This year's glaucoma research covers a broad range of topics, from medications and surgery to associated factors, genetic influences and new approaches to diagnosis. (Unless otherwise noted, studies were conducted without commercial support.)
Factors That Impact Glaucoma
Researchers at the
Researchers identified all beneficiaries age ≥40 years continuously enrolled in a large managed-care network who made at least one visit to an eye-care provider between 2001 and 2007. ICD-9 billing codes identified individuals with OAG and those with components of metabolic syndrome. Cox regression was used to determine the risk of developing OAG in patients with components or combinations of components of metabolic syndromes. Adjustments were made for sociodemographic factors, systemic medical conditions and other ocular diseases.
Of the 2,182,315 enrollees who met inclusion criteria, 54,558 (2.5 percent) had OAG. After adjustment for confounding factors:
•Those with HTN (HR=1.35) or DM (HR=1.17) had an increased hazard of developing OAG relative to persons with neither of these conditions. Those who had HTN and DM in combination also had an increased risk (HR=1.48).
• The presence of hyperlipidemia in combination with HTN (HR=1.13) or with DM (HR=1.09) produced hazard ratios of lesser magnitude.
• Persons with hyperlipidemia alone had a 5-percent decreased hazard of OAG (HR=0.95) compared with those who had no components of metabolic syndrome.
The authors note that determining whether hyperlipidemia or the medications used to treat this condition reduce the hazard of OAG could lead to improved OAG treatment strategies.3974
Researchers at the
The data showed that NTG patients with a higher degree of myopia had bigger 24-hour fluctuation of IOP. Fluctuation was significantly negatively correlated with age (β=-0.008, r2=-0.035, p=0.034) and refractive error (β=-0.033 ,r2=0.046, p=0.015).563
Noting that Helicobacter pylori infection and NTG are both common among Koreans, researchers at three centers in
The NTG patients had significantly more positive serologic results than did the normal controls (Group I: 72 percent vs. 28 percent, p=0.018; Group II: 73.1 percent vs. 59.8 percent, p=0.008, OR=1.83). No significant association was found between clinical characteristics and a positive serologic result in NTG patients. The authors note that H. pylori may play a role in the development or progression of NTG as a secondary aggravating factor, or could be a primary cause.190
Glaucoma Medications
Researchers at two universities in
Researchers at the
A statistically significant reduction in mean CCT was observed in the latanoprost group (535.5 ±37.9 vs. 530.1 ±36.4 µm, p<0.001) but not in the control group (543.1 ±40.2 vs. 542.6 ±37.0µm, p=0.786). The authors note that CCT variations resulting from medical treatment could affect IOP measurement in NTG patients.179

Imaging
Noting the increased use of spectral domain optical coherence tomography in glaucoma assessment, researchers at multiple centers in the
The mean reflectivity of the RNFL was significantly lower in glaucomatous eyes than in healthy eyes: 0.506 (SE 0.015) vs. 0.619 (SE 0.015) (p< 0.01). Also, the contrast between the RNFL and the GCC was significantly lower in glaucomatous eyes than in healthy eyes: 0.123 (SE 0.011) vs. 0.232 (SE 0.011) (p<0.01). They conclude that the differences in contrast and reflectivity may impair accuracy and limit the use of SD-OCT in glaucoma management.212
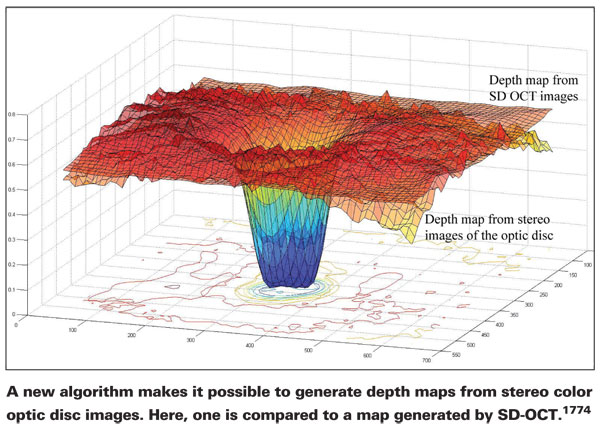
Researchers at the University of Iowa and Iowa Veterans Admin-istration Medical Center conducted a study to validate an algorithm they've created that's able to generate depth maps from stereo color images of the optic disc—a widely used, low-cost tool that has lacked a means of objective assessment. For validation they compared 30 depth maps and SD-OCT scans of the optic disc taken on the same day from both eyes of glaucoma patients. (See image, above.)
