When patients with weak zonules present for cataract surgery, surgeons will need to get creative when implanting the IOL.
According to Richard Hoffman, MD, who is in practice in Eugene, Oregon, diagnosing zonular laxity is fairly straightforward. “Preoperatively, if patients have phacodonesis, a history of trauma or pseudoexfoliation, then you need to be prepared for weak zonules,” he explains. “And, if they don’t have phacodonesis, one very easy way of diagnosing zonular laxity at the beginning of the procedure is to push down on the lens to start the capsulorhexis. If you see a whole bunch of striae or folds, that usually implies that you’ve got mild to moderate zonular weakness. At that point, you have to decide whether you want to place capsule hooks or place a capsular tension ring.”
After the Diagnosis
“The first thing to consider is the severity of the weakness,” says Uday Devgan, MD, who is in practice in Los Angeles. “Am I able to just insert the lens into the capsular bag or maybe even have a sulcus lens with optic capture? Or am I going to need to suture in some sort of support for the lens or the capsule? That’s the difference between doing a routine surgery and possibly placing a capsular tension ring, which will take 10 minutes or less, versus doing a more complicated procedure in which I’ll have to suture in some type of support for the capsule or suture the lens in place, which will take 20 to 30 minutes.”
Dr. Hoffman agrees. “Everything depends on how loose the zonules are,” he says. “If the lens is frankly subluxed and moving around in the eye, I will usually just coordinate that with the retinal surgeon and have him do a pars plana vitrectomy and lensectomy. Then, I’ll scleral-fixate a posterior chamber lens. The latest technique I’m using is the Yamane intrascleral haptic fixation technique. However, it’s rare to have a patient whose whole lens is jiggling around. Some people try to rescue the lens with the capsular bag, do a rhexis, support it with hooks, and then sew in capsular prosthetic devices. It’s just a lot of work, and I find it’s a lot easier just to remove a very loose crystalline lens and scleral-fixate a posterior chamber lens in extreme cases.”
In most cases, patients just have a small amount of zonular laxity or weakness. “Most of the time, we can get by with just being very gentle during the procedure. If there’s a lot of capsular laxity but the lens isn’t frankly moving, then I’ll use capsule hooks, sometimes in combination with a capsular tension ring. However, lately, I’ve been moving towards just using the capsule hooks and then putting the capsular tension ring in after I’ve removed most of the cataract,” Dr. Hoffman explains.
 |
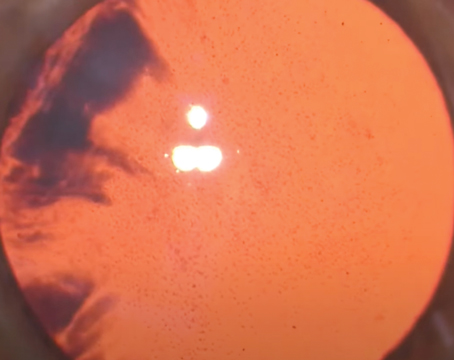
| A capsular tension ring is valuable in cases of weakening due to trauma. |
What’s the Cause?
After determining the severity of the weakness, surgeons will need to ascertain whether the weakness is due to a progressive disease or whether it’s due to trauma, so they’ll know whether the zonules will continue to deteriorate.
“There’s a difference between being hit in the eye with a car air bag or a left hook, versus a progressive disease, such as pseudoexfoliation or Marfan syndrome,” Dr. Devgan says. “With trauma, what you see today is what you will see over time. With progressive disease, the zonules will be worse in the future, and you’ll need to plan for that.”
He adds that, in patients with weak zonules due to trauma, surgeons can typically support the weak area with a capsular tension ring during surgery. “However, if the weakness is due to a progressive disease, you may do a capsular tension ring, and if there is really severe zonular loss, you may have to plan on sewing in a lens after removing the cataract,” he says. “Another option would be to put in an anterior chamber lens or plan some other alternative placement of the lens.”
According to Alan Crandall, MD, from the Moran Eye Center at the University of Utah, if the laxity was caused by trauma and is less than four to five clock hours, a capsular tension ring by itself will usually stabilize the lens. “But then, there are the progressive phenomena, such as pseudoexfoliation,” he notes. “These patients’ pupils don’t dilate well. You’ll also need to figure out how much zonulopathy currently exists.
