IOL calculation formulas have undoubtedly improved over time, helping surgeons’ accuracy and fostering patient satisfaction. However, as every surgeon knows, there still exists a subset of eyes that make calculations a little less predictable, leading to poorer outcomes. Among those categories surgeons often find challenging are long and short eyes, post-corneal refractive eyes (RK, LASIK, PRK), keratoconus and post-keratoplasty, to name a few. We asked several cataract surgeons how they approach these patient presentations and which IOL formulas show the most reliability for getting close to your target.
Understanding the Challenges
Certain factors such as anatomy, corneal power and refraction are just some of the data to consider when calculating IOL power, but the information is a bit more difficult to measure in challenging patient presentations.
Dagny Zhu, MD, a cornea, cataract and refractive surgeon practicing in Rowland Heights, California, says there are three variables that contribute to these challenging IOL calculations.
“We still have sources of error when it comes to predicting where the lens will sit,” Dr. Zhu says. “The final effective lens position is really hard to predict in complex eyes, although it’s better than ever before with our modern-day formulas. Short eyes are the most difficult to predict the effective lens position because of the anatomy of the eye, and it can change based on the anatomical features, including the ACD and the lens thickness.
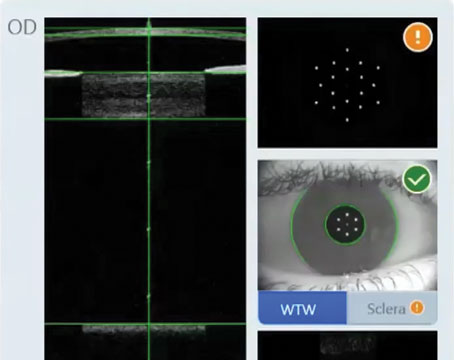
“The other one is corneal power,” she continues. “Not only is corneal power difficult to measure because there’s often ocular surface disease that can make it hard to get consistent, accurate measurements, but especially in post-refractive eyes, if they’ve had LASIK, PRK, or RK, it’s hard to measure the true total corneal power. All you can do is estimate it using topography to measure the anterior curvature, which ends up being more variable in these post-refractive eyes. This can then be used along with other factors to calculate a predicted posterior corneal curvature. The other option is to directly measure the posterior corneal curvature using a Scheimpflug device or swept-source OCT biometer, which is still not perfect. The ELP is also based on total corneal power, so all of that ties together and kind of confounds each other.
“And then the last variable I’d say is that these complex eyes are very difficult to refract in general,” Dr. Zhu says. “There’s a lot of fluctuation, especially with advanced keratoconus eyes, and so it becomes difficult when you’re trying to fine tune your personal surgeon A-constant. All of these variables can hinder your ability to improve the consistency and accuracy of your refractive outcomes.”
Recent formulas have been able to improve on earlier standards, which could lead to a myopic or hyperopic shift in atypical eyes. There are regression formulae (second generation) such as SRK II, vergence formulae (third generation) such as Holladay I and II, Hoffer Q, Haigis and Barrett. “Regression formulae such as SRK II make a lot of assumptions, and may fail to deliver in atypical eyes,” says Nicole Fram, MD, who is the managing partner of Advanced Vision Care in Los Angeles. “For example, in short eyes, if you use the assumptive standard, first/second-generation formulas, you’ll end up more myopic than expected because the effective lens position is more anterior than expected. Luckily, we have new AI generation formulas that aren’t just simply regression or vergence formulae. Now, they can look at the variables that are most sensitive to effective lens position and use artificial intelligence to achieve better outcomes by inputting more and more data.”
There are some proactive steps to take for all eyes to improve refractive accuracy, not just complex eyes, say experts. “You want to optimize the ocular surface,” says Dr. Zhu. “I put all my patients on preservative-free artificial tears every hour, usually a lubricating ointment at night and have them start twice-daily lid scrubs and warm compresses. Sometimes I’ll start them on a low-potency steroid as well and maybe even an immunomodulatory agent like cyclosporine or lifitegrast if they have more advanced ocular surface disease. I will have them follow this regimen for at least two weeks, and then repeat many of the preoperative measurements.”
Douglas D. Koch, MD, professor and Allen, Mosbacher, and Law Chair in Ophthalmology at the Cullen Eye Institute, Baylor College of Medicine in Houston, asks his patients to follow a similar regimen. “They use preservative-free artificial tears four times a day, and lid scrubs and warm compresses at night in the two weeks before they come in for their measurements,” he says. “I’ve found that the reproducibility of the measurements has really improved. I think the importance of that is magnified in these eyes with any kind of irregular cornea, such as the post-LASIK, post-RK, post-keratoplasty and keratoconus.”
