|
These are some of the results from this month’s survey on intraocular lenses. This month, 23 surgeons (4.6 percent) of our 500-physician panel responded. See how your preferred practices compare with theirs.
Presbyopic Opinions
Fifty-six percent of respondents implant multifocal, diffractive or accommodating IOLs. In terms of presbyopic lens performance, 64 percent say they are satisfied, 14 percent are very satisfied, 7 percent are somewhat satisfied and 14 percent are unsatisfied. On the survey, 43 percent of surgeons implant the ReSTOR +3 D lens the most in their practices, 43 percent prefer the Tecnis multifocal and 14 percent use the Crystalens AO. Tecnis users implant an average of 10 per month with a charge of $2,479; ReSTOR users implant an average of six lenses per month with an average charge of $1,913; and Crystalens users report implanting an average of nine lenses per month, though they didn’t share their average charge for them on the survey.
Robert Epstein, MD, of McHenry, Ill., often implants the ReSTOR. “I am satisfied—but not ‘very’ satisfied—with the ReSTOR,” he says. “There are definitely patients with it who have awesome-looking eyes with no astigmatism but unsatisfactory vision. If there is any macular or dry-eye issue in the patient, then forget it; the multifocal lens results will be inadequate and you will wish you never agreed to put it in. The Lord did not necessarily align the center of the capsular bag with the center of the pupil, so surgeons should make sure that the two are aligned at the end of surgery for best results, but it may shift slightly or just not align that way. Definitely underpromise [to the patient].”
A surgeon from Florida says that though she is somewhat satisfied with the multifocal IOL that she uses, there is still room for improvement. “Multifocality is not the best solution for presbyopia,” she says. Richard Erdey, MD, of Columbus, Ohio, says he’s very satisfied with the Crystalens, but would like to see some tweaks: “The Crystalens is not a one-size-fits-all IOL,” he says. “We perform UBM on all candidates and screen out those with short capsular bag diameters to avoid Z or U syndrome. B + L should offer a 0.5-mm smaller diameter option throughout the available power range.”
|
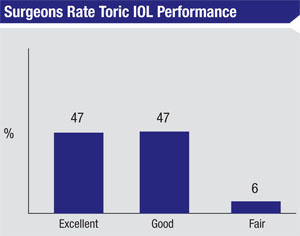
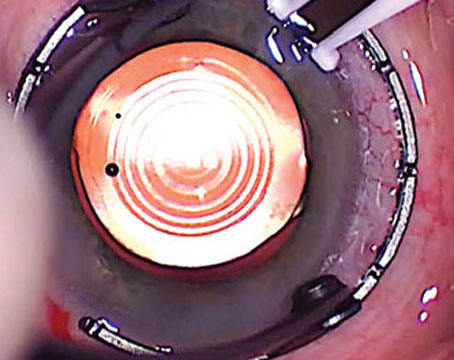
Panelists continue to be impressed with the performance of toric IOLs, with 68 percent of the surgeons saying they implant them. Forty-seven percent rate toric IOL outcomes as excellent and another 47 percent say they’re good. Only 6 percent say toric outcomes are only fair.
Miami ophthalmologist William Trattler says his toric outcomes have been “excellent,” and Fort Myers, Fla., surgeon Mark Gorovoy says he thinks toric performance has been good, though he notes, “It’s rare to hit ‘zero’ cylinder.” Gerald Roper, MD, who rates toric performance as fair, says that in his experience, “Patient satisfaction is fair, and comparable to monofocal [lenses], but they are still spectacle-dependent at a high cost.” Another surgeon from Florida says her experience with torics has been excellent, but adds, “I wish they didn’t have glistenings.”
IOL Materials and Features
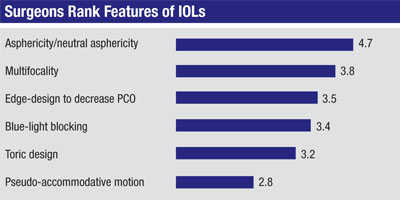
Surgeons also weighed in on what they like about the lenses they use most, and the features, such as multifocality, asphericity or the presence of a toric correction, that they find most useful.
