Preop Issues
Experts say that, when looking for potential problems, their evaluation runs the gamut from a patient’s cornea and retina to his personality.
• Age. Surgeons say something as basic as a person’s age can affect the outcome of a multifocal. “One of the aspects is just age in general,” says Des Moines, Iowa, ophthalmologist James Davison. “We don’t have a hard-and-fast age limit, but if someone frail comes in wanting the best vision but isn’t in shape to appreciate the function of the multifocal intraocular lens, we kind of discourage it in him. With these IOLs, there is some loss of contrast sensitivity, and you need a certain mental facility to enjoy the kind of vision multifocals give you. Some people just don’t have that mental facility anymore.”
• Ocular surface. Since the tear film is the first thing incoming light hits on its way to the retina, surgeons say it better be in good shape if you want something as complex as a multifocal optical system to work properly. “Look at it this way,” says George Beiko, MD, of Toronto, “if you have a television with a great picture tube but a dirty screen, you’re not going to get a good image. You have to get everything working properly.
“Dry eye will impact all lenses,” Dr. Beiko continues. “Even a monofocal IOL will be impacted. You can have a perfect surgery but the vision will still not be good because of dry eye or lid issues. Recently, I had a monofocal IOL patient whose vision wasn’t good because of chronic blepharitis associated with acne rosacea. Last month I put him on some doxycycline, and when I saw him this month he said he noticed improvement. It will take three months for him to get the full effect. In a multifocal patient, fairly bad blepharitis would be a red flag, and is a common problem in the elderly, whether it’s seborrheic blepharitis or blepharitis associated with acne rosacea or Demodex mites. These conditions tend to lead to corneal surface disease and need to be treated fairly aggressively. For blepharitis, my first-line treatment is lid hygiene, from which I’ll progress to ointments such as a combination steroid/antibiotic or a mild antibiotic like erythromycin on the lid margin. If that approach doesn’t treat it effectively, or if someone has fairly severe acne rosacea, I’ll go to an oral medication such as doxycycline.”
Beverly Hills, Calif., surgeon Kerry Assil says that, even though dry eye is something that needs to be addressed, you’ll know early on whether the person is a candidate for a multifocal or not. “Certainly, dry eye should be addressed in advance,” he says. “However, if someone in the cataract age group has dry-eye disease, it will usually either be mild, which you can treat, or severe. So it isn’t often a dilemma: If the dry eye is severe they wouldn’t be a good candidate for a multifocal IOL.”
Dr. Davison, who describes himself as conservative when it comes to selecting candidates for multifocal IOLs, says also to be wary of patients with lower-lid ptosis or retraction that’s causing ocular surface problems.
• Corneal health and shape. Some corneal irregularities can be dealt with ahead of time, but some are deal breakers, doctors say.
|
Dr. Assil also watches out for corneas with unusual measurements. “Neither the ReSTOR nor the Tecnis performs brilliantly in patients with steep central corneas,” he says. “This is especially true if they’ve had a significant amount of hyperopic LASIK previously, whereby the central cornea steepening (relative to the mid-peripheral cornea) is accentuated. Elevation maps and topographic maps will usually alert the surgeon, though a good rule of thumb is that anyone who’s had more than 1 to 1.5 D of previous hyperopic LASIK might be a suboptimal candidate for a multifocal IOL. By the same token, a patient who’s had more than 3 or 4 D of myopic LASIK could be problematic, because very few of those treatments are so perfectly centered as to enable synergistic optics with a multifocal lens. Also, in post-RK eyes, we have to select patients sparingly for premium IOLs.”
When it comes to corneal evaluation, surgeons note that you have to consider ahead of time how you’re going to handle pre-existing astigmatism, and rule out patients with irregular cylinder. “Irregular astigmatism is a red flag,” says Alexandria, La., surgeon R. Bruce Wallace. “However, patients with regular astigmatism of 0.75 D and lower could have a multifocal lens, though it depends on where the incision is and where the astigmatism is. If it’s against-the-rule, then you’re reducing some of that with a phaco incision. It’s just the opposite in cases of with-the-rule astigmatism, where it will depend on where the astigmatism is located and how accurate your measurement is. For low levels like that, the topography may not even match the K readings that well.”