Dr. Zhu adds not to be shy on the amount of measurements either. “Try to take as many measurements as possible, at multiple time points and with as many devices as possible,” she says. “The more data points you have, the more likely you are to hit the correct target. All of my preoperative patients are measured using two different biometers and one or two Scheimpflug or Placido disc topographers. All of that helps me to decide what the most accurate Ks are, as well as the most accurate astigmatism magnitude and axis, and as long as they all agree, you can be pretty certain that you’ll hit the target.”
 |
|
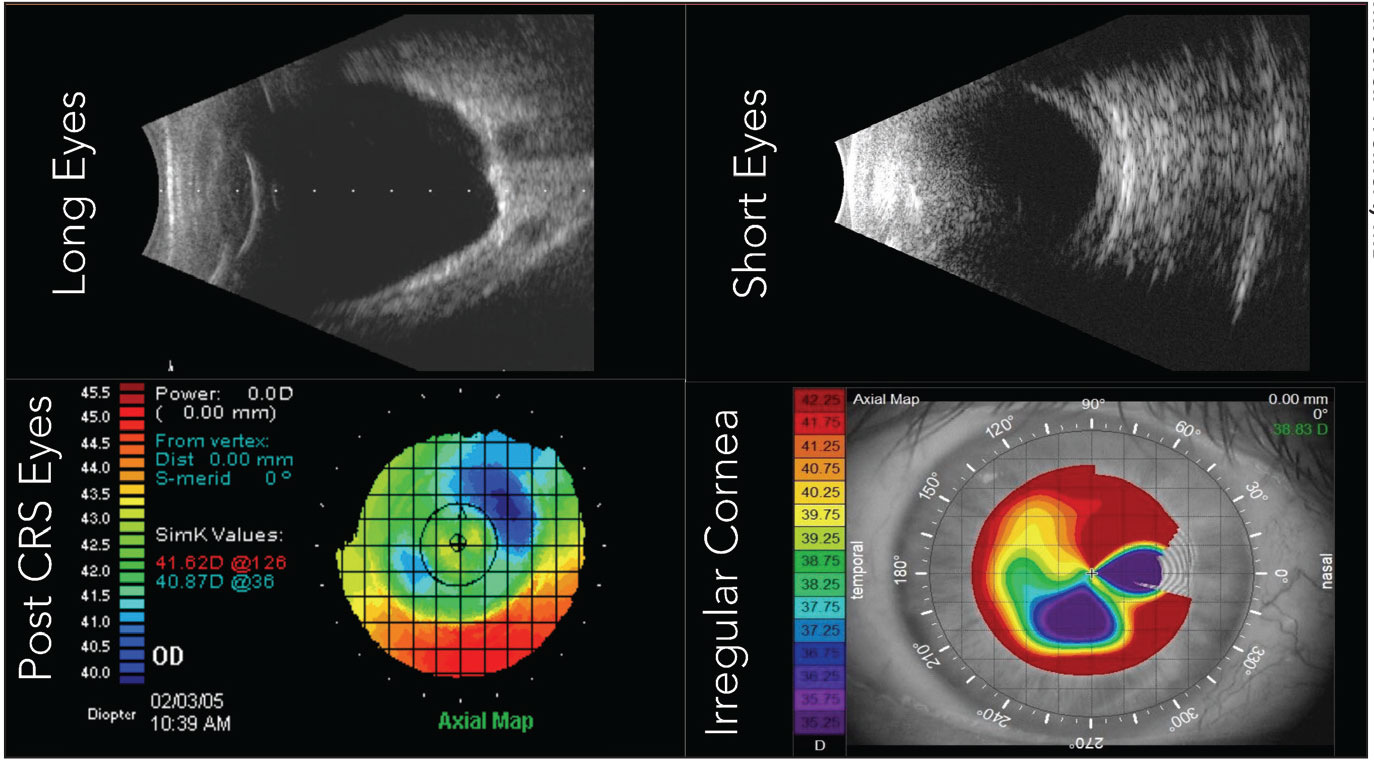
Some of the most challenging categories of eyes include long and short eyes, post-corneal refractive and keratoconus. Studies have shown that certain IOL formulas are a better fit than others depending on the patient presentation. (Image courtesy of Mitchell Weikert, MD.) |
It’s also a good idea to explain the situation to patients to help them understand why they need to do this additional prep.
“These patients always warrant a longer preoperative discussion and counseling,” Dr. Zhu says. “We often tell patients that their eyes aren’t within the normal range and are more of a special case so we’re going to take special care of their eyes by doing extra optimization of their ocular surface before surgery and taking multiple measurements. After surgery—even after all the careful and special calculations that we do—we ultimately explain that the way their eye heals is unique to them and there’s no way anyone can predict that—only God would know.
“We counsel them on the small chance that if they’re off, we’ll have to do a touch up with laser vision correction or even an IOL exchange, or, if we’re using the Light Adjustable Lens, I’ll explain that process,” she continues. “But this way they know that we’ve done all that we can and the remaining variable is on them. They’re pretty understanding when we explain it that way. Also the extra effort on their part preoperatively to do all the treatments and the measurements shows that we’re in this journey together. They understand that they have some responsibility in this as well.”
