Presentation
A 53-year-old female presented to Wills Eye Hospital for evaluation of double vision she’d had for three months. Five months prior, she presented to her primary care physician with chronic headaches, sinus pressure and right-sided periorbital swelling. She was treated with amoxicillin/clavulanic acid and low-dose oral prednisone for presumed sinusitis, and brief improvement in her symptoms was noted. She returned for evaluation two months later with recurrence of sinus pain and headaches, as well as epistaxis and binocular diplopia, most prominent with lateral gaze. An enlarged, mobile cervical lymph node was also discovered on exam, and she was referred to an otolaryngologist for further evaluation. Transnasal endoscopic biopsy of her sinuses was performed and showed inflammatory changes consistent with chronic sinusitis, without any evidence of malignancy. She was subsequently directed to the Otolaryngology and Ophthalmology departments at Thomas Jefferson University Hospital and Wills Eye Hospital for further evaluation.
Medical History
Her past medical history included hypertension, hyperlipidemia and obstructive sleep apnea. In addition, her history was notable for several years of chronic sinusitis, for which she had undergone previous endoscopic sinus surgery with minimal relief. Her family and social histories were noncontributory. Current medications included montelukast, desloratadine, pravastatin and candesartan/hydrochlorothiazide.
Examination
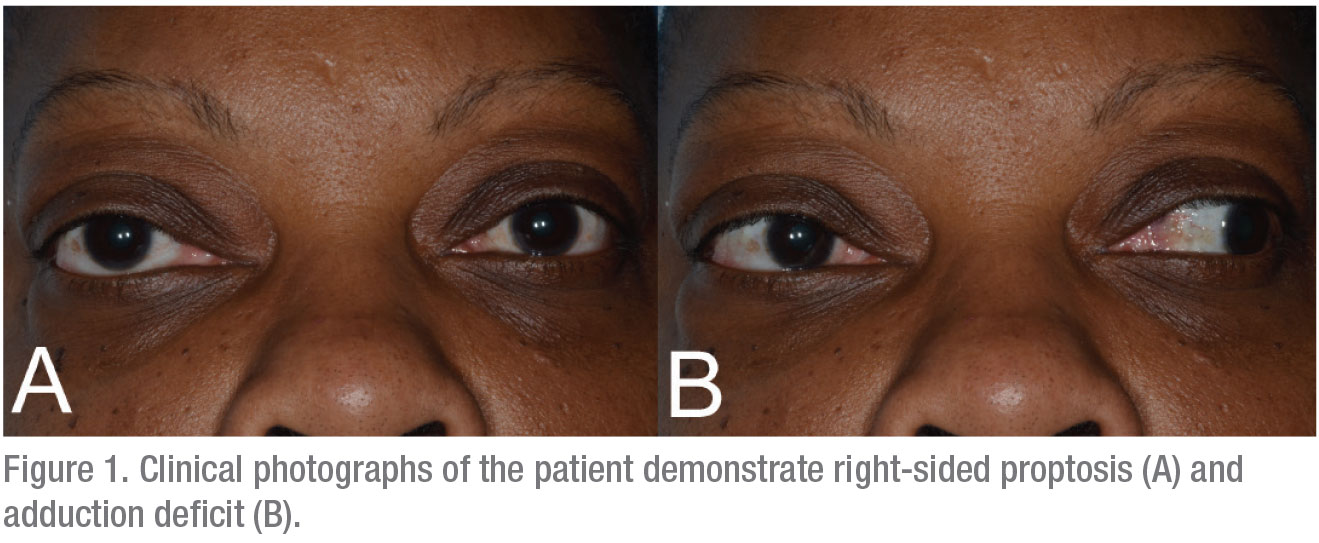
Ophthalmologic examination revealed a best corrected visual acuity of 20/25 OD and 20/20 OS. Her pupils were equal, round and reactive to light with no afferent pupillary defect. Intraocular pressures were 25 mmHg OU. The patient’s external exam was remarkable for mild lateral displacement of the right globe and 1 mm of proptosis of the right eye by Hertel exophthalmometry. Extraocular movements demonstrated orthophoria in primary gaze but bilateral restriction of adduction, right greater than left. Mild restriction of infraduction was also noted OU (Figure 1). Her visual fields were full to confrontation and color plates were full OU. Her slit lamp exam was within normal limits except for 2+ nuclear sclerotic cataracts OU.
 |
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.



