 |
After voluntarily recalling Susvimo (ranibizumab injection) in October 2022, Genentech announced in July the reintroduction of the ocular implant for the treatment of wet age-related macular degeneration.
Susvimo is implanted surgically and refilled once every six months with a needle designed specifically for the implant. It was initially approved by the FDA in 2021 for the treatment of wet AMD in eyes with at least two prior anti-VEGF injections.
“We’re pleased to reintroduce Susvimo, a unique therapeutic approach shown to provide an effective alternative to regular eye injections by preserving vision with two refills per year in Phase III study patients with wet AMD,” the company announced in a formal statement.1
Genentech took the implant and tool assembly kit, including the drug vial and initial fill needle, off the market after it investigated reports of septum dislodgement in the port delivery system in patients during the Phase III trial program. The recall didn’t include the Susvimo 100 mg/ml drug vial or refill needle in order to allow retina specialists to continue refill-exchange procedures in those patients with an existing implant.
In a letter sent to health-care providers first announcing the recall,
Genentech said, “During an investigation into septum dislodgement cases in the port delivery system with ranibizumab Phase III clinical trial program, we identified a need for additional testing of the commercial implant supply. This additional testing of our commercial supply involved repeatedly puncturing Susvimo implants with a needle, to evaluate performance of the septum of the implant over the long-term via multiple refills. The results showed that some implants did not perform to our standards. Hence, a pause in all new implantations is required.”2
According to Jason Hsu, MD, a retina surgeon at Wills Eye Hospital in Philadelphia, who was part of the Phase III trials for Susvimo, as the company alluded to in its statement, the implant includes a septum for the needle to penetrate. “The septum creates a barrier to prevent any efflux of the drug into the subconjunctival space,” he explains. “However, in the reports of dislodgement, the glue of the septum wasn’t holding, essentially causing the septum to drop into the tip of the implant and preventing any refills.”
Among the changes to the implant were the doubling of the bonding strength of the septum component, as well as lubrication of the refill needle, which allows it to be inserted more smoothly and reduces the insertion force, notes Dr. Hsu.
“In my experience inserting these devices, septum dislodgement wasn’t a major issue,” he says. “We did see it happen in a couple of patients, but we witnessed dislodgement of the entire implant into the eye during the refill procedures. Some of that had to do with the amount of pressure it took to insert the needle into the device for refills. The changes made to the refill needle add a little bit more reassurance that it won’t require as much pressure, so this should hopefully make it much safer for the long term.”
The U.S. Food and Drug Administration has given a post-approval supplement to the Biologics License Application for Susvimo, reflecting these updates. Genentech also said it will work to make Susvimo available in the United States in the coming weeks.
“As for those who did have the original Susvimo implant, now that a new device is FDA approved, they’ll need to have it exchanged at some point, which is a bit of an inconvenience to undergo another surgery,” continues Dr. Hsu. “But I think these long-lasting, anti-VEGF options are a huge benefit to everyone, patients and clinicians, in terms of burden of care. I’m happy to see it’s back on the market because I think it will allow us to have another option for patients who need very frequent treatments. This potentially means they don’t need to come back to the office as often for repeated intravitreal injections.”
1. Genentech to Reintroduce Susvimo for People With Wet Age-Related Macular Degeneration (AMD). https://www.gene.com/media/press-releases/15031/2024-07-08/genentech-to-reintroduce-susvimo-for-peo. Accessed July 18, 2024.
2. Voluntary recall of the SUSVIMO Ocular Implant. https://www.gene.com/download/pdf/Susvimo_DHCP_Important_Prescribing_Information_2022-10-18.pdf. Accessed July 18, 2024.
Eye Length’s Relation to Glaucoma Severity, Progression
Research has suggested a clear relationship between myopia and glaucoma; axial elongation in myopic eyes stretches posterior ocular structures, resulting in progressive thinning of the retina, choroid and sclera and a higher susceptibility of lamina cribrosa deformation. In turn, these patients are subjected to a greater likelihood of glaucomatous optic disc changes. With the knowledge that axial length and glaucoma are related, a recent study aimed to determine whether there is a difference in inter-eye glaucoma severity and progression in patients with asymmetric axial length.1 The results revealed that glaucoma tended to be more severe and to progress faster in the longer eye.
The long-term observational study included 190 eyes of 95 glaucoma patients with asymmetric axial length (>1 mm difference between eyes) from a university hospital in Korea. The researchers classified each person’s eyes as the “longer eye” and “shorter eye” then performed an analysis on baseline and follow-up clinical data. The mean patient age was 51 years, and the mean follow-up period was just over 10 years.
Here are some of the main findings from the study:
- There was no difference in baseline intraocular pressure or central corneal thickness between longer and shorter eyes.
- Several baseline disc parameters were greater among longer eyes, including ovality index, beta-zone and gamma-zone parapapillary atrophy.