The root mean squared difference between normalized structures was 0. 1592. The automatically computed depth maps based on stereo color images of the optic disc faithfully reproduced the shape of the ONH generated by SD-OCT. The authors propose this method as a low-cost alternative to SD-OCT for diagnosis and management of glaucoma and other optic neuropathies.1774
Glaucoma and Daily Living
Researchers at multiple centers in the
The data showed that the highest level of physical activity was associated with lower IOP, lower BMI, lower systolic blood pressure and smaller waist/hip ratio.
The authors note that physical activity and weight control may offer a safe, simple method of reducing IOP.3977
Researchers in the National University Health System in
Twenty-three adult patients without glaucoma, ocular hypertension or any other conditions associated with raised IOP, who were able to lie recumbent in the supine and left lateral decubitus position, were recruited from general ophthalmology out-patient clinics. Mean age was 54 ±16 years. Ocular diagnoses included cataracts (30 percent), dry eyes (26 percent), blepharitis (22 percent), vitreous syneresis (13 percent) and other (9 percent). The IOP in the left eye of each patient was measured in the supine position using a Tono-Pen XL, immediately followed by a second measurement obtained in the left lateral decubitus head position. Measurements in both positions were obtained with the patient lying first on a soft pillow, then on a hard pillow.
The mean IOP in supine head position was 14.1 ±3.3 mmHg; the mean IOP in left lateral head position was 17.1 ±3.4 mmHg—a statistically significant change (p<0.001). The shift from soft to hard pillow made no difference in IOP in either head position. The authors note that this possible increase in IOP during sleep could lead to progression of glaucomatous optic neuropathy despite target IOP being achieved on examination at routine follow-up.558
Researchers at the University of Alabama at Birmingham conducted a study to evaluate the association between specific visual field characteristics and motor vehicle collision (MVC) involvement in 438 glaucoma patients (mean age: 72.8 years; 55.5 percent female, 60.5 percent white, the remainder black). All subjects had been seen at least once between January, 1994 and December 1995 in one of three university-affiliated ophthalmology and optometry practices. Investigators obtained information on use of glaucoma medications, BCVA in each eye, and visual fields (either a 30-2 or 24-2 test) in each eye. Binocular visual field measures (created by averaging individual eye measures) were stratified into nine regions, and average threshold (TH), total deviation (TD) and pattern de-viation (PD) values were obtained. Finally, demographic, driving, health and other information was obtained via a telephone survey, and information regarding all MVCs that occurred between January 1994 and June 2000 was obtained from the Alabama Department of Public Safety.
Over the entire visual field TH, TD and PD impairment was associated with a non-significant 50-percent, 44-percent and 68-percent increase in the rate of at-fault MVCs, respectively. However, once the visual field was separated into regions, significantly increased rates were observed for certain locations (i.e., the inferior region) and were limited to specific measures (i.e., TD and PD). The authors note that this data might provide clinicians with a set of markers to identify glaucoma patients at risk of motor vehicle collision involvement.3986
Improving Glaucoma Surgery
One of this year's abstracts presents two-year follow-up results from the Ahmed vs. Baerveldt Study, a multicenter, randomized clinical trial comparing the Ahmed-FP7 valve to the Baerveldt-350 implant for treating refractory glaucoma. In the study, 250 patients at least 18 years old with uncontrolled glaucoma refractory to medical, laser and surgical therapy were randomized to receive either an Ahmed-FP7 valve (n=129) or a Baerveldt-350 implant (n=121) using standardized surgical technique.
Results at two years included:
• Mean IOP was 14.4 ±6.7 mmHg in the Ahmed group and 13.7±4.9 mmHg in the Baerveldt group (p=0.58).
• Mean number of glaucoma medications was 1.43 ±1.49 in the Ahmed group and 0.77 ±1.06 in the Baerveldt group (p=0.012).
• The cumulative probability of failure was 48.4 percent in the Ahmed group and 44.2 percent in the Baerveldt group (p=0.78).
• 22 patients (17.1 percent) in the Ahmed group had complications which required intervention, compared to 31 patients (25.6 percent) in the Baerveldt group (p=0.098).
