continuous process involving the extraocular muscles, lacrimal gland and orbital fat. Given the patient’s history of remote breast cancer, these findings were thought to be consistent with metastatic breast cancer to the right orbit. The patient was then referred to an oculoplastic surgeon for biopsy. Biopsy of the lacrimal gland was significant for evidence of chronic inflammation and fibrosis on H&E staining. It was positive for cytokeratin AE1 and AE3 immunohistochemical stain, significant for carcinoma. Further specialized immunohistochemical staining was positive for CK7+, GATA3+ and ER+, narrowing the diagnosis of metastatic breast carcinoma, lobular type. Predictive and prognostic markers were also obtained on histology; biopsy was positive for ER and negative for Her2/neu. The patient was subsequently referred back to her primary medical oncologist for further systemic evaluation and consideration for additional treatment of metastatic disease.
Discussion
Though any cancer in the body can metastasize to the orbit, most orbital metastases are derived from lung, breast or prostate tumors. Presenting symptoms often include pain, proptosis and early ophthalmoplegia, though orbital metastases can present in a myriad of ways. Extraocular muscles are frequently involved, due to their abundant blood supply. Of those patients who present with metastatic tumors to the orbit, 75 percent have a history of known primary tumor. This leaves 25 percent of patients presenting with metastatic tumors to the orbit without a known primary.1 These patients require immediate referral to a medical oncologist for systemic imaging and laboratory evaluation.
A survey from the Wills Eye Hospital Ocular Oncology department of 1,264 patients with orbital tumors and simulating lesions found that the three most common types were lymphoid tumors, idiopathic orbital inflammatory syndrome and cavernous hemangioma. Of these lesions, 64 percent were found to be benign, while 34 percent were malignant. Notably, the percentage of malignant lesions compared to benign lesions increased with age, comprising 58 percent of lesions in older patients age 60 to 92. Of those subclassified as having metastatic tumors to the orbit, 48 percent were due to breast carcinoma, making breast carcinoma the most common orbital metastasis.2
Breast cancer is the most common primary source of orbital metastases in women. It has a propensity to invade the extraocular muscles and orbital fat, theorized to be due to the increased relative estrogen concentration in these regions. Metastasis can occur many years after the initial breast cancer has been removed, as in this case, therefore a history should always include inquiries about previous cancer surgery.3 Breast metastasis to the orbit can rarely also elicit a fibrous response in the orbit, causing enophthalmos and restriction of ocular motility, commonly known as scirrhous breast carcinoma.4-6 The response to hormonal therapy is favorable for patients with ER+, PR+ findings in the tumor tissue. Estrogen receptor assay results from orbital metastases can differ from those of the primary lesion, so any orbital tissue studies should include their own separate assay.5
A retrospective review from the Cogan Ophthalmic Pathology Laboratory of the Massachusetts Eye and Ear Infirmary analyzed histopathologic correlations of breast cancer that metastasized to the orbit; it found that lobular breast cancer represents the cancer subtype with the highest prevalence among orbital metastases.5,7 On immunophenotypical characterization, this was theorized to be due to the lack of intercellular cohesiveness in lobular breast cancers, because they lack the molecule E-cadherin. E-cadherin is normally expressed in many neoplastic cell types, including ductal breast carcinomas, limiting their dispersion.5 REVIEW
1. American Academy of Ophthalmology 2019-2020 Basic and Clinical Science Course, Section 07: Oculofacial Plastic and Orbital Surgery. Available at https://store.aao.org/2019-2020-basic-and-clinical-science-course-section-07-oculofacial-plastic-and-orbital-surgery.html.
2. Shields JA, Shields CL, Scartozzi R. Survey of 1,264 patients with orbital tumors and simulating lesions: The 2002 Montgomery Lecture, part 1. Ophthalmology 2004;111:5:997-1008.
3. Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Current Opinion in Ophthalmology 2007;18:5:405-413.
4. Valenzuela AA, Archibald CW, Fleming B, et al. Orbital metastasis: Clinical features, management and outcome. Orbit 2009;28:2-3:153-159.
5. Jakobiec FA, Stagner AM, Homer N, Yoon MK. Periocular breast carcinoma metastases: Predominant origin from the lobular variant. Ophthalmic Plastic and Reconstructive Surgery 2017;33:5:361-366.
6. Shields JA, Shields CL, Brotman HK, Carvalho C, Perez N, Eagle RC. Cancer metastatic to the orbit: The 2000 Robert M. Curts Lecture. Ophthalmic Plastic & Reconstructive Surgery 2001;17:5:346-354.
7. Raap M, Antonopoulos W, Dämmrich M, et al. High frequency of lobular breast cancer in distant metastases to the orbit. Cancer Medicine 2015;4:1:104-111.