- In baseline OCT data, the thickness of the RNFL and ganglion cell-inner plexiform (GCIPL) layer was reduced in longer eyes vs. short eyes.
- The mean deviation and visual field index values were significantly lower in the longer eyes according to a baseline visual field test.
The researchers also reported differences in glaucoma progression between longer and shorter eyes. The following rates of change were greater in longer eyes: superior GCIPL (longer eyes: -0.65 µm/yr, shorter eyes: -0.40 µm/yr), mean deviation (longer eyes: -0.40 dB/yr, shorter eyes: -0.21dB/yr) and visual field index (longer eyes: -0.92 percent/yr, shorter eyes: -0.46 percent/yr).
“The greater the difference between the mean IOP and beta-zone parapapillary atrophy area between inter-eyes, the greater the difference in the rate of change of RNFL and GCIPL,” the study authors pointed out. Furthermore, they added, “the greater the difference in IOP fluctuation, the greater the difference in the rate of change between mean deviation and visual field index.”
All these observed differences between clinical parameters of longer vs. shorter eyes “provide insights into the nuanced nature of glaucomatous changes associated with axial length dissimilarities,” the authors noted. When evaluating patients with an inter-eye axial length difference of more than 1 mm, it may behoove ophthalmologists to consider that—based on the findings of this study—the longer eye may experience structural differences in the optic nerve head (larger ovality index and parapapillary atrophy area), greater thinning of the RNFL and GCIPL and more rapid change in mean deviation and visual field index.
“Longer eyes, as characterized by structural variations at baseline and an accelerated rate of glaucomatous change, exhibit a higher susceptibility to disease severity and progression,” the researchers concluded in their paper.
1. Huh MG, Jeong Y, Shin YI, et al. Assessing glaucoma severity and progression in individuals with asymmetric axial length: An intra-patient comparative study. Ophthalmology. July 15, 2024. [Epub ahead of print].
Bilateral, Same-day Surgery Safe According to U.K. Study
Increased efficiency at surgical centers and negligible risk argue for the adoption of same-day dual cataract removal in regions where demand far outstrips supply. However, widespread adoption of such a practice would require dramatic logistical and financial changes that are not in the offing any time soon. The Centers for Medicare and Medicaid Services have yet to bless such a protocol, all but stopping it in it tracks.
Nevertheless, the experience of surgeons outside the U.S. gives us a window into outcomes we could anticipate if circumstances change. In the U.K., immediate sequential bilateral cataract surgery (ISBCS) was introduced into government-sanctioned guidelines in 2017 and has become increasingly popular there, but still only comprises 0.5 percent of all cataract operations performed nationally.
The Buckinghamshire Healthcare NHS Trust redesigned its service to routinely offer ISBCS and is now considered a leading provider of the service in the U.K. As such, it audited its cataract operations performed in 2022 to gain greater insight on the spread of the newer approach. In total, 4,652 cataract operations were performed; 10.7 percent (n=498) were operations using the ISBCS approach on 249 patients. Trainees performed 32.5 percent of these cases, and there were only two intraoperative complications, which both occurred during the second eye operation. One of these was a suspected suprachoroidal hemorrhage while the other was a posterior capsular rupture post lens implantation. Postoperative complications included one retinal detachment needing a vitrectomy following uncomplicated ISBCS and five instances of Irvine-Gass syndrome managed medically.
In a recent article for the journal Eye, the study authors relay that, “from this data, ISBCS does not pose a greater risk to patients in terms of complications” and note that “with appropriate preoperative counseling, patients listed for unilateral surgery can be converted to ISBCS on the day of operation to fully utilize theatre capacity. Patients listed for ISBCS can also be converted to unilateral surgery on the day of operation when surgeons need time to deal with complications safely.”
In their discussion, the researchers further elaborate on the benefits this dual procedure may provide. They explain how doing ISBCS is quicker to perform on one patient than doing two separate cataract operations on differing patients due to preoperative review, patient maneuvering, setup times and postop counseling, which are all quicker on the day, potentially meaning that “this time saving could allow for more operations to be carried out in a single theatre session,” the authors point out.
A number of patients seem to prefer this method, too, as one study found 45 percent of patients on NHS cataract surgery waiting lists would undergo ISBCS if offered, while another study reported 36 percent of NHS patients accepting ISBCS when offered.
The investigators also argue that the one patient who experienced a macula-on rhegmatogenous retinal detachment six weeks after operation had a better outcome than she would have receiving the surgeries separately. This is because the detachment likely would have occurred before the second eye operation, thus causing a long delay before operation on that eye, which would result in worse vision and greater morbidity while recovering from the detachment. As well, this may have caused her to decline the operation in the second eye, resulting in long-term increased morbidity.
However, the authors highlight that “perhaps the greatest impact of ISBCS in years to come will be the flexibility it provides to adapt surgical lists in real-time with no additional administrative burden.” As they outline, a surgical list may consist of ISBCS cases but given any complications, surgeons may modify the procedures for the day to accommodate for increased time, dropping the procedures to only perform on one eye. Conversely, patients may be given the opportunity to opt out of the second operation on the day either before the operation or after the first eye’s completion, offering greater patient choice.