Overall, at two years the two groups had similar success rates, IOPs and VAs, and required a similar number of interventions to treat complications of surgery. However, the Ahmed group required a greater mean number of glaucoma medications than the Baerveldt group.4443
Researchers at two universities in
The data showed:
• IOP immediately pre- and post-needling was 24.1 ±5.8 mmHg and 10.4 ±5.6 mmHg, respectively (p<0.001).
• Success of needling was 63 percent at one month, 53 percent at six months and 41 percent at 12 months.
• Factors correlating to needling failure included: non-Caucasian race (p=0.003, RR=1.8); re-op trabeculectomy (p=0.05, RR=1.6); history of previous needling (p<0.001, RR=2.1); IOP >25 mmHg before needling (p<0.001, RR=2.0); IOP >12 mmHg after needling (p<0.001, RR=2.0); and resumption of glaucoma meds post-needling (p<0.001, RR=2.2).611
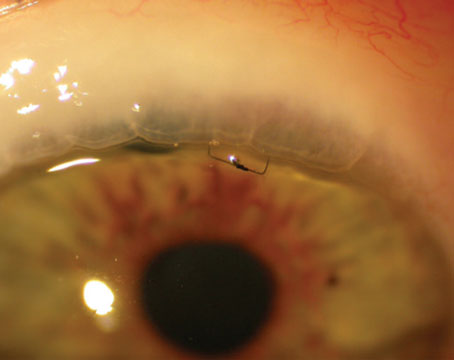
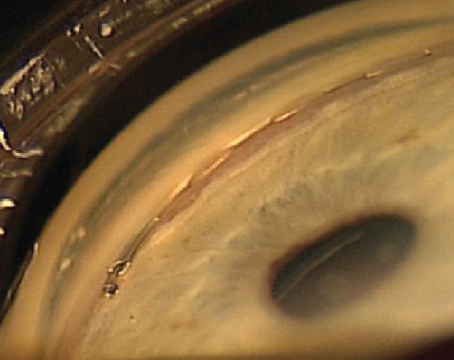
Researchers at the University of Virginia conducted a retrospective, interventional, noncomparative case series to describe surgical applications and clinical outcomes of 10 consecutive patients (mean age 47) who underwent primary or secondary glaucoma surgery in one eye using sterile, irradiated cornea allograft.
The grafts were used to cover a primary glaucoma tube shunt in three patients; to cover a revised or repositioned glaucoma tube shunt in five patients; for tectonic support of a revised trabeculectomy flap in one patient; and to cover subconjunctival prolene sutures following a surgical iridoplasty in one patient. Allografts were either full-thickness (n=5) or split-thickness (n=5). Mean follow-up was 10 months (r: 8.2 to 12.6 months).
No case required revision of the allograft. The allografts demonstrated good biocompatibility in all 10 cases during the follow-up period, as evidenced by maintained clarity of the corneal tissue, absence of clinical signs of immunologic rejection or ocular inflammation, and integrity of the sterile cornea and the conjunctiva over the graft. Cosmetic results were excellent, and there were no complications during the follow-up period.600
The Family Connection
Researchers at
The data showed:
• Of the 332 PAC patients, 83 (25 percent) had a family history of glaucoma. Characteristic-adjusted odds ratio of family history for PAC was 4.82; OR for severity was 1.61.
• The presence of first-degree relatives with glaucoma contributed to the odds of having PAC (OR 5.09), as did the number of first-degree relatives (OR 4.71). However, among first-de-gree relatives, only parents contributed to the odds of having PAC (OR 8.76)—not siblings or offspring.
• Of the 228 POAG patients, 49 (21.49 percent) had a family history of glaucoma (OR 8.38); OR for severity of POAG was 1.81.
• Both the presence and number of first-degree relatives with glaucoma contribute to POAG (OR 7.28 and 6.61, respectively). However, unlike PAC, only siblings and offspring with glaucoma contributed to the odds of having POAG (OR 8.99 and OR 19.23, respectively)—not parents.2764
Researchers at two centers in the
After a mean follow-up duration of 11.5 years (SD 2.0; r: 7.4 to 13.7 years), four participants with GVFL were identified (mean age at follow-up, 59 years): three incident cases and a single subject who already had GVFL at baseline, for a prevalence of 4.3 percent in this group—significantly higher than the prevalence of 0.7 percent in the general population of similar age. The incidence rate and 10-year risk of GVFL were 2.8/1000 person-years and 2.8 percent respectively. Factors associated with GVFL were: high myopia (p=0.003); IOP (p=0.032); IOP treatment (p=0.004) and linear cup-to-disc ratio (p=0.009).