Finding the Right Formula
Many of the most commonly used formulas have been tested by time and validated in large studies. And while the newest generation of formulas, several of which harness artificial intelligence, are far and away better than the early generations, surgeons still find themselves falling short of the target in certain eyes and say there’s room for improvement.
Dr. Koch says short eyes and post-refractive eyes particularly don’t get great results. He has two papers coming out, co-authored with Mitchell Weikert, MD, showing that results for short eyes are less than 75 percent within 0.5 D of target, and another paper on post-LASIK eyes. “If you look at the literature, almost all studies show that the percentage of eyes within 0.5 D of target is less than 75 percent,” Dr. Koch says. “We have a paper coming out (with Dr. Weikert) showing that again, we’re getting about a little over 70 percent within 0.5 D of target with one of the Barrett formulas. But again, these data are disappointing.”
In the post-LASIK category, Dr. Koch says there probably are three reasons that IOL calculations are inaccurate with today’s technology. “The first one being the prediction of the effective lens position, the second one being corneal power and the third one being any error introduced by refraction,” he says. “All three of those are actually accentuated in the post-LASIK eye. The ELP is more complicated because most formulas for ELP use corneal power as one of the variables, and of course the corneal power has been modified. Corneal power as a source of error is present because the anterior cornea has more asymmetry, more higher order aberrations, more irregularity, making it harder to figure out what the ‘true power’ is. Also the anterior corneal power doesn’t accurately predict what the posterior corneal power will be, so that induces error. Their refractions are more variable, they’re softer endpoints. This is a situation where we do okay with standard formulas—if you’re happy with 75 percent within a 0.5 D of target—but to get better with what we have now, we’re looking at postoperative modification.”
So, what are the formulas that work best in these complex eyes? Here’s what our experts had to say:
• Long eyes. This is one category where experts say they do well. “That problem became really alleviated when Li Wang, MD, came up with the idea of optimizing the axial length,” says Dr. Koch.
In 2011, Dr. Wang co-authored a study that evaluated the accuracy of four IOL formulas in eyes with axial length greater than 25 mm.1 Eyes were randomized into two groups: one used to develop the method of optimizing AL by back-calculation; the other used for validation. In the validating group, the method of optimizing AL significantly reduced the mean numerical errors for IOLs greater than 5 D from +0.27 to +0.68 D to -0.10 to -0.02 D and for IOLs of 5 D or less from +1.13 to +1.87 D to -0.21 to +0.01 D, respectively (all p<0.05). The method significantly reduced the percentage of long eyes that were left with a hyperopic outcome.
“Other formulas have been catching up to that,” continues Dr. Koch. “Long eyes should actually do quite well these days with current formulas. One of the reasons that you would expect them to do well is because the IOL power is low so the error created by the effective lens position should be diminished because a low-powered IOL moved in one direction or the other has much less impact on the outcome than an IOL that has higher power.”
Dr. Fram says her favorite formuls for long eyes are the Wang-Koch adjustment, Barrett Universal II and Hill RBF. “By using the Wang-Koch adjustment formula for >26 mm eyes, we’re hitting our refractive targets upwards of 90 percent,” Dr. Fram says. “I also look at the Hill-RBF, the Barrett, the regression formula for Holladay, and Zeiss AI, but my most accurate moments are with the Wang-Koch adjustment. Kane is also an excellent choice. When you do hyperopic biometry calculations, the biometer will assume that the eye is longer than it is and you’ll put in a lens that’s less powerful, and then you end up with a hyperopic error and that’s the heartbreak of any myope. It’s helpful to look at different types of formulae and mechanism of action for increased consistency in these challenging eyes.”
Dr. Zhu favors the Barrett II Universal, Kane, EVO and Hill-RBF for long eyes. “The Hill-RBF in particular is nice because it actually uses big data and AI to come up with the lens prediction,” she says.
