In this year's survey of refractive surgeons in the American Society of Cataract and Refractive Surgery, the news is mixed. Though LASIK volumes remain flat, so, too, do the reported cases of ectasia, giving surgeons something to feel good about.
This year, 634 physicians (13 percent of the ASCRS membership) responded to the survey. Here are some of the highlights.
Procedure Volumes
Though more PRK procedures were performed by the respondents in 2008 compared to 2007 (229,000 vs. 160,000), the number of LASIK cases has fallen from 856,000 to 759,000, leading to a diminished combined overall surgical volume of 988,000. This is the third year in a row that the overall volume has hovered around the million mark.
"PRK continues to go up as LASIK continues to go down," observes Dr. Duffey. "In terms of percentage of total volume, LASIK is at 76 percent with PRK at 24. However, as LASIK has continued to drop, and the overall numbers continue to decrease, the proportion of PRK cases is actually going up. I think this is a result of a conservative movement that makes us more willing to do PRK if we have any doubt about the risk of ectasia or any other problems." Dr. Duffey also points out that, though there is no growth, the absolute number of procedures is still around a million, so it's not as if it's dropped precipitously.
Only 21 percent of surgeons say they perform more than five LASIK cases per month (vs. 26 percent in 2007), 9 percent do more than 25 (compared to 13 percent in 2007) and only 3 percent perform more than 75 per month (down from 5 percent in 2007). The number of PRK cases in each of these ranges has increased by a small margin. The highest point for these ranges of monthly volume came in 2003, when 51 percent said they performed more than five cases per month, 25 percent did more than 25 and 8 percent performed more than 75.
As to what will be necessary to turn things around, Dr. Duffey says three things affect LASIK volumes: "the economy; the economy and the economy. ... The good thing is that when the economy picks up again, there will be a lot of people who have been standing on the sidelines who will have it done."
Procedures of Choice
Phakic intraocular lenses continue their march to the top of the popularity charts for high myopes (-10 D on the survey). In 2005, "waiting" was the most popular option (36 percent) followed by LASIK (25 percent) and phakic lenses (24 percent). However, since that time, phakic IOLs have increased in popularity for this segment of the refractive population, and the percentage of respondents who say they prefer them is 40 percent in this year's survey vs. 20 percent for LASIK and 24 percent for waiting. "Phakic IOLs certainly have surpassed LASIK in high myopes," says Dr. Duffey. "This is because surgeons would rather not remove too much corneal tissue with LASIK and then run a higher risk for ectasia."
In the hyperopic realm, it's refractive lens exchange that's making strides. For the +3 D hyperope, LASIK is still the most popular, with 46 percent of respondents preferring it. Lens exchange is gaining converts, though, and a quarter of the surgeons say it would be their procedure of choice. Just four years ago, only 10 percent of the surgeons preferred RLE and 70 percent preferred LASIK for these patients. For high hyperopes (+5 D), it's virtually no contest: 54 percent of ASCRS surgeons prefer RLE, compared to 9 percent for LASIK. Thirty percent would wait.
In the refractive-lens arena, though the percentages are still small, an interesting trend is emerging: Surgeons are becoming more likely to implant phakic IOLs bilaterally, a procedure once roundly vilified. "Fourteen percent say they're willing to do both eyes at the same sitting," says Dr. Duffey. "Fourteen percent isn't huge, but it's one in seven.
Though it's not the standard of care yet, it's a trend that's increased each year for the past four years, going from 6 to 10 to 11 to 14 percent. Why? Like anything else, surgeons are trying to keep costs down as much as they can while still providing good medicine for patients. So, I think some people are starting to say, 'You know what? In the right, controlled environment, if things go perfectly with the first eye, I'm willing to do the second."
The preferred surgery for presbyopia is once again monovision, with 43 percent of surgeons preferring it. Micro-monovision, in which the surgeon leaves the non-dominant eye a little less nearsighted than he would with conventional monovision, is second at 19 percent. Fifteen percent of surgeons would implant a ReSTOR lens, 14 percent prefer the Crystalens and 3 percent like the ReZoom.
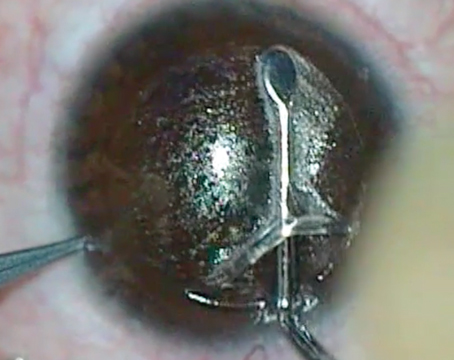
Flaps and Ectasia
Mainly in an effort to avoid ectasia, surgeons are moving toward thinner flaps. Though 120-µm to 130-µm flaps are still preferred by the highest percentage of surgeons (50 percent) the percentage of surgeons who prefer 100-µm flaps jumped from 20 percent in last year's survey to 32 percent this year, while proponents of thicker 150- to 160-µm flaps decreased to 14 percent. Only 4 percent prefer 180-µm flaps. "The number of surgeons preferring 100-µm flaps has grown consistently for the past five years," avers Dr. Duffey. "Both femtosecond lasers and microkeratomes can create thin flaps, as microkeratomes have seen the development of better heads that have enabled them to make thin flaps consistently. Again, these thin flaps give us more room for corneal treatment and less risk for weakening the cornea.
"The gold standard for residual stromal bed thickness used to be 250 µm, but it's creeping higher," Dr. Duffey observes. "Going back five years, at that time 75 percent of surgeons thought 250 µm was fine. This year, it's 52 percent. The really nice finding is that the total reported number of cases of ectasia is stable and hasn't grown for the past two or three years. We've gotten more conservative, have a better understanding of ectasia and we have better tools. I hope we'll see ectasia numbers decrease over time rather than continue to grow. That's certainly been the case with the data here."