Dr. Davison feels similarly, saying that you can’t reliably deal with 0.5 D of astigmatism. “If someone has 0.75 D of astigmatism, I’ll correct it with the femtosecond laser using 80 percent of the arc length suggested by the Donnenfeld nomogram, at 80 percent depth. For with-the-rule astigmatism I open the incisions because they’re usually smaller and above and below the cataract incision. For against-the-rule, they’re usually larger incisions because they’re paired with my cataract incision, and I won’t open them because they’re going to have a larger effect to begin with. I don’t correct for 0.5 D because that’s within the standard deviation of our measurement devices, so it’s not something I can reliably measure and correct. However, multifocal patients with 0.5 D of astigmatism are usually happy, but it’s still the great unknown. You don’t know who is going to be happy and who’s not. To gauge if someone will be happy, you’ve got to look at astigmatism in relation to all the other factors, such as their aberrations, the front and back surfaces of their cornea, their macula, the lens centration and their mental status.”
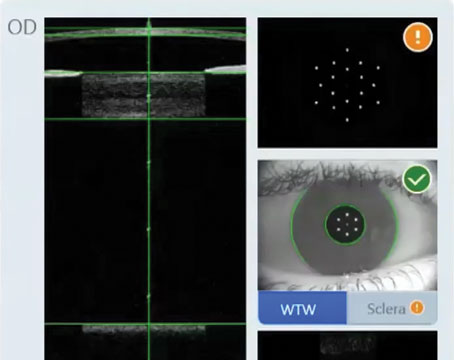
Dr. Assil says that, if he is going to correct the astigmatism intraoperatively, the WaveTec VerifEye has become invaluable to him. “If the surgeon is trained on the proper use of the device, then the astigmatism may consistently be titrated down to the amount deemed appropriate,” he says.
Dr. Beiko looks for nice, sharp mires on keratometry. “If they’re sharp, it’s likely the surface is good and there isn’t anything negative going on,” he says. “But if there are distorted mires, you have to use topography to take a good look to see if it’s pellucid marginal degeneration or keratoconus. There are some elderly patients who have some degree of keratoconus that may not have been diagnosed. They may also have peripheral marginal disease, either guttering or thinning, that can also affect the quality of the light going through the cornea. If you see marginal disease or pellucid, it will be hard for the patient to be happy with the vision because it will distort the light coming through the cornea. I’ll have a discussion with him about that, informing him that he’s not the ideal candidate even though he might get some benefit from the multifocal lens. Sometimes, having had that discussion, the patient will want to go ahead with it and see what result he can get.”
Also be aware of any contact-lens-induced corneal warpage that can give false readings or mask other corneal problems. “Typically, we recommend patients stay out of soft contact lenses for a few weeks,” says Dr. Beiko. “If they’re in hard contacts, then stay out of them for a month or two. We perform an initial topography, then see them in a month to see if there’s been any change. If there is a change, then we see them a month later, ultimately waiting until it’s all stable.”
• Specular microscopy. Gauging the overall health of the cornea can actually help pick out borderline cases. “If you perform specular microscopy and find that the patient has a low cell count relative to an age-matched group, or if the cells are irregularly shaped, that may indicate he’s at risk for a corneal procedure later on, such as DSAEK or PK,” advises Dr. Beiko. “You have to warn the patient that, if this occurs, the quality of vision will drop with a multifocal much more than it would with a monofocal IOL.”
• Higher-order aberrations. Researchers and clinicians are beginning to get a sense that there are certain levels of higher-order aberrations that make it more challenging for a multifocal patient to tolerate his new lens. “Warren Hill, MD, has pointed out that corneal coma—positive or negative, vertical or horizontal—is indicative of increased visual symptoms and multifocal intolerance when it reaches a value of 0.32 µm or greater,” says Dr. Beiko.1 “Also, at the 2012 meeting of the American Society of Cataract and Refractive Surgery, Marc Michelson, MD, from Birmingham, Ala., presented a paper in which he found that patients with 0.12 µm of horizontal quatrefoil had trouble tolerating multifocality, while those with up to 0.07 µm could tolerate it. He also found that, in his patients who were unhappy with their multifocal lenses, the total RMS value of the third- and fourth-order aberrations was 0.23 or greater. Patients with third- and fourth-order aberrations totaling 0.18 µm or less were tolerant of multifocality. So, in patients who fall into these intolerant ranges, he basically won’t implant multifocal lenses because they’ve got corneal issues that are generating these higher-order aberrations and making the vision poor.”