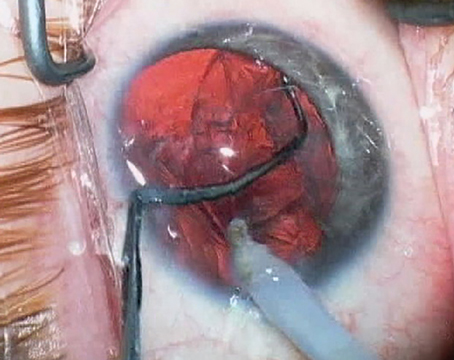
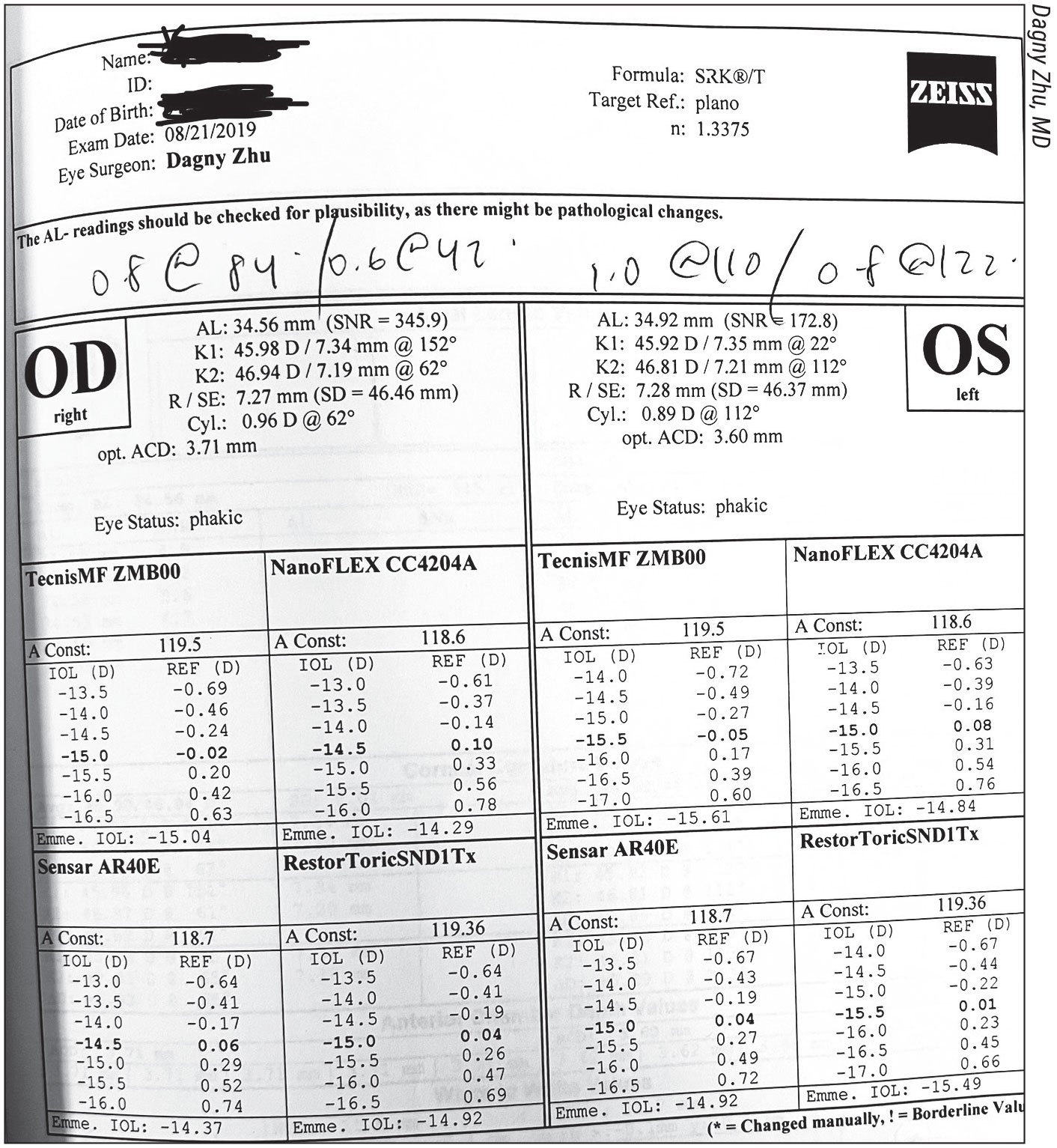
She’s grateful for the evolution of these formulas. “I remember when I first started clinical practice and [one patient] had the longest eye I’d ever seen,” Dr. Zhu recalls. “The patient was a -30 D refraction, and his axial length was almost 35 mm. In training, we were still taught to use the very old SRK/T formula for long eyes, so that’s what I used. Thankfully, the IOL didn’t even come that low in powers, so I couldn’t even use the one that I calculated. I ended up using a higher power lens, which ended up getting me exactly where I wanted to be. I lucked out, but I ended up taking that case and back-calculating what the predictive power would have been for every formula, and in retrospect, I found that the Holladay 1 (with Wang-Koch adjustment), Kane and EVO would have been the most accurate, although the Barrett II and Hill-RBF would also have gotten me to within -0.5 D. Using the actual lens power calculated by SRK/T would have made the patient almost 3 D hyperopic. The modern-day formulas take into account the effective lens position and also the posterior corneal power, which are all very helpful for extreme eyes.”
• Short eyes. The other side of the coin is the short eye, says Dr. Koch, which requires a high powered IOL. “The short eye has a wildly variable anatomy, ranging from a small corneal diameter to a shallow anterior chamber to a relatively normal anterior segment for any given axial length, so there’s a lot of variability,” he says.