1. King, C., Botcherby, E.J., Adams, M. et al. Implementing immediate sequential bilateral cataract surgery at Buckinghamshire Healthcare NHS Trust. Eye (2024). https://doi.org/10.1038/s41433-024-03202-1.
Ophthalmology Groups Respond to GLP-1/NAION Data
Earlier this month, researchers at Harvard University published the results of their recent study, which observed an increased risk of nonarteritic anterior ischemic optic neuropathy in patients taking semaglutide for type 2 diabetes or weight loss. Semaglutide, a glucagon-like peptide receptor agonist (GLP-1 RA), is the active ingredient in Ozempic and Wegovy, two medications being prescribed with increasing frequency across the United States, adding to a cause for concern about the study’s findings.
The American Academy of Ophthalmology and the North American Neuro-Ophthalmology Society recently released a statement responding to the study and commenting on its potential implications for clinical practice. The stance of the two organizations is that, while the observed association between semaglutide and NAION of this study is “interesting,” more research is warranted to confirm whether the relationship is causal.
“The type of study conducted here helps identify potential links between GLP-1 treatment and NAION, but it’s not the type of study that can show the treatment caused NAION,” states Andrew Lee, MD, a clinical spokesperson for the American Academy of Ophthalmology and a neuro-ophthalmologist at Houston Methodist Hospital, in a recent Vision Monday article. Until more research is conducted, he says “patients should be aware of this information and, in consultation with their care team, make a careful, informed choice based on their individual risk profile.”
The AAO and the North American Neuro-Ophthalmology Society offered several other comments and concerns regarding the design and limitations of the study. For one, they point out that prior to its 2017 FDA approval, semaglutide was rigorously studied in multiple randomized controlled trials around the world. Notably, this is the first study to report an association between semaglutide and NAION.
They also noted that subjects in this study were either overweight, obese or had type 2 diabetes, the latter of which is an established risk factor of NAION, with others including heart disease, history of heart attack, high blood pressure and sleep apnea. However, the study authors did assert that they controlled for these potential confounders in their analysis.
Another potential limitation of the study according to the AAO and the North American Neuro-Ophthalmology Society was that all patients included were seen at Massachusetts Eye and Ear in Boston. Because the specialty hospital sees a large percentage of NAION patients in the region, this could limit the generalizability of the findings.
The two organizations point out that semaglutide has previously been linked to other vision changes, such as blurred vision, worsening of diabetic retinopathy and macular complications, though these effects typically subside within three or four months.
Though the AAO and the North American Neuro-Ophthalmology Society don’t recommend that people stop taking semaglutide at this time, they reiterate that further research will help clarify the relationship between the drug and ocular events such as NAION.
Drugs and Systemic Diseases May Alter OCT Findings
Comparing inner retinal measurements against a reference database is vital to diagnosing and monitoring certain pathologies, including primary eye conditions like optic neuropathies, as well as visual pathway lesions and systemic diseases. Researchers recently performed a study that used optical coherence tomography to conduct measurements of the inner retina in a large sample of normal, healthy eyes. Furthermore, it assessed the association between various inner retinal measures, such as peripapillary RNFL, and physiological factors, demographics, non-ocular pathology and pharmaceutical drug use.
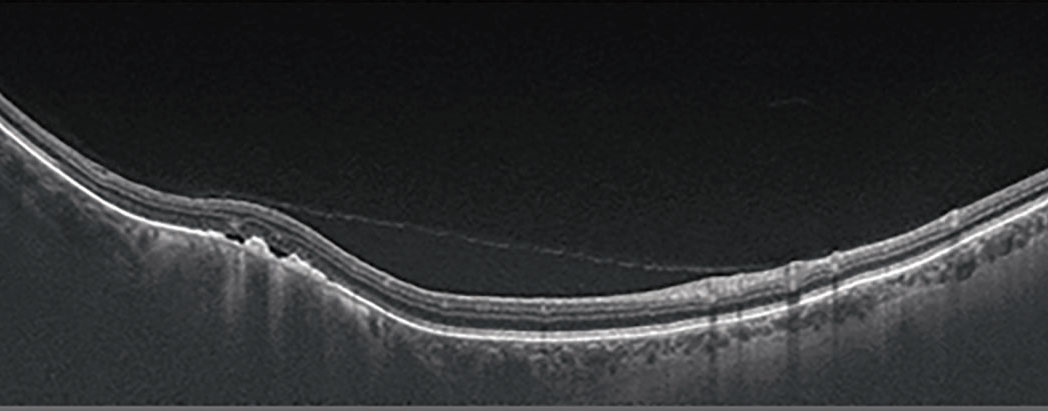 |
A recent analysis found that certain systemic diseases and