Pharmacokinetics does matter: It is at the heart of strategies seeking to decrease drug side effects and increase efficacy, duration and an agent's ability to reach biochemical targets that were once unreachable. This article, the first in a series of Therapeutic Topics on the different aspects of pharmacokinetics and drug delivery, will address concepts related to the duration of action of drugs. It will also introduce the different ways a drug can extend its efficacy profile.
What Influences Drug Duration
Two parameters affect the duration of action of a particular drug: its general physiological mechanism of action and the dynamics of the tissue concentration of the active ingredient over time. A good example of how the mechanism of action of a drug can influence duration of activity are the prostaglandins Xalatan (latanoprost) and Travatan (travoprost), and the prostamide Lumigan (bimatoprost). Compared with other classes of glaucoma medications, which may have effects on aqueous production or the contraction/expansion of ciliary and dilator muscles, some researchers believe these drugs induce structural changes in the trabecular meshwork, the ciliary muscle and/or uveoscleral outflow.
Research has shown how the intraocular pressure-lowering effect can actually be maintained for a few days or more, even after discontinuation of the drug.1 After examining the bioavailability of the drug in the tissue, it's apparent that tissue concentrations alone probably can't account for the duration; pharmacokinetic studies have shown that the elimination of drug from the eye is fairly rapid. With latanoprost, for example, in humans, the maximum concentration of active drug in the aqueous humor occurs one to two hours following topical administration, and has an elimination half-life of two to three hours.2 Rapid drug hydrolysis, examined in rabbits, was evident throughout many regions of the eye, with elimination half lives in ocular tissues ranging from 1.4 hours in conjunctiva to three hours in aqueous.3 Therefore, the prolonged drug effect is probably due to structural changes to the tissue, which take time to recover, as well as maintenance of the drug presence at receptors.
Allergy drugs with multiple modes of activity are another example. Olapatadine 0.1% (Patanol, Alcon) and ketotifen 0.025% (Zaditor, Novartis Ophthalmics), which have both antihistamine and mast-cell stabilizing properties, have a much longer duration of action, at least 12 hours, than antihistamines such as pheniramine (Naphcon-A, Alcon), levocabastine (Livostin, Santen) and emedastine (Emadine, Alcon), which have durations of two to four hours. The mast-cell stabilizing properties are thought to confer the longer duration of action. While these agents' exact mechanisms of action aren't clear, changes in cell membranes may occur that impede the release of mediators from the mast cell during subsequent exposure to allergens.
The concentration of drug in tissues is affected by several factors. Variables that work against bioavailability include barriers to penetration, drainage, dilution and metabolism. Things that work to increase bioavailability include enhanced penetration to the target tissue, maintaining concentrations of the active ingredient over time and increased dwell time.
The Drug Delivery Problem
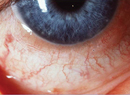
The eye's defense mechanisms make it difficult to achieve the necessary concentrations of drugs. Systemic drugs face the challenge of passing through the blood-aqueous and blood-retinal barriers. Drugs administered topically must pass through the cornea and conjunctiva and are subject to rapid elimination from the precorneal area through drainage and tear-fluid turnover. Less than 5 percent of an instilled topical drug reaches the intraocular tissue.4
When a drug is administered to the eye, the solution first mixes with the lacrimal fluid. The lacrimal fluid drains into the nasolacrimal duct during blinking, resulting in the elimination of a large portion of the drug.
This drainage is particularly evident in allergy, as allergens that enter the body at the ocular surface have been shown to induce allergic symptoms in the nose as well. Conversely, when allergens enter through the nose, no ocular reaction is evident, confirming the unilateral downward flow of drainage from eye to nose. The same is observed with use of topical ocular antiallergy medications; instillation of a drug onto the ocular surface can have a significant effect on management of nasal symptoms as the active agent drains through the nasolacrimal ducts.5-7
You can see additional evidence of how significant this drainage can be with the systemic effects of beta-blockers. The medication can penetrate the corneal epithelium through either the transcellular (for lipophilic drugs) or the paracellular (for hydrophilic drugs) pathways. The effect of a topical drug is further slowed due to its binding to corneal tissues and gradual release into the aqueous humor. Once the drug reaches the aqueous humor, it's diluted further and is then slowly distributed to the intraocular tissues.
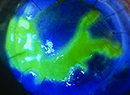
The major factor limiting ocular absorption of eyedrops is the cornea. The epithelium is lipophilic and functions as a barrier to ion transport. Tight junctions in the epithelium prevent the diffusion of macromolecules and act as a selective barrier for small molecules. The stroma is a highly hydrophilic layer and the endothelium functions to maintain corneal hydration.
Factors that affect the permeability of drugs in the cornea are lipophilicity, hydrophilicity, ionization, charge, solubility and molecular shape and size. Further, enzymes such as esterases are present in the cornea, and they act to metabolize drugs before they can even penetrate the eye.
Enhancing Bioavailability
It's certainly desirable to increase the duration of action of drugs, as there are clear implications for compliance. So what types of strategies are being pursued? The use of pro-drugs (e.g., dipivefrin [Propine, Alcon], latanoprost and travoprost) to counter metabolism is widely known. Clearance of the drug can also be reduced by addressing the dilution that occurs in the tear film. With this, you can see how the comfort of a drop is very important. Efforts to increase the comfort of a drop may focus on changes to its pH, osmolarity, or use of a new vehicle. If instillation causes stinging, burning and subsequent tearing, this can dilute the amount of active drug available. Nasolacrimal occlusion can help keep a drug from draining as quickly, allowing it to remain longer on the ocular surface.