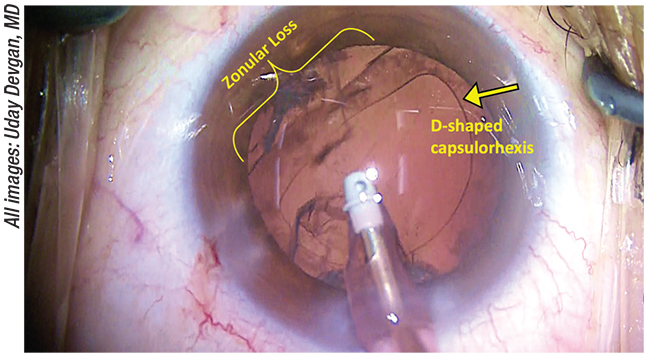
“One of the biggest clues is wrinkling in the anterior capsule as you start the rhexis,” Dr. Crandall continues. “If a patient has pseudoexfoliation, we don’t want to stress the zonules during surgery, so we make sure that we have a good hydrodissection, a 5.5-mm rhexis, and use pre-chop or some form of zonular-friendly debulking and cataract removal system. The miLoop (Carl Zeiss Meditec), for example, is good to use because the energy comes all the way up. The best technique depends on the hardness of the cataract. In pseudoexfoliation, with any zonular instability, I’m always going to put in a capsular tension ring. Additionally, you may need to use a capsular tension segment, such as a Cionni modified segment (FCI Ophthalmics), to suture.”
If the patient has zonular weakness due to trauma, Dr. Crandall recommends tearing toward the defect when performing the rhexis. “You want to use the good zonules for counter-traction. If they don’t have any stability, as in loose pseudoexfoliation, surgeons should start the rhexis and then put in an iris hook, a capsule hook or Grieshaber hooks (Alcon) in order to use them as counter-traction to continue the rhexis,” he says. “Once the cataract procedure has been performed, you will need to decide whether to place a Cionni segment, a capsular tension segment or two capsular tension segments.”
Suturing/Gluing
If the lens needs to be secured in the eye, there are a few options, and surgeons will need to determine which is best for their patient. “If there’s absolutely no capsular support, and the capsule is just shot, then we will sew the lens or attach it to the sclera,” Dr. Devgan explains. “It can be sewn to the sclera using various suture techniques, or it can be glued to the sclera. Additionally, there’s the Yamane technique that fixes the haptics of the lens to the sclera. These options are all scleral-based. If there is some support, then maybe sewing it to the iris would be helpful, as well.”
A new technique was recently described that uses 8-0 polypropylene sutures for four-point scleral fixation.1 Surgeons first mark four sclerotomy sites 2.5 mm from the limbus, and two scleral grooves are created in between. Two sets of polypropylene sutures are then passed through the IOL haptics, and the posterior chamber IOL is inserted behind the iris. The sutures are then pulled ab interno and tightened for optimal IOL centration. The sutures and the exposed knots are embedded in the scleral groove and are sealed with fibrin glue. This technique was performed uneventfully in nine cases, and the posterior chamber IOL remained stable for 10 months with no signs of subluxation, dislocation, tilt or suture-related complications, such as erosion or infection.
Additionally, the Yamane technique for transconjunctival intrascleral fixation of an IOL was recently prospectively studied in 100 eyes of 97 consecutive patients with aphakia, dislocated IOL or a subluxated crystalline lens, who underwent posterior chamber sutureless implantation of an IOL.2 This technique consists of making two angled incisions parallel to the limbus using 30-gauge thin-wall needles. The haptics of the IOL were externalized with the needles and were cauterized to make a flange of the haptics. The flange was then pushed back and fixed into the scleral tunnels. The IOLs were fixed with exact centration and axial stability.
Preoperatively, the mean best-corrected visual acuity was 0.25 logMAR units (somewhat worse than 20/32), which significantly improved postoperatively to 0.11 (around 20/25) at six months, 0.09 (a little better than 20/25) at 12 months, 0.12 at 24 months and 0.04 (nearly 20/20) at 36 months. Mean corneal endothelial cell density decreased from 2,341 cells/mm2 preoperatively to 2,313 cells/mm2, 2,240 cells/mm2, 2,189 cells/mm2 and 2,244 cells/mm2 postoperatively at six, 12, 24 and 36 months, respectively. Mean IOL tilt was 3.4 ±2.5 degrees.
Postoperative complications included iris capture by the IOL in eight eyes (8 percent), vitreous hemorrhage in five eyes (5 percent) and cystoid macular edema in one eye (1 percent). No patients experienced postoperative retinal detachment, endophthalmitis or intraocular lens dislocation.