In terms of the lens they use most often, 43 percent of respondents say it’s the Alcon SN60WF, 17 percent choose the Tecnis, 13 percent name the Bausch + Lomb SofPort AO, 8 percent prefer the Lenstec Softec HD, and the Rayner C-flex and Hoya iSymm/iSert each were chosen by 4 percent of panelists. Eight percent of the respondents chose “other.”
|
“Acrylic folds easily and has good biocompatibility,” says a surgeon from New York. A surgeon from New Jersey says, “The Alcon SN60WF is easy to use and a great option ... acrylic is biocompatible with silicone oil if it’s ever needed for retinal work.” A Tecnis fan from Maryland appreciates the lens for its “great centration, great optics, and the fact it’s a single-piece lens,” while a surgeon from Florida prefers the B + L SofPort AO for the same reasons: optics and centration. Dr. Trattler likes both the Tecnis and the Softec HD, saying, “Both IOLs provide excellent quality of vision, a very low incidence of negative dysphotopsia and, in general, no glistenings.”
None of the surgeons report implanting the Implantable Miniature Telescope IOL (VisionCare, Saratoga, Calif.). “I very much like the idea,” says Dr. Epstein. “I have brought up the idea to several patients and they were somewhat cool to it, though. I know the inventor, Isaac Lipschitz, MD, and he told me about a newer lens that only enlarges a part of the field of vision, rather than the entire field. I like that idea better.”
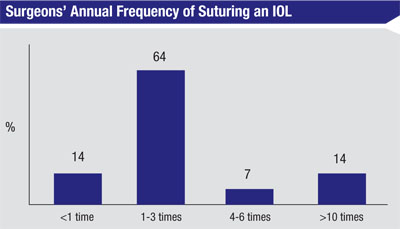
Lens Complications
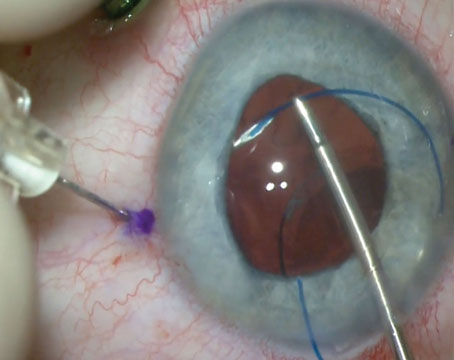
Though surgeons like their lenses for the most part, problems can and do occur from time to time. Fifty-three percent of our panelists say they have to re-enter the eye and suture one to three lenses per year, 12 percent have to suture refixate four to six lenses, and 6 percent have to suture more than 10 lenses. Twenty-nine percent, however, say they don’t suture any lenses during the year (either because of no complications or because they just refer them to another surgeon for performance of the procedure).
Reasons for suturing include: loss of zonulocapsular integrity from trauma or pseudoexfoliation; dislocated lens/capsular complex; and planned scleral fixation in patients with significant zonular laxity. Dr. Epstein explains his suturing approach: “In these cases, I use intraocular forceps and do an intrascleral haptic burial technique that doesn’t require sutures for the fixation,” he says. “I used to perform suturing to the sclera into the sulcus. It’s worthwhile to bury the suture with the knot intracorneally at the limbus, but the best way is with no sutures at all.
The most annoying aspect of fastening the IOL to the sclera is dealing with sutures eroding through or around the scleral pocket and through the conjunctiva. I will sometimes operate on these cases with a vitreoretinal surgeon.”
|
Surgeons also described the most common causes for explanting a lens and replacing it with a new one in the past year. These include:
• incorrect lens power;• an unhappy multifocal IOL patient;• luxation or malposition in general;• haptic in the sulcus; and• not achieving the targeted refraction in a premium lens patient.
Though many physicians and patients are satisfied with their patients’ multifocal lens outcomes, some surgeons say it’s almost inevitable that they will encounter an unhappy multifocal recipient at some point. Says Fort Myers’ Dr. Gorovoy: “I see an unhappy multifocal IOL patient almost every week.” REVIEW