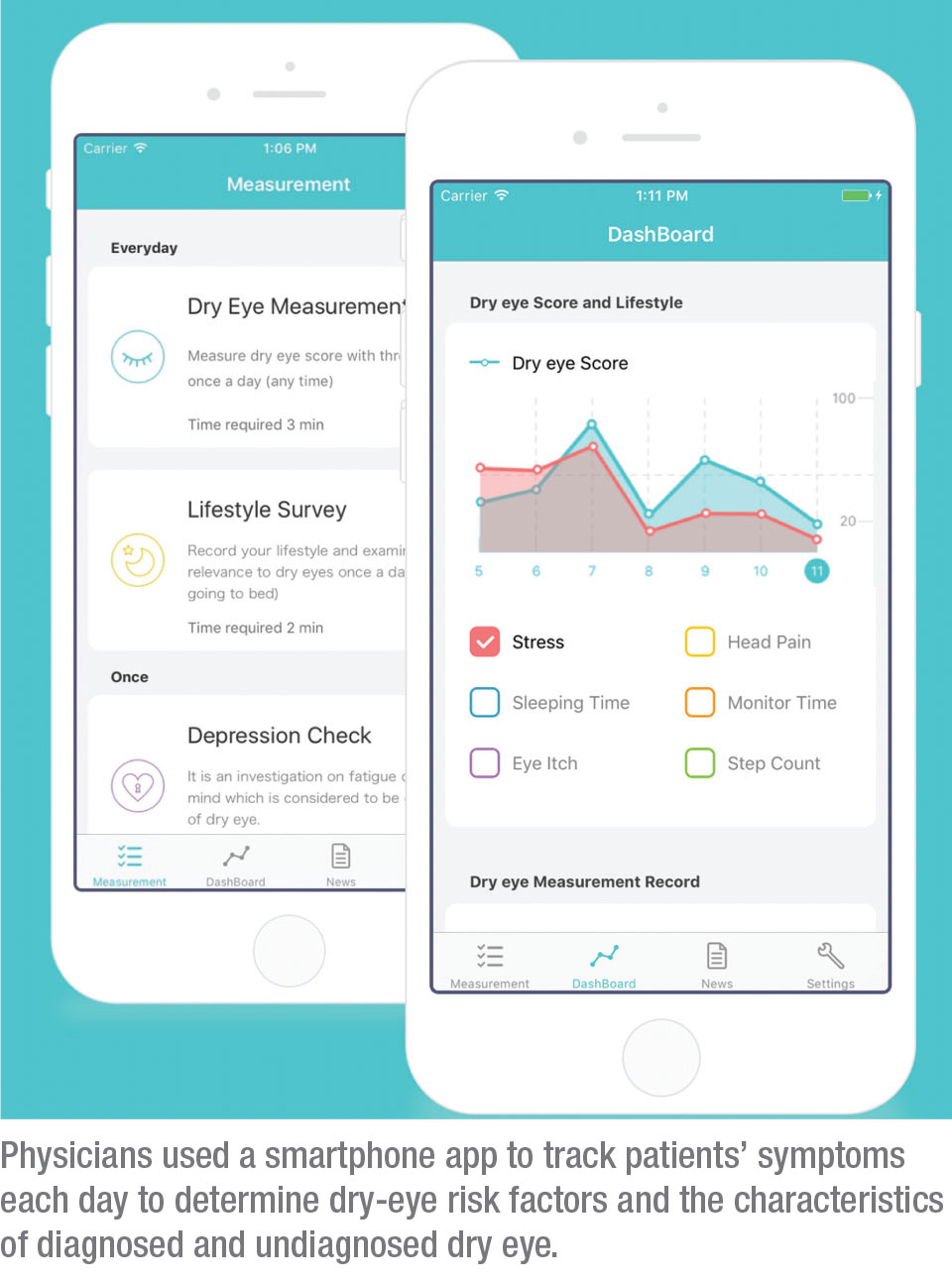
Taking advantage of big data and heavy smartphone use, a research team at Japan’s Juntendo University designed the DryEyeRhythm free mobile app with Apple’s ResearchKit to identify risk factors and characteristics of diagnosed and undiagnosed dry-eye disease. “This study is among the first to use a crowdsourced smartphone application to collect epidemiological data for dry-eye disease,” says Michael T. M. Wang, MBChB, fellow in ophthalmology at the University of Auckland, New Zealand, School of Medicine. The app documents symptoms, medical history and lifestyle habits. “One of the advantages of using an app to conduct clinical research is the potential for unlimited participation and no geographical restrictions or participation cost,” says Takenori Inomata, MD, PhD, MBA, of the Juntendo University Faculty of Medicine in the Department of Ophthalmology and one of the study authors.
 |
The cross-sectional, crowdsourced research included an electronic informed consent step in the smartphone app. A total of 21,394 records were identified in the app’s database; 11,485 were duplicate records, and after removing user records outside of Japan or with incomplete data, a cohort of 4,454 participants were enrolled in the study. Of the 4,454 users, 899 participants (27.3 percent) had diagnosed dry eye and 2,395 participants (72.7 percent) had undiagnosed symptomatic dry eye; 2,972 participants (66.7 percent) were women; mean age was 27.9 ±12.6 years.
