Autoimmune diseases and other systemic conditions, such as rheumatoid arthritis and ocular herpes simplex virus are considered relative contraindications for laser vision correction, according to the U.S. Food and Drug Administration, as well as the American Academy of Ophthalmology.1,2 This recommendation was based on potential surgical complications and unpredictable healing responses, yet there are limited case reports of LVC on patients with these conditions.
“The lack of large-scale studies on laser vision correction for patients with autoimmune diseases like RA and HSV contributes to the uncertainty,” says Nichelle Warren, MD, an anterior segment surgeon at Georgia Eye Partners in Atlanta. “There are no large sample sizes to draw definitive conclusions, which makes it challenging to form clear guidelines. Most available data come from smaller studies and reviews. Continued research would be beneficial, but currently, that’s probably not a reality due to the risks.”
Surgeons say there needs to be clarification of the risks associated with refractive surgery in patients with these conditions. “Although some case series suggest that such surgeries can be safe, there are many case reports of poor outcomes,” notes David S. Chu, MD, who’s the medical director at Metropolitan Eye Research and Surgery Institute in Palisades Park, New Jersey, and a clinical associate professor of ophthalmology at Rutgers University. “This discrepancy indicates a need for more detailed research to balance risks and benefits more accurately. No one is disputing that the risks in these patients are higher, but we just don’t know how much higher.
“Despite the risks, people with rheumatoid arthritis undergo refractive surgery regularly,” he continues. “As clinicians, the goal is to carefully select patients and weigh the risks and benefits.”
Without standardized guidelines, refractive surgeons have to make decisions on a case-by-case basis. We asked these experts to chime in on the patient presentations that would give them cause for concern, and on whom they’d proceed with laser vision correction. Here’s what they shared.
Rheumatoid Arthritis and Autoimmune Involvement
RA is a systemic autoimmune disease that can affect more than a person’s joints. Its ophthalmic manifestations can include scleritis, peripheral ulcerative keratitis, uveitis, corneal melt and severe dry eyes, says Dr. Chu.
Historically, patients with RA were often excluded from FDA trials for LASIK and other refractive procedures due to concerns about safety, says Brad Feldman, MD, a cornea/cataract/refractive surgeon at Wills Eye Hospital in Philadelphia and a clinical instructor in ophthalmology at the Sidney Kimmel Medical College at Thomas Jefferson University. “Over time, case series have examined the safety of LASIK for these patients, but there was a degree of cherry picking on which patients were included. RA remains a relative contraindication because there are different types of RA patients. Some have RA that isn’t well-controlled with active inflammation, while others may have only joint disease without additional systemic manifestations, such as skin and eyes.”
This caution isn’t limited to RA; other rheumatic diseases such as lupus, scleroderma and inflammatory bowel disease also fall under this spectrum, Dr. Feldman continues. “For these patients, my general rule of thumb is to avoid offering LASIK if the patient has extra-arthritic manifestations or systemic involvement. This is because these patients are at higher risk for ocular complications either immediately postoperatively or down the road. We aim to select patients who present the lowest risk for complications.”
Small case series have reported some of the risks associated with performing LVC on these patients. “Although refractive surgery is possible for patients with rheumatoid arthritis, it likely increases the risk,” Dr. Chu says. “There are case reports of complications such as severe dry eyes, non-healing corneal ulceration and corneal melting etc., in the literature,” Dr. Chu says. “There have been instances where photorefractive keratectomy in patients with rheumatoid arthritis has gone terribly wrong.”
“A particularly alarming complication is necrotizing scleritis, which can lead to perforation,” says Dr. Warren. “Corneal melt also poses a risk of perforation. Given these risks, it’s crucial to be very cautious about performing any laser vision correction on RA patients. They’re already at a higher risk for possible infection if they’re immunosuppressed. Up to 25 percent of RA patients also have secondary Sjögren’s syndrome, which exacerbates their dry eye. If LASIK is performed, it will further worsen their dry eye symptoms.”
Dr. Chu says it’s important to be aware of overlapping conditions in RA patients. “Regarding autoimmune diseases like Sjögren’s syndrome, patients with severe dry eyes—a common manifestation of Sjögren’s—generally do poorly with refractive surgery,” he says. “Sjögren’s patients who show significant loss of tear production or a very inflamed or dry ocular surface are particularly problematic. These patients, especially those with overlapping conditions such as rheumatoid arthritis, should be thoroughly evaluated and avoided if the ocular surface is excessively dry. Some patients with very dry surfaces may not have been diagnosed with Sjögren’s, so they may not be aware that they have it.”
