In the quest to find better ways to diagnose and monitor glaucoma, visual evoked potential technology has been a promising avenue of exploration. Monitoring the brain's electrical response to a stimulus using electrodes placed on the scalp bypasses some of the problems that accompany other tests such standard automated perimetry; most notably, the subject doesn't need to respond to stimuli by pushing a button.
The best-known version of this technology is multifocal VEP, which is similar in design to standard automated perimetry in that it maps the visual field. The chief problem with mfVEP has been that it's a time-consuming test; it can take even longer than a standard automated perimetry test, making it potentially difficult for some elderly patients, while taking up valuable clinic time. Primarily for that reason, its theoretical advantages over SAP haven't been sufficient to make it a popular technology outside of research situations.
However, VEP technology may be more practical when employed in other formats. Researchers at three sites in the
icVEP vs. mfVEP
George Hu, PhD, founder of VeriSci, the company currently developing the icVEP technology, has been working with this technology for almost two decades; he collaborated with Vance Zemon, PhD, professor at the Ferkauf Graduate School of the Albert Einstein
"Both VEP technologies place a stimulus in front of the patient and record the visual evoked potential," explains Dr. Hu. "The major difference between mfVEP and icVEP is that with mfVEP, you're displaying multiple stimuli at different points throughout the visual field while asking the patient to focus on the center of the screen, just as SAP technology does. If the patient has some visual field loss in one area, the lowered VEP response in that part of the field will reveal it, producing a map of the visual field much like that produced by a visual field test. And, like SAP, mfVEP essentially looks for visual field loss in the peripheral area.
"Isolated-check VEP uses a different ap-proach," he continues. "We display a single stimulus pattern on the entire screen at once. As a result, the technology doesn't produce a visual field map showing the viability of individual areas in the visual field. In fact, we're basically testing the viability of the patient's central vision rather than the details of the patient's peripheral vision."
Dr. Hu notes that clinical evidence supports the idea that central vision is affected by early stages of glaucoma—even though the periphery is the area that's traditionally been measured. "The vision-related cells in the central retina have a much higher density, making early damage to a few cells more difficult to measure," he points out. "However, icVEP technology can detect subtle losses in central vision because it taps select neural pathways in the visual system.
"We use a high-temporal-frequency, low-contrast stimulus that targets the magnocellular pathway," he continues. "That pathway seems to be particularly good at revealing early glaucoma damage; the signal-to-noise ratio tells us whether a patient has a central visual defect." (In the Phase I trials, 100 percent of controls passed the test, while nearly all glaucoma patients did not.)
Dr. Hu adds that VEP technology isn't new; it's been available for about 50 years. "Mostly, it's been used in the laboratory, not in the clinic," he says. "The problem has been that the VEP signal is very weak and it's embedded in the larger noise of brain activities. It's hard to extract. So we've designed a special stimulus and algorithms that strengthen the signal and reduce the background noise, which help us get a reliable response. Our innovation is not VEP; our innovation is making it practical and reliable for use in a clinical setting."
Taking the Test
Dr. Hu explains that when a patient takes the test, the stimulus is displayed for two seconds. "The two-second stimulus runs eight times in a row with a break of about two seconds between test runs," he says. "Artifact rejection software alerts the operator if any of the eight tests are statistical outliers, so the test can be repeated until eight valid results have been obtained for processing. The whole test takes about 30 seconds per eye, plus the time it takes to put three electrodes on the patient's head, which is usually less than five minutes."
"The patient doesn't really experience anything, except possibly a little fatigue from trying to concentrate for a few seconds," notes James C. Tsai, MD, chairman of the Department of Ophthalmology and Visual Science at Yale University School of Medicine, and chief of ophthalmology at the Yale-New Haven Hospital in New Haven, Conn. (Dr. Tsai has been the principal investigator in both Phase I and Phase II clinical trials of the icVEP instrument, funded by two National Eye Institute Small Business Innovation grants.) "There's no sensation, and there are very few risks associated with the test. The worst part of the whole test is that you have to wash your hair afterwards."
Dr. Hu describes several advantages of icVEP. "One advantage of using a single stimulus to test central vision is that fixation is much easier," he says. "Even if there's a little eye movement, the results are not affected.
"A second advantage," he continues, "is that the test is much faster than either mfVEP or a visual field test because we're presenting a single stimulus, not a series of stimuli in different locations across the visual field. A third advantage is that the visual evoked potential signal we're measuring is much stronger and more reliable because we use the whole screen for the stimulus."
Dr. Tsai notes another downside to visual fields: You generally need several tests to be sure of the results. "The Ocular Hypertension Treatment Study found that 88 percent of the time, visual fields that initially showed a defect found a normal visual field when the test was repeated," he points out. "We've seen that in our SAP pa-tients as well; they get worse in one test and then do a little better the next time. It may be that ganglion cells deteriorate gradually, and depending on the time of day and the stress the cells are under, they transmit more or less information. We're curious to see whether measuring contrast sensitivity via M-cell activity will give us more consistent test results."