Study participants reported daily subjective symptoms, such as ocular itching, stress levels and headache; and filled out disease-specific questionnaires, such as the Ocular Surface Disease Index (100-point scale; scores 0 to 12 indicate normal; 13 to 22 mild; 23 to 32 moderate; 33 to 100 severe dry-eye symptoms) and the Zung Self-Rating Depression Scale (total of 20 items; total score ranging from 20 to 80; ≥40 highly suggestive of depression).
Study participants were classified as having no symptomatic dry eye (defined as an Ocular Surface Disease Index total score <13) or having symptomatic dry eye (OSDI ≥13). The symptomatic dry-eye group was further divided into diagnosed and undiagnosed symptomatic dry eye.
The researchers used multivariate-adjusted logistic regression analysis to identify risk factors for the disease. They found that risk factors for symptomatic dry eye included younger age, female sex, allergic rhinitis, mental health disorders, digital device screen exposure time and contact lens wear. For undiagnosed symptomatic dry eye, associated risk factors included younger age, male sex, absence of a collagen disease, mental health disorders, ophthalmic surgery and contact lens wear.
“The identification of associated risk factors offers valuable information which might help to inform targeted health promotion strategies and/or opportunistic screening among those with a greater propensity of developing dry-eye disease, as well as risk factor reduction or modification strategies,” says Dr. Wang.
“With the exception of younger age, the remaining risk factors identified in the current study are in agreement with those previously reported in the literature,” Dr. Wang continues. “It’s possible, however, that the potential selection bias associated with participant recruitment among those that use digital devices in the current study might have contributed to the association between younger age and symptomatic dry eye detected in the current study. Only a low proportion of survey respondents (8 percent) were 50 years or older. Furthermore, moderate-to-severe dry-eye symptoms might also limit the use of digital devices, which may potentially contribute to a risk of under-sampling.”
“We were surprised to find a lot of symptomatic dry eye in younger males as undiagnosed dry eye,” says Dr. Inomata. Dr. Wang agrees, pointing out that “the high proportion (72.7 percent) of the study’s respondents with undiagnosed disease among those with symptomatic dry eye . . . represents a significant public health concern, particularly in the context of the high economic and societal burden of dry-eye disease.”
Dr. Wang says the data on risk factors that the study uncovered might translate to the clinic in terms of timely intervention. “Recent research suggests that early detection and treatment can help delay the progression of dry-eye disease,” Dr. Wang says. “Research surrounding risk factors of undiagnosed dry eye is particularly valuable and can contribute to the identification of barriers associated with disease detection and/or treatment, and might also prompt efforts of raising awareness among those who are less likely to contact health-care services.”
The researchers believe that, without their mobile app, identifying undiagnosed symptomatic dry eye would be more difficult. Still, they say the sample size of the study may still be insufficient for identifying risk factors that are only weakly associated with diagnosed and undiagnosed symptomatic cases of dry-eye disease.
Some other limitations of the study include sources of bias, such as recall bias, volunteer bias and self-reporting bias, as well as bias for age and socioeconomic factors, since the app was released for only iOS and iPhone.
Additionally, only the OSDI questionnaire was used for identifying dry-eye disease. Dr. Wang notes that “mobile health technology does not yet allow for the clinical evaluation of ocular surface signs, which would limit the ability to formally diagnose dry-eye disease according the recent global consensus Tear Film and Ocular Surface Society Dry Eye Workshop II criteria, which would require the presence of both clinical signs and symptoms.”
Clinical research is expected to improve through the use of artificial intelligence and big data, which make participant recruitment, communication and real-time data acquisition easier and more cost-effective.1 Dr. Inomata believes that mobile health technology will lead to the development of better preventive medicines. REVIEW
1. Inomata T, Iwagami M, Kakamura M, et al. Characteristics and risk factors associated with diagnosed and undiagnosed symptomatic dry eye using a smartphone application. JAMA Ophth 2020;138:1:58-68.