Recent developments in drug delivery systems have focused on maximizing ocular drug absorption by keeping the drug in the cornea longer and by slowing the release of drug from the delivery device. Classes of ocular drug delivery systems include polymeric gels, colloidal systems, cyclodextrins, collagen shields and systems that bind to receptors on the surface of the eye. Next month, we'll talk more about these technologies, as well as devices that can increase penetration into the eye and release a drug over time.
When tissue levels of a substance reach a maximum level, the half life will remain consistent. This means that when a product with X0% is instilled, and X1% is left after 16 hours, then if the drug at a concentration of 2X0% is instilled, 2X1% will be available after 16 hours. If X1% happens to fall below the clinical threshold needed to see a therapeutic effect, but 2X1% is above the clinical threshold, we see how an increased concentration can directly influence the duration of action (See Figure 1). This is exactly what we see with the new allergy product coming soon which contains olopatadine at 0.2%.
A clinical study has shown that olopatadine 0.2% does indeed have clinical activity that supports q.d. dosing, compared to b.i.d. use with the currently available olopatadine 0.1%. One obstacle to consider, however, whenever one increases a drug's concentration, is that the solubility limit may be approached. In the case of olopatadine 0.2%, it has inactive agents that increase the solubility of the solution at higher concentrations.
The discussion of tissue saturation leads to another interesting point. If one drop of a drug is able to saturate the tissue (recall that 95 percent of the drop may not even be available to the tissue) then, it should follow logically that dosing two drops sequentially should not increase a drug's duration of action. This is, in fact, what has been found. Further, on the same point, loading of a drug in most cases (except when required based on the mode of activity), also will not increase duration of action compared with a single drop.
Several studies have identified that the ideal instilled volume of pilocarpine is approximately 20 ml8-10— any additional fluid is either spilled over the lid margin or drained from the eye by the nasolacrimal duct, often within two to three minutes of instillation. These studies have demonstrated an important finding: Increasing drop size doesn't increase bioavailability.11 If using drops sequentially, it's clear that you should wait beyond the dwell time of the first drop before instilling the second. Even then, additive efficacy can't be expected; this is due to several factors, particularly saturation of the drug, which creates a reservoir in the eye and saturates the receptors. So, even if you use sequential drops, you won't double the effect. Additionally, the specific saturation levels and dose-response curves will differ from drug to drug depending on a particular agent's receptor selectivity. Therefore, the level of saturation may not directly correspond to the maximal clinical effect, and it depends upon a specific drug's selectivity or strength as a pharmacologically active agent.
Clearly, there's a trend toward creating drugs that have longer durations of action and, therefore, require less frequent dosing. There are multiple benefits of q.d. dosing, including increased convenience for the patient, a decreased occurrence of systemic side effects and the likelihood of better patient compliance.
In next month's column, we'll probe deeper into some specific new technologies and drug delivery.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals. Ms. Rosner is a research associate at Ophthalmic Research Associates in North Andover.
1. Stewart WC, Holmes KT, Johnson MA. Washout periods for brimonidine 0.2% and latanoprost 0.005%. Am J Ophthalmol 2001;131:6:798-9.
2. Sjoquist B, Stjernschantz J. Ocular and systemic pharmacokinetics of latanoprost in humans. Surv Ophthalmol 2002;47:S6-12
3. Sjoquist B, Basu S, Byding P, Bergh K, Stjernschantz J. The pharmacokinetics of a new antiglaucoma drug, latanoprost, in the rabbit. Drug Metab Dispos 1998;26:8:745-54.
4. Bourlais CL, Acar L, Zia H, et al. Ophthalmic drug delivery systems—recent advances. Progress in Retinal Eye Research 1998;17:1:33-58.
5. Lanier BQ, Abelson MB, Berger WE, et al. Comparison of the efficacy of combined fluticasone propionate and olopatadine versus combined fluticasone propionate and fexofenadine for the treatment of allergic rhinoconjunctivitis induced by conjunctival allergen challenge. Clin Ther 2002;24:7: 1161-74.
6. Crampton HJ. A comparison of the relative clinical efficacy of a single dose of ketotifen fumarate 0.025% ophthalmic solution versus placebo in inhibiting the signs and symptoms of allergic rhinoconjunctivitis as induced by the conjunctival allergen challenge model. Clin Ther 2002;24:11: 1800-08.
7. Spangler DL, Abelson MB, Ober A, et al. Investigation of the relationship between the eye and the nose in allergic rhinoconjunctivits: An evaluation of an eye drop (olopatadine 0.1% ophthalmic solution) nasal spray (mometasone furoate monohydrate nasal spray, 50mcg) and a systemic antihistamine (fexofenadine HCl 180 mg) on nasal and ocular symptoms using allergen challenge models (in press).
8. Patton T. Ocular drug deposition. In: Robinson J, ed. Ophthalmic Drug Delivery Systems. Washington, D.C.: American Pharmaceutical Association, 1980.
9. Mishima S. Clinical pharmacokinetics of the eye. Invest Ophthalmol Vis Sci 1981;21:504.
10. Sugaya M, Nagataki S. Kinetics of topical pilocarpine in the human eye. Jpn J Ophthalmol 1978;22:127.
11. Chrai S, Makoid MC, Eriksen SP, Robinson JR. Drop size and initial dosing frequency problems of topically applied ophthalmic drugs. J Pharm Sci 1974;63:333-38.