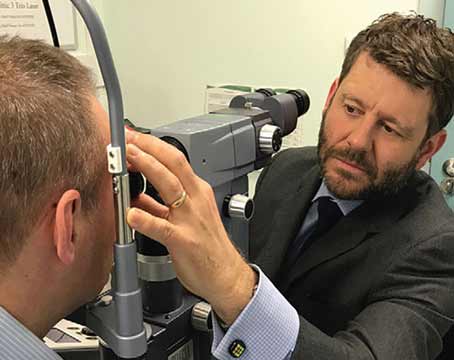
Dr. Hu says the instrument design has evolved since the Phase I trials. "We've increased the speed of the stimulus display frame rate, and increased the grey-level resolution from eight to 16 bits so the screen can display a more precise stimulus," he notes. "We've also improved the data processing and added a chinrest so the patient stays the correct distance from the screen. Furthermore, we've mounted a camera so the operator can monitor patient fixation during the test. (See picture, above.) If the operator sees that the patient is falling asleep or unable to focus, the test can be run again."
Dr. Hu admits that some patients have non-glaucomatous problems in their central visual pathways that could interfere with taking the test, but points out that discovering that is part of the doctor's job. "If the patient has other problems such as macular degeneration that might interfere with central vision, the doctor needs to identify them," he says. "If no other problems are present, a questionable icVEP result will give the doctor a good reason to suspect the presence of glaucoma."
Dr. Tsai agrees. "In order to determine contrast sensitivity, the patient must have high-level visual acuity," he says. "However, I don't think the need for good central vision will be a serious problem. Most early glaucoma patients have field loss in the periphery; they don't usually notice anything centrally. A certain percentage of patients may be excluded because of this requirement, but the majority, especially patients who just want to know if they have any early evidence of glaucoma, will still have good central vision."
A Promising Adjunct
"Some ophthalmologists are a little skeptical about this technology, but I think they misunderstand what we're trying to do," says Dr. Tsai. "This is not intended to replace visual field testing; it's meant to be a complement to it. We're interested in seeing whether this technology can provide another data point to help determine whether glaucoma is present, whether a therapy is slowing progression, and whether a non-IOP-lowering treatment is having an effect on vision. As you know, a patient can lose 30 or 40 percent of his ganglion cells before he has a visual field abnormality. We're hoping that icVEP will be able to provide earlier evidence that a person has developed glaucoma so treatment can begin before the loss becomes that extensive.
"This technology could also impact glaucoma clinical trials," he continues. "Most clinical studies of glaucoma that go beyond simply trying to lower IOP take several years to show a clear-cut difference between groups because they depend on visual field results. If this technology can pick up a change more quickly, it could make clinical trials faster and easier to perform. In addition, it might serve as an alternative when a patient has difficulty taking the visual field test—someone who pushes the button all the time, or always looks toward the test signal instead of maintaining focus on the target."
"Conservatively, we think of this instrument as an aid for glaucoma diagnosis, not a replacement for the other instruments," agrees Dr. Hu. "It's a way for the doctor to get another perspective on the patient's status. Visual field tests examine specific areas of vision loss; icVEP tests the overall strength of the evoked signal.
"In theory, this technology should be able to detect glaucoma earlier than a visual field test can," he adds. "If a patient has a visual field loss, it means he's partially blind already. He can't see in one area of the viewing field. Our technology is different because the patient may still be able to see despite early damage, but we can detect the damage because the evoked potential signal is weaker."
Dr. Hu also points out that the technology should be useful for monitoring progression, even though the current clinical trials are focused on detecting early glaucoma. "As the disease progresses, the VEP signal should become weaker and weaker," he notes.
Dr. Tsai agrees. "In the future, we hope to conduct longitudinal studies to see whether the technology picks up changes in signal-to-noise ratios or other values as the glaucoma progresses, and how those changes compare with conventional visual field tests," he says.
What's Next
"In the first trials, we tested all the patients with both icVEP and visual fields," says Dr. Hu. "In Phase II, we're also testing with OCT and FDT. It's too early to know what correlations we may find. In addition, we're retesting subjects to evaluate repeatability.
"We hope to finish all the data collection in March or April of this year;," he adds. "Then we'll need a few months to evaluate all of the data." (The three sites involved in Phase II testing are
"In Phase II, we're trying to ratchet up the sensitivity," adds Dr. Tsai. "We're trying to determine whether icVEP can clearly differentiate between mild glaucoma, no glaucoma, ocular hypertension and a glaucoma suspect. For the technology to be practical and clinically relevant, the sensitivity has to be more robust."
Dr. Hu is also concerned about commercializing the technology. "I hope that after we analyze the Phase II data we'll be able to start working on getting this technology to the marketplace," he says. "We want to make sure that the marketing of the device complies with FDA regulations, and we also need to resolve other issues such as insurance reimbursement. Insurance codes already exist for VEP testing to assess visual neural defects, but we have to make sure icVEP will be covered when used for glaucoma assessment in a clinical setting. Hopefully the current clinical trials will demonstrate that this is a valid tool for diagnosis of glaucoma."
In terms of when an icVEP instrument might be available to the average clinician, Dr. Tsai believes it will take at least five years for this technology to reach the marketplace. "My estimate may be conservative, but ac-cumulating sufficient data to prove the effectiveness of the technology is laborious and takes time," he notes. "Hopefully we'll see results from the Phase II trials before the end of the year. In the meantime, the company is working to refine the instrument to make it as easy as possible to incorporate into clinical practice."
Dr. Tsai adds that he has confidence in the science behind icVEP. "Dr. Hu and his team have studied this for years," he points out. "It's exciting to work on because there's clearly something here that has enormous potential."