As referenced earlier, Dr. Koch and others from Baylor published a paper in the Journal of Cataract and Refractive Surgery looking at 15 formulas for short eyes (22 mm axial length or smaller).2 The study included 278 eyes and used two axial length values: (1) machine-reported traditional AL (Td-AL) and (2) segmented AL calculated with the Cooke-modified AL nomogram (CMAL). It concluded that the Zeiss AI IOL calculator outperformed Barrett, Pearl-DGS and Kane. The Cooke-K6 formula outperformed some formulas depending on parameters.
“We found that this new formula, the Zeiss AI IOL calculator, actually came out best in terms of mean absolute error and in terms of the percentage of eyes within 0.5 D of target,” he says. “Unfortunately, even though it was best, it was still less than 75 percent within 0.5 D of target. The other formula that actually turned out quite well was the Cooke-K6 formula. In some respects that was almost as good as the Zeiss AI. But those aren’t great results.”
Dr. Fram says she’s excited about the potential of the AI formulas. “We’re getting better and better, but the reality is, we were only hitting our targets on short eyes about 65 percent of the time with non AI formulae, and patients routinely end up myopic which they aren’t accustomed to, causing discontent,” she says. “It’s really challenging, especially with refractive lens exchange. These are often hyperopes that do the best and we’re putting in a multifocal. We need to be able to hit our refractive targets. Fortunately, we’re improving outcomes with new generation formulae. Refractive outcomes are closer to 80 percent within +/- 0.50 D in small eyes using formulas such as the Hill-RBF, the Zeiss AI and the Cooke-K6 formula. We’re in a much better place.”
• Post-refractive eyes. “When you enter into calculating IOLs for post-refractive eyes, it becomes even more challenging because these are people that expect the same outcome from corneal refractive surgery with their cataract surgery,” says Dr. Fram. “What I explain to the patient is that someone has manipulated their cornea and because of that, the formulas that we normally use aren’t as accurate. And they still look at me like, ‘Yeah, but you’re going to hit your target, right?’ The ASCRS and ESCRS calculators will create an average from many formulae to help in these post-refractive eyes and are critical to picking IOLs.”
Running various formulas through a platform such as Veracity or the ASCRS calculator can be beneficial for these eyes, say experts. “For the post-refractive eyes, whether it be LASIK or PRK, we run the Barrett on the Veracity and we also run the ASCRS calculator which gives us several formulas and look at those,” says Dr. Koch.
“I do look at the average of the ASCRS calculator, but the Barrett True K is really incredible,” Dr Fram says. “When we look at the Barrett True K in our office, we’re hitting our targets about 83 percent of the time within +/-0.5 D. Usually it’s between 65 and 74 percent of the time. In the literature, there’s a Barrett True K TK formula that shows even more promise; it looks at the posterior corneal curvature that can be measured either with Pentacam, Galilei or anything that measures posterior cornea, or you can use the IOLMaster 700 (Zeiss), which has built-in PK1 and PK 2. We’re currently looking at that and it looks like it gives us about a 4-percent advantage, although we’re still examining the data. It’s taking us from 83 percent on target to 87 percent. That little bit does matter when you think about how many patients you operate on in a year, and so, Barrett True K TK is still taking us to an even better level in terms of hitting our targets.”
Dr. Zhu uses the Barrett True K for post-refractive eyes as well, in addition to the EVO.
Dr. Fram also uses intraoperative aberrometry for post-refractive cases. “At AAO we reported a paper looking at over 1,000 eyes of Barrett True K vs. intraoperative aberrometry formulae and intraoperative aberrometry did better than Barrett True K—approximately 76 percent vs. 69 percent within 0.5 D,” she says. “I still use ORA for these cases as this is constantly being optimized with big data.”