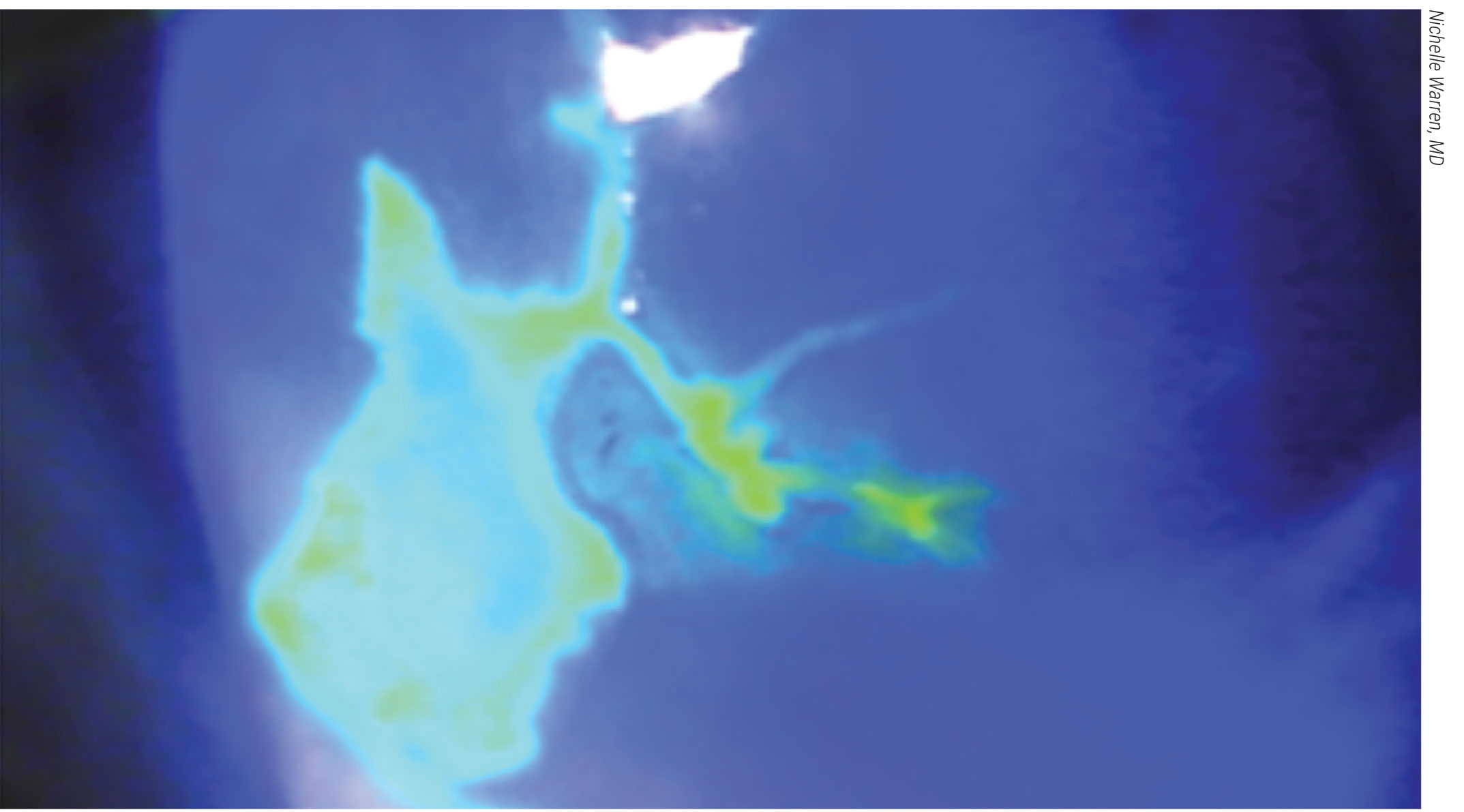
 |
|
This patient with Sjögren’s syndrome underwent PTK for a corneal scar and was then referred to David S. Chu, MD, with a non-healing corneal ulcer, which can be a common complication of those with autoimmune diseases who undergo laser vision correction. |
Despite these warnings, only four retrospective studies on this topic have been published in the past 20 years, according to a paper co-authored by Dr. Chu, in which he summarized those findings.1 The largest and most recent was published in 2016, and it included 1,226 eyes of 622 patients with underlying collagen vascular or autoimmune diseases. Among them, 315 patients had RA. LASIK was performed on a majority of the eyes in the study, with PRK on the remainder, and the authors concluded that no sight-threatening complication such as corneal perforation was reported.3
With this in mind, some surgeons will consider performing LASIK on RA patients under specific guidelines. “If you decide to proceed with laser vision correction for these patients, it’s crucial to first evaluate their tear film using Schirmer’s, staining and tear breakup time,” Dr. Warren advises. “Additionally, a thorough corneal exam should be performed to ensure there are no signs of staining or scarring from previous issues. Ideally, the patient’s disease should be well-controlled for at least six months before considering any surgical interventions. Any uncontrolled disease condition is an absolute contraindication for laser surgery, as it could lead to severe complications.”