• Retinal issues. A retinal issue that can arise in many patients is the presence of an epimacular membrane, and it may take work to suss out.
|
Though some surgeons are moving toward performing optical coherence tomography on all their prospective multifocal patients, Dr. Beiko says you can begin with a good posterior exam with either a 60- or 90-D lens and, if you have any suspicions, move on to an OCT. “Typically, when someone has an epimacular membrane and you take it out, the vision won’t be perfect. I think this type of case would be on the borderline, and most surgeons would shy away from implanting a multifocal.”
A substantial amount of macular degeneration would be a contraindication, but some surgeons say there are exceptions. “If it’s a tiny amount of drusen, I think it would be OK,” says Dr. Davison. “The same goes for a small amount of RPE pigment changes in an older person. But, if someone is 55 years old and he’s starting to show those signs, I’m not sure that’s the type of person I want to put a multifocal in, because if he lives to be 80 then sooner or later he’ll likely suffer some macular dysfunction.”
• Anticipate halo/glare problems. Surgeons note that some patients are more sensitive to qualitative problems than others. “What I say to cataract patients is that any IOL we put in their eyes, even a monofocal lens, has a risk of glare and halo, but that multifocal IOLs have a slightly higher risk,” says Dr. Beiko. “I also inform them that it takes about six months to adapt to that change. So, the contract has to be in place that states if the patient is going to have a multifocal he’s aware of this risk and will give it at least six months before giving up.”
Intraoperative Factors
Small parts of the surgery itself can prove to make a big difference if they’re not executed well, say surgeons.
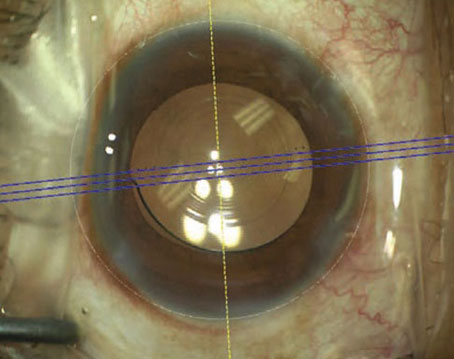
• Centration. Dr. Wallace says there are aspects of the lenses themselves that can help you avoid a decentration that can decrease results. “What’s nice about these multifocal IOLs compared to monofocals is that you can tell how well they’re centered using their rings,” he says. “I like to be 0.5 mm nasal rather than in the middle of the pupil, because I think that’s where the sweet spot is for the quality of vision.” This sentiment demonstrates what Dr. Davison believes: “I think you center these lenses where they look good to you, which is maybe the center of the pupil, the limbus or maybe both,” he says. “I’m not sure I believe everything I hear about factoring in angle kappa when centering these lenses. Some surgeons say at the end of surgery you should nudge the lens over and it will be perfect, but I don’t believe in nudging it. These lenses go where they want to go, though I think you can influence their position by rotating them to an optimal location within the capsular bag so they appear to be centered better to you. Empirically for me, that position turns out to involve orienting the haptics supero-temporal to infero-nasal. I don’t have any study that shows this orientation is superior, but that usually gives me the best result.”
• Avoid leaks. Surgeons say that you could pick the best patient and the ideal lens but still falter at the finish line. “Make sure the entry site is well-sealed at the close of surgery,” says Dr. Assil. “This isn’t just for the obvious reasons of avoiding inflammation and infection, but also to avoid a shift in the IOL’s position due to IOP decrease from the wound leak. This is even more important with toric IOLs.”
Dr. Davison says that, if you pay attention to the small factors as well as the large, and select patients carefully, working with multifocal lenses can be rewarding. “There’s no one more happy than someone with a multifocal lens who sees well—it’s wonderful to see,” he says. “However, there’s no one more unhappy than someone who has expectations of multifocality and good functional vision but doesn’t get it—then it’s a disappointing and regrettable experience for everyone.” REVIEW
1. Warren Hill, personal communication