Workup, Diagnosis and Treatment
 |
Shortly after the patient’s arrival at Wills, the differential diagnosis was broadened from chemical exposure, especially given the benign corneal exam with improving conjunctival injection and chemosis. Given the presence of vitritis and the initial concern for a possible infection, a vitreous sample was obtained, followed by intravitreal injection of vancomycin, ceftazidime and voriconazole. Vitreous cultures, blood cultures and HIV testing were all unremarkable. Careful B-scan ultrasound by a retina specialist didn’t reveal any evidence of rupture, and exploration was deferred.
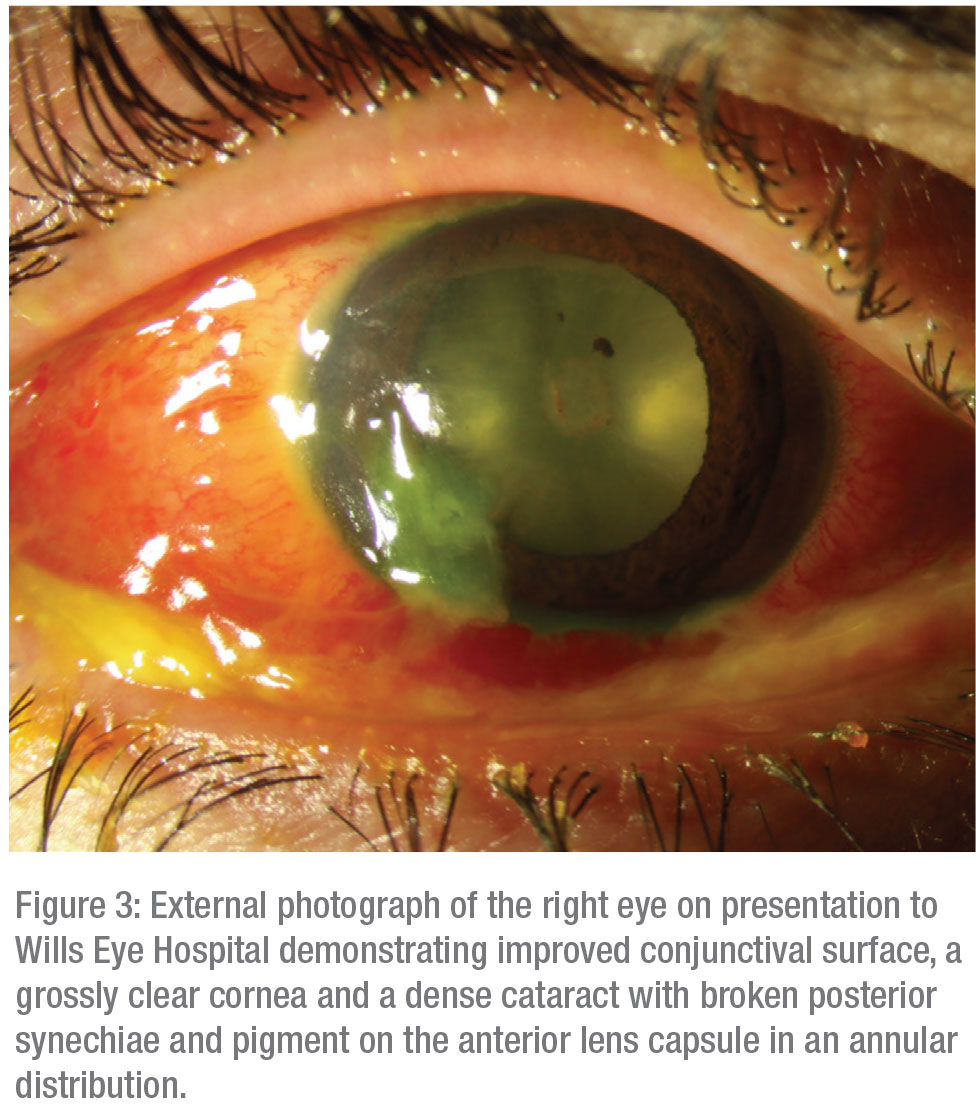
Despite the initial concern for infectious etiologies, including endogenous sources as well as penetrating inoculation, the onset and course of the patient’s vision loss wasn’t consistent with these entities. The presence of acute unilateral vision loss, a large RAPD, initial retrobulbar edema, proptosis and ophthalmoplegia pointed toward a diagnosis of “Saturday night retinopathy” with additional elements of orbital infarction, especially given the onset of symptoms following a prolonged state of unconsciousness. This diagnosis was also muddled by the presence of an acute onset cataract. Although no evidence of penetrating injury was discovered, the presence of pigment on the anterior lens capsule was suggestive of a Vossius ring. This was hypothesized to be due to blunt trauma to the right eye, likely occurring while intoxicated.