Although a Schirmer’s test may be routine on all patients, Dr. Feldman says there are some nuances when RA is involved. “A borderline low Schirmer score is more concerning than it would be for a patient who otherwise has no signs or symptoms of dry-eye disease,” he says. “If a patient with RA has a low Schirmer score but no other findings or symptoms of dryness, I would be more suspicious that this patient may be someone who will have chronic ocular surface disease after surgery. However, if on that same patient, the Schirmer score is borderline but other tests are normal, I might have a more detailed discussion about dry-eye disease with the patient, but I may still offer them laser vision correction, though this is done with greater caution.”
Patients should be asymptomatic for dry eye before proceeding, say surgeons. “There should be no staining on their cornea, and their topography and refraction should be stable,” Dr. Warren says. “Ideally, the patient shouldn’t be on high-dose steroids, and preferably not on any steroids at all. If they’re on immunosuppressants, caution is required because these patients are at increased risk for infection. Additionally, patients need to be fully informed about the potential for future issues, as autoimmune diseases like RA can wax and wane. Even if the disease has been controlled for the past six months, there’s a possibility of problems arising later on.”
Dr. Feldman says he’s hypervigilant in the postop period for these patients. “My approach involves careful monitoring and follow-up,” he says. “I make it a point to examine these patients daily after surgery myself to ensure that any issues are promptly addressed. I wouldn’t co-manage these patients.”
Treating physicians need to be aware of potential complications. “They should monitor for unusual inflammation, such as diffuse lamellar keratitis, or issues with corneal epithelium healing or increased inflammation in the eye, including uveitis or scleritis, which are not typical after laser refractive surgery,” says Dr. Chu. “Any abnormal inflammation should be treated proactively, and consultation with additional specialists might be necessary if issues arise.”
Dr. Warren also says to monitor for any corneal opacifications which could be a scar, the start of a sterile ulceration or potential infection. “It’s also important to look for signs of exacerbation of their dry-eye symptoms, such as increased staining and signs of epithelial basement membrane dystrophy or other complications,” she says, echoing Dr. Chu’s warning about DLK and adding RA patients specifically are at risk of developing peripheral ulcerative keratitis.
“If an epithelial defect is detected, I’m more likely to place a bandage contact lens to promote healing,” says Dr. Feldman, “although I usually have a low threshold for this regardless of the patient’s condition.”
Finally, don’t overlook the role of patient counseling in these situations. “I find that you can help decrease your chair time if you spend the time upfront managing their expectations and educating the patient on the disease and potential problems they might encounter down the road,” Dr. Warren says. “When you educate them ahead of time, it can prevent a patient from blaming their problems on the surgery itself.”
Ocular HSV
Although these surgeons say that LVC on RA patients may be pursued under the right circumstances, they feel differently when it comes to ocular HSV.
“For me, HSV is an absolute contraindication for LASIK or PRK,” says Dr. Feldman. “I won’t perform these surgeries on anyone with a history of ocular HSV. My decision is based on a specific case I inherited where a patient with a remote history of documented HSV went into surgery on valacyclovir and had no early complication. This person developed severe interface haze after surgery, leading to legal blindness and required a corneal transplant. She then had complications in her transplant due to HSV as well. This case highlighted the unacceptable risk associated with performing LASIK in such patients.”
Dr. Chu also says he avoids refractive surgery on patients with HSV due to the risks and complications associated with the disease.
Ocular HSV is a broad diagnosis. “The primary occurrence is often blepharoconjunctivitis,” says Dr. Warren. “However, as cornea specialists, we see more issues related to recurrent infections. These recurrences can lead to stromal opacification, stromal keratitis, epithelial keratitis and endotheliitis, which can cause permanent damage to the cornea and long-term vision loss.”
The main concern with laser vision correction in HSV patients is the risk of reactivating the virus, she continues. “HSV remains dormant in the nerve tissue after the initial infection. If a patient has already had one recurrence, they’re at risk for more. Applying a laser to their cornea could increase this risk. Additionally, the postoperative use of steroids can suppress the immune system in the cornea, increasing the risk of reactivation,” continues Dr. Warren.