The authors note that although being an offspring of a glaucoma case does appear to be a risk factor for developing visual field loss, a 10-year risk of only 2.8 percent suggests that examinations of offspring can be widely spaced in time.3979
The Cornea Connection
Researchers at two American universities, along with the Ocular Hypertension Treatment Study Group and European Glaucoma Pre-vention Study Group, conducted a study to determine whether adjusting baseline IOP for corneal thickness actually does increase the accuracy of the prediction model for the development of POAG from the Ocular Hypertension Treatment Study and the European Glaucoma Prevention Trial. (This study was supported by multiple non-commercial grants along with grants from Merck, Pfizer and RPB.)
The authors ran the same Cox proportional hazards model using each of five published correction algorithms, changing only whether or not IOP was adjusted for CCT. They found that, in the models that included IOP adjusted for CCT, the C-indices ranged from 0.763 to 0.770—no better than the original prediction model (0.774). When CCT was added to models in which IOP was adjusted for CCT, CCT still made a statistically significant improvement.
The authors conclude that calculating individual risk for the development of POAG is simpler and just as accurate using IOP and CCT as measured, as when applying an algorithm to correct IOP for CCT.2708
Researchers at the University Eye Hospital Freiburg, in
The data showed a highly significant association between corneal hysteresis and IOP: CH decreased as IOP increased. The authors note that this data suggest that the CH as measured by the ORA is not an independent biomechanical property of the cornea. Either CH itself is dependent on IOP, or the ORA is incapable of measuring CH accurately at higher IOP levels.5553
Researchers at three centers in
The data showed:
• Progressing eyes had thinner CCT (525.0 ±34.2 vs. 542.3 ±38.5 µm, p=0.04) and lower CH (7.5 ±1.4 vs. 9.0 ±1.8 mmHg, p<0.01) compared to nonprogressing eyes.
• CH and CCT correlated significantly (Pearson's r=0.33, p<0.01).
• Older age (OR=1.04, p=0.04), CH (OR=0.63, p<0.01), and mean follow-up IOP (OR=1.24, p<0.01) were significantly associated with VF progression.
The authors note that because CH is associated with increased risk of VF progression and may describe corneal properties more completely than thickness alone, it may be a better parameter to assess the risk of progression.4025
New Diagnostic Tools
Researchers at
Both groups underwent visual field testing using the Humphrey Perimeter (Central 24-2 SITA-FAST). While in front of the perimeter, they underwent photostress testing with a standard 60-watt white light bulb 50 cm from the eye. In addition, Stratus OCT was used to determine thickness of the central macula and retinal nerve fiber layer.
The data showed that all eyes in the glaucoma group had lower foveolar threshold values (p<0.001) and longer recovery times (p<0.001) than the controls. No significant correlation existed between CMT and recovery time, but there was a moderate correlation between RNFL and recovery time (p<0.01). The authors note that photostress testing may be useable as a functional biomarker of glaucoma.5492
In hopes of finding a screening test for glaucomatous optic nerve damage that's quick, inexpensive and easily performed by trained allied health-care workers, researchers at Stanford University School of Medicine conducted a study to see whether testing relative afferent pupillary defect (RAPD) using a swinging flashlight could be an effective tool for glaucoma screening. Non-ophthalmic personnel masked with regard to disease presence examined 107 subjects recruited from a mixed population of glaucomatous and non-glaucomatous patients. All subjects underwent a swinging flashlight test with, when necessary, the aid of neutral density filters, to determine whether or not a RAPD was present. Medical charts were subsequently reviewed to grade disease stage.
Statistical analysis found an OR of 9.71 for glaucoma if RAPD was present, with a sensitivity of 66.7 percent and a specificity of 82.9 percent. A planned subanalysis of phakic study subjects revealed an OR of 17.05 for glaucomatous disease if RAPD was present, with a sensitivity of 68.8 percent and a specificity of 88.6 percent. Sensitivity, specificity and predictive value was greater for phakic subjects than for the overall group, which included those who had previously undergone cataract surgery.183
Dr. Netland is professor and chairman of the department of ophthalmology at the