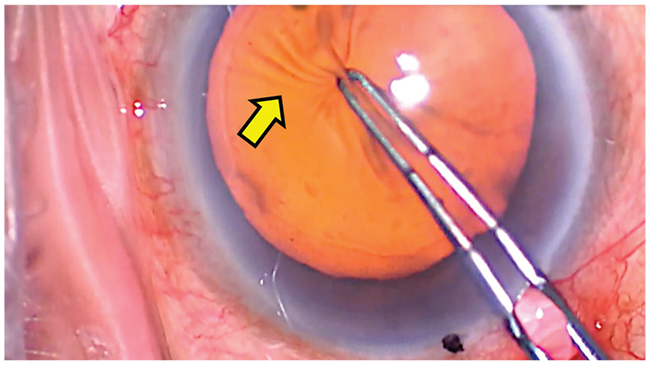 |
| A wrinkled anterior capsule (arrow) is a sign of weak zonules. |
Another option is to glue the IOL in place. A recent study found scleral-glued surgery to be a good option for fixating an IOL in eyes with pseudoexfoliation and poor zonular integrity or absent zonular support.3 The study included 28 eyes, and the indications for scleral-glued IOL fixation included late endocapsular IOL dislocation (75 percent), exchange for iris-fixated IOL due to complications (14 percent), subluxed crystalline lens (7 percent) and aphakia after complicated cataract surgery (4 percent). More than half of eyes (54 percent) had pre-existing glaucoma at the time of scleral-glued surgery. Eight eyes (29 percent) experienced postoperative ocular hypertension that required escalated medical management. The investigators recommend paying special attention to intraocular pressure control following surgery, because it can be less predictable in eyes with pseudoexfoliation, with or without pre-existing glaucoma. At the final follow-up, corrected distance visual acuity was equivalent to or better than it was preoperatively in 89 percent of eyes.
Decentered IOLs
Some patients, especially pseudoexfoliation patients, experience weak zonules after cataract surgery, which can cause their lens to decenter. “This is common, and I think we’re going to see more cases like this,” Dr. Hoffman says. “When I lectured about this 10 years ago, I recommended that people place capsular tension rings in pseudoexfoliation patients, even when there doesn’t appear to be any zonular weakness, because a certain percentage of these patients end up having subluxed lenses that are in the capsular bag seven or eight years down the road. The zonules have just degraded with time.”
In these cases, Dr. Hoffman says he usually fixates the haptics to the sclera using a lasso technique. “This is a lot easier if the haptic is in the meridian of the subluxation, and it’s even easier if the patient has a capsular tension ring, because you don’t have to worry about where the haptics are,” he says. “You just fixate the capsular tension ring to the sclera using either 9-0 Prolene or CV8 Gore-Tex, which usually works. These patients tend to be elderly, and it’s probably going to take 15 to 20 years or more for 9-0 Prolene to degrade. In a younger patient, Gore-Tex makes a lot of sense.”
Dr. Devgan adds that the treatment depends on the type of lens and how decentered it is. “If it’s a three-piece lens that you can reach from the anterior segment, then you can just keep that lens in the eye and sew it in place,” he says. “Usually, sewing it to the back of the iris or to the sclera is sufficient. If it’s a single-piece lens, it’s a little tougher to suture in place, but it still can be done. If the lens is very far dislocated into the eye, you may just have to take it out via a pars plana approach. Depending on your comfort level, you may want to ask for the assistance of your vitreoretinal colleagues. Remember that when your patient is sitting at the slit lamp, the lens in the eye is perpendicular to the floor. However, when you lie the patient on the operating room table, if the lens isn’t well-supported, the lens can fall way back into the vitreous, which makes the situation much tougher,” he says. REVIEW
Dr. Devgan owns and runs cataractcoach.com. Dr. Crandall is a consultant for Iantech, which was recently purchased by Carl Zeiss Meditec. Dr. Hoffman has no financial interests related to the products/companies mentioned in this article.
1. John T, Tighe S, Hashem O, Sheha H. New use of 8-0 polypropylene suture for four-point scleral fixation of secondary intraocular lenses. J Cataract Refract Surg. 2018;44:12:1421.
2. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124:8:1136-1142.
3. Ragam A, Ritterband DC, Waisbren ED, Mathew-Padiyedathu J, Kang J, Seedor JA. Clinical outcomes and intraocular pressure control after scleral-glued intraocular lens insertion in eyes with pseudoexfoliation. J Glaucoma. 2018;27:2:164-169.