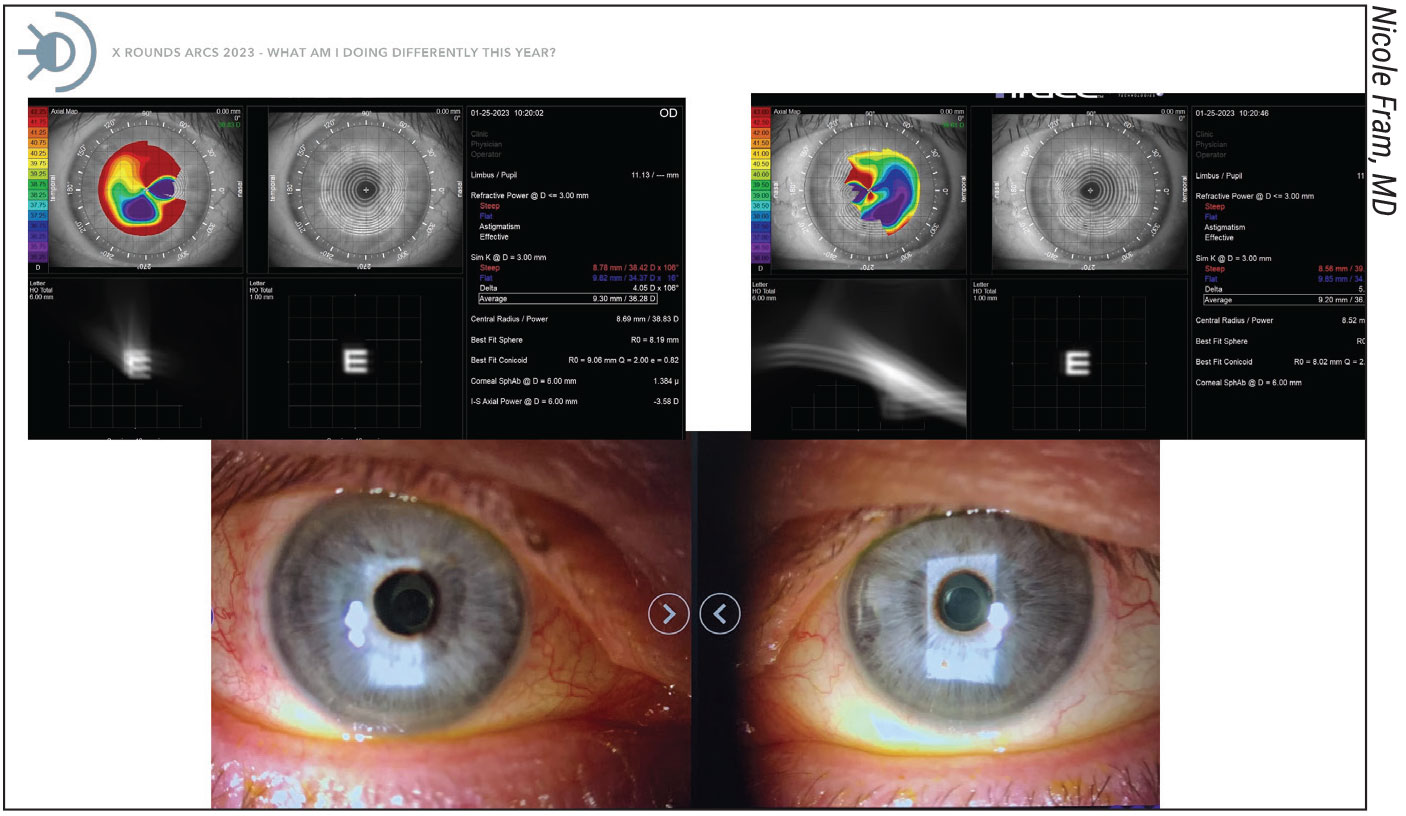 |
|
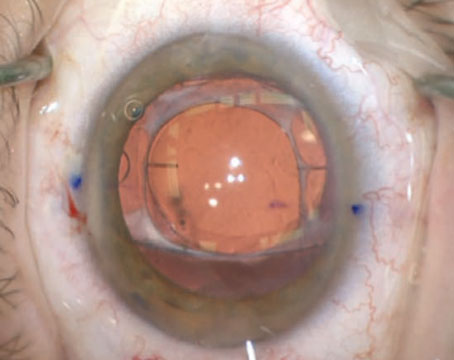
New IOLs such as the Apthera/IC-8 may help surgeons get closer to their refractive target in eyes with irregular astigmatism, post-RK and keratoconus, say experts. |
• Keratoconus. Many of the same formulas that have success in post-refractive eyes also work for keratoconus. “For keratoconus, I like to use the Barrett True K, which has a keratoconus mode—it’s most accurate when you put in the actual measured posterior corneal curvature powers,” says Dr. Zhu. “And Kane keratoconus also has a special keratoconus feature for its IOL formula. EVO also is good for keratoconus, especially when you put in the measured posterior corneal curvature powers.”
Dr. Fram says it’s not unusual to end up with a hyperopic outcome because of underestimating the cornea. “A lot of people in the past would just use SRK/T and aim -1, which is pretty arbitrary, but Kane and Barrett have keratoconus formulas that are performing really well,” she says. “They’re still only approximately 60 to 65 percent on target, but at least it’s an improvement in this challenging population.”
“For keratoconus formulas, we released a paper in the Journal of Refractive Surgery,” says Dr. Koch. “What we found for keratoconus is that the new keratoconus formulas, Barrett-KC and Kane-KC do quite well in keratoconus eyes when the corneal power is less than 50 D—getting within approximately 70 percent within a 0.5-D target.3 But once the corneal power is 50 and up, then the accuracy falls way off and we’re talking about less than 20 percent within a 0.5 D. You can argue that you should use the Light Adjustable Lens for these eyes, and that’s certainly a possibility.