Case studies on this topic involving humans are limited, and surgeons have supplemented their research with animal models. PRK has been found to be a particular trigger for reactivation, according to research. In one animal study, de-epithelialization coupled with the excimer laser resulted in a 66.67 percent HSV keratitis reactivation rate.2,4
“For patients with HSV, PRK is particularly risky,” says Dr. Feldman. “The large epithelial defect associated with PRK, combined with the use of steroids, can lead to non-healing defects or geographic ulcers. Even if the patient is on antiviral medication at the time of surgery, the risk of haze and scarring remains high. PRK is generally avoided in HSV patients due to these risks.”
Similar concerns apply to corneal collagen cross-linking, he continues. “I’ve encountered HSV in patients who underwent cross-linking without a known history of HSV,” says Dr. Feldman. “Those things can happen, but in these situations, these patients are prone to haze or scarring in the area of delayed epithelialization. Stromal haze is another risk, and in the worst-case scenario, patients can develop corneal ulceration and melts. Even if they don’t have corneal structural defects, they can have chronic dry eye, which is exacerbated by LASIK or PRK. The procedure itself often leads to dry eye for at least three to six months, which can be particularly problematic for HSV patients.”
Surgeons should take extra care during the patient evaluation. “Most people are seropositive for HSV, but testing isn’t universally recommended unless they demonstrate signs of ocular HSV,” says Dr. Warren. “It’s also important to review the patient’s medication list. For instance, patients may be on acyclovir or Valtrex and that’s a red flag. You want to further tease out why they’re on that medication.
 |
|
In those with ocular HSV, laser vision correction surgeries, including PRK, combined with the use of steroids, can lead to non-healing defects or geographic ulcers, as seen here. Surgeons say the risk of haze and scarring remains high even if the patient is on antivirals, and laser vision correction is generally avoided in these patients. |
“One thing that’s not normally done in other patients but should be done in HSV patients is checking corneal sensitivity,” she continues. “If a patient has had an HSV episode or has latent infection, they could have neurotrophic keratitis. If they’re already neurotrophic, performing LASIK could exacerbate the problem, as cutting the flap transects nerves and can further reduce corneal sensation. This can impair healing even if PRK is performed. Ensuring that the corneal epithelium is healthy and the tear film is in good condition is vital.”
Most surgeons avoid these procedures due to the high risk of reactivation, however, if the patient’s HSV is well-controlled and there have been no recent flare-ups, others may consider proceeding with caution, says Dr. Warren. A narrative review2 that examined corneal refractive surgery in patients with a history of herpes simplex keratitis concluded that surgery is appropriate provided the patient has no history of multiple recurrences and no evidence of disease for at least one year. It also recommended patients begin 400 mg twice daily of oral acyclovir or valacyclovir 500 mg once daily for two weeks prior to surgery, to be continued for two weeks postop or for as long as the patient is on topical steroids.
“It’s important to educate patients thoroughly about the potential risks and ensure they understand the possibility of future reactivations,” says Dr. Warren.
“For those who can’t proceed with surgery, I discuss alternative options such as contact lenses or glasses,” notes Dr. Feldman. “If someone has dry eye and HSV in an eye, they can do well with a scleral lens. Although these alternatives may not offer a permanent solution like LASIK, they can still meet patients’ needs. Patients are often appreciative of the detailed explanation of the potential risks and the focus on their safety. There’s very little pushback when I tell them they aren’t candidates for laser vision correction.”
Dr. Chu, Dr. Feldman and Dr. Warren report no related financial disclosures.
1. Chen TY, Chu DS. Refractive surgery for the patient with autoimmune diseases. Curr Opin Ophthalmol 2020;31:4:247-252.
2. Moshirfar M, Milner DC, Baker PA, McCabe SE, Ronquillo YC, Hoopes PC. Corneal refractive surgery in patients with a history of herpes simplex keratitis: A narrative review. Clin Ophthalmol 2020;16:14:3891-3901.
3. Schallhorn JM, Schallhorn SC, Hettinger KA, Venter JA, Pelouskova M, Teenan D, Hannan SJ. Outcomes and complications of excimer laser surgery in patients with collagen vascular and other immune-mediated inflammatory diseases. Journal of Cataract & Refractive Surgery 2016;1:42:12:1742-52.
4. Asbell PA. Valacyclovir for the prevention of recurrent herpes simplex virus eye disease after excimer laser photokeratectomy. Trans Am Ophthalmol Soc 2000;98:285-303.