The patient was treated with topical steroids, cycloplegics, and lubrication. Repeat B-scan five days later showed resolved vitritis and a flat retina with improved choroidal thickening and resolved choroidal detachment. Topical steroids were slowly tapered. The patient was counseled on his poor visual prognosis. He was recommended to seek close follow-up with a local ophthalmologist to discuss possible cataract extraction after a period of sustained quiescence, but he was unfortunately lost to follow-up.
Discussion
Saturday night retinopathy is a rare, unilateral blinding condition, first described in 1974,1 that’s characterized by permanent vision loss in the setting of continuous external orbital pressure following substance-induced stupor and unconsciousness. Similar iatrogenic etiologies are well-documented in cases of unilateral vision loss following surgeries that require prolonged prone positioning against a headrest.2 The hypothesized mechanism involves the collapse of orbital vessels secondary to the external pressure on the orbit, in addition to a sedative-induced dampened response to painful stimuli that would otherwise act to alleviate the insult. Vision loss specifically is thought to be due to lack of blood flow through either the central retinal or ophthalmic artery with resultant ischemia, while other orbital signs like proptosis and ophthalmoplegia may be due to temporary obstruction and subsequent reperfusion of multiple small orbital vessels.2 One report documenting the fluorescein angiography and optical coherence tomography findings in a patient with Saturday night retinopathy noted delayed choroidal filling, delayed retinal filling and severe full thickness disorganization of retinal architecture with subretinal and sub-retinal pigment epithelium fluid, further supporting the hypothesis that ophthalmic artery occlusion plays an important role in the pathophysiology of this rare entity.3
Despite several confounding factors, including a traumatic cataract and chemical conjunctivitis, our patient demonstrated many classic features of SNR. One study cataloging three cases of SNR noted poor visual acuity ranging from no light perception to hand motion with large RAPDs in all subjects, similar to our patient’s examination findings.4 Additionally, two of the three patients in this study presented with periorbital swelling, proptosis and ophthalmoplegia, which improved to varying degrees over subsequent visits despite persistent visual loss, as was also observed in our subject. Further, our patient concurrently used cocaine in addition to opiates. Other studies have hypothesized that the powerful sympathomimetic and vasoactive properties of cocaine may exacerbate the ischemic insults of SNR.5
In summary, Saturday night retinopathy is a rare, blinding condition characterized by vascular obstruction from prolonged orbital compression during a substance-induced state of unconsciousness. Given that patients wake with severe ischemic vision loss in a scenario occurring outside of the hospital, no productive preventative measures or treatments are available. Knowledge of this entity is important for both ophthalmologists and emergency medicine providers, as the patients are often unable to give a detailed history of events due to their intoxication. As was seen in our case, our patient’s convoluted history and initial findings made diagnosis particularly challenging. REVIEW
1. Jayam AV, Hass WK, Carr RE, Kumar AJ. Saturday night retinopathy. J Neurol Sci 1974;22:4:413-8.
2. Hollenhorst RW, Svien HJ, Benoit CF. Unilateral blindness occurring during anesthesia for neurosurgical operations. AMA Arch Ophthalmol 1954;52:6:819-830
3. Williams AL, Greven M, Houston SK, Mehta S. Self-induced orbital compression injury: Saturday night retinopathy. JAMA Ophthalmol 2015;133:8:963-5.
4. Malihi M, Turbin RE, Frohman LP. Saturday night retinopathy with ophthalmoplegia: A case series. Neuroophthalmology 2015;39:2:77-82.
5. Van stavern GP, Gorman M. Orbital infarction after cocaine use. Neurology 2002;59:4:642-3.