“The problem with the keratoconus eye and also for the RK eyes is the question of stability,” he continues. “Are they going to change over time? That’s one of the unknowns. It doesn’t mean you shouldn’t try to be as accurate as you can the first time around but you can’t promise the patient this will last indefinitely.”
IOL Selection and Patient Counseling
Surgeons should give consideration to which lens is going into these challenging eyes. Much like the formulas, some IOLs are a better fit than others.
“In these eyes I would typically end up using a monofocal lens,” says Dr. Zhu. “I’m not going to use a multifocal lens in eyes with any sort of irregular astigmatism or higher order aberration, which can commonly be seen with keratoconus or post-refractive eyes. But if some eyes have very mild forme fruste keratoconus and regular astigmatism, I’ll still consider using a toric lens, maybe even an EDOF toric lens. It’s similar for post-refractive eyes, if the ablation is well-centered, and if it didn’t induce a high level of higher order aberrations, I’m comfortable using EDOF and even multifocal lenses in post-myopic and post-hyperopic LASIK eyes. I’ve looked at my own outcomes and I’ve had pretty good results with those types of patients as long as I screen properly. The eyes still have to be relatively regular.”
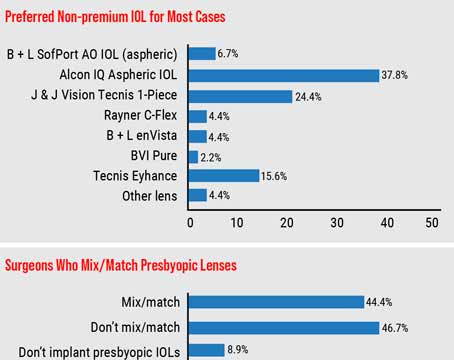
In post-myopic LASIK eyes, Dr. Fram says she prefers to use a lens with some negative spherical aberration to match the positive spherical aberration of the cornea or to mitigate it. “The Tecnis Eyhance (Johnson & Johnson Vision) or the LAL are my favorite lenses for post-myopic LASIK,” she says. “For post-hyperopic LASIK, I use a lens that has zero spherical aberration profile or very minimal in the center, so I’ll use an MX60 enVista or the LI61AO (Bausch + Lomb), or I’ll do LAL, and that’s been a great approach. The Zeiss CT Lucia 621 is also a really excellent lens for any type of eye.
“I rarely choose a diffractive technology in post-LASIK eye with abnormal topography such as decentered ablation or irregular Placido imaging because if they have dysphotopsia afterward, I’m not going to know what’s coming from the cornea and what’s coming from the lens, and it becomes a bit complicated. These eyes may benefit from a small aperture technology,” she continues.
“For long and short eyes, you’re limited based on what IOL power is available,” says Dr. Zhu. “A lot of the multifocal lenses don’t go very low or very high. They’re usually around 10 to 30 D and the astigmatism is limited as well, correcting up to approximately
3 D, or 2.5 D for against-the-rule astigmatism. So in those cases, you’re kind of stuck with using a monofocal.”
Patients should also be counseled on outcomes, especially for long and short eyes. “I think the only caveat with short eyes is that when we’re planning an EDOF or a multifocal lens, you want to make sure that patients understand that there’s a risk of being off target and they may need an IOL exchange, or, if you’re really off target, a laser vision enhancement,” says Dr. Fram. “As far as IOLs, I always use what’s in the patient’s best interest and I use every different type of IOL.
“The same goes for long eyes, but if they have a history of retinal detachments, or retinal detachments in their family, I’ll try to avoid silicone if I can because if they have a retinal detachment and it’s not amenable to repair with laser and gas, they may need silicone oil in the future,” she continues. “But if silicone is the best lens for them for a variety of reasons, I still use it.”
 |
|
This patient presented with an extremely long eye, with an axial length of almost 35 mm. At the time, Dagny Zhu, MD, used the SRK/T formula to calculate the lens power, but she didn’t end up using it because the patient would have been left nearly 3 D hyperopic. Newer generation formulas take other variables into account that help reduce the chance of hyperopic or myopic shifts. |
Newer IOLs, including the LAL and Apthera/IC-8, are contributing to accuracy in these eyes, say these experts. “We do have newer IOLs that provide even greater accuracy in these complex eyes,especially with the LAL, which allows you to tweak a final refraction after surgery,” says Dr. Zhu. “I have found the LAL to be my go-to for post-RK eyes and some of my post-refractive eyes in which they’ve had large ablations and I’m worried about missing the target by a large magnitude.”
“I was very interested in the LAL for post-LASIK patients,” says Dr. Fram. “I was very motivated to see if the technology would help us hit our refractive targets. If you have a myopic ablation, then you can end up hyperopic because the cornea is overestimated. If the corneal power is overestimated, you won’t put in as powerful of an IOL and you can end up hyperopic. When you work with the LAL, you don’t have to worry about that because you can adjust afterward. In hyperopic LASIK, the cornea is underestimated and you can put in a lens that’s too powerful because the cornea is steeper than was assumed and so, in that scenario, the patient ends up too myopic. I don’t have to worry about that when using the LAL. However, with post-hyperopic LASIK you want to be a little bit careful with the LAL because if you have a lot of negative spherical aberration in the cornea and then you add a negative spherical aberration lens, there can be issues. But, in general, the goal of hitting your target with a post-LASIK patient is the priority.”
Dr. Fram cautions surgeons about using the LAL on post-RK eyes. “You can use it but the patient needs to have normal Placido imaging,” she says. “If they don’t have normal Placido imaging, they’re still going to need a lot of help with higher order aberrations and the LAL doesn’t correct higher order aberrations. I’ll use the iTrace to help me decide, am I going to put a LAL in this patient, or am I going to put an IC-8?”
Although this lens has been doing well, Dr. Zhu says surgeons shouldn’t consider it to be the solution to every challenging eye. “I think that we have to acknowledge that the LAL is an extra expense for the patient, as well as quite a bit of extra time that they have to dedicate postoperatively,” she says. “We shouldn’t neglect all of our preoperative due diligence of having to treat the ocular surface and get multiple measurements whenever possible, because a lot of times people are just relying on the LAL knowing it can be adjusted postoperatively so they’re almost abandoning all of the traditional good practices. A lot of patients can still get excellent outcomes by using some of the traditional formulas by doing that preoperative due diligence, and using the modern-day formulas even for complex eyes.
“I don’t want people to think that a LAL is the only way to go, especially because it’s such a huge financial investment and not a lot of practices or surgeons are able to afford it,” Dr. Zhu continues. “This lens also adds a bit of negative spherical aberration so I would caution using it in the eyes that already have a large amount of existing negative spherical aberration, such as post-hyperopic LASIK eyes, because it may affect the visual quality. There have been a few cases of IOL exchanges with a LAL because of visual quality issues, but thankfully it’s been rare, and overall, I’ve had a very positive experience with it.”
Dr. Zhu says the Apthera/IC-8 can be considered for eyes with irregular astigmatism, post-RK and keratoconus. “Any eye that’s more severe will do well because the pinhole is going to improve the best corrected visual acuity, which the LAL doesn’t do,” she says. “The LAL only gets you to a more precise refractive outcome, but it’s not going to improve the quality of vision. The IC-8 has the advantage of both offering more flexibility in terms of the landing zone so you can be a little bit off and it’s still forgiving because of that pinhole, but it also improves the visual quality because of the pinhole effect. I tend to reserve the IC-8 for more irregular eyes and I’ll use the LAL for eyes that I think are relatively regular and have good potential for the patient to still be happy with their final outcome.”
Dr. Fram says, “We’ve been very successful using the small aperture IC-8 in RK patients, but I think the key with that lens is to make sure the patient understands that they may have a little bit of dimming because it’s a small aperture lens and it’s supposed to be in the non-dominant eye and it’s off-label for irregular corneas.”
A preop pilocarpine test may help determine if the IC-8 is the right way to go, says Dr. Fram. “You don’t want to use the IC-8 if you test a patient preoperatively and a pinhole obscures their vision because of a scar or if you put pilocarpine in and they don’t see any improvement,” she says. “The pilo test will mimic what the IC-8 does with the small aperture. So, how do I target that lens? For an eight-cut RK, which is the most common, I’ll aim -0.75 to -1 D using the Barrett True K and the ASCRS calculator on RK because the small aperture lens—when targeted myopic—did best in the clinical trials for mini-monovision. You always want to hedge a little bit more myopic in post-RK eyes because you can get a hyperopic shift over time. Some will do topo-guided PRK after for enhancement. The IC-8 has been a huge advancement for these challenging patients and patients where you want to avoid diffractive technology.”
Dr. Fram consults for Zeiss. Dr. Koch is a consultant for Alcon, Johnson & Johnson Vision and Zeiss. Dr. Zhu consults and does research with Alcon, and consults for Johnson & Johnson Vision and Bausch + Lomb.
1. Wang L, Shirayama M, Ma XJ, Kohnen T, Koch DD. Optimizing intraocular lens power calculations in eyes with axial lengths above 25.0 mm. J Cataract Refract Surg 2011;37:11:2018-27.
2. Kenny PI, Kozhaya K, Truong P, Weikert MP, Wang L, Hill WE, Koch DD. Efficacy of segmented axial length and artificial intelligence approaches to intraocular lens power calculation in short eyes. J Cataract Refract Surg 2023;1:49:7:697-703.
3. Kozhaya K, Chen AJ, Joshi M, Kenny PI, Koch DD, Fram N, Weikert MP, Wang L, Khandelwal SS. Comparison of keratoconus specific to standard IOL formulas in patients with keratoconus undergoing cataract surgery. J Refract Surg 2023;39:4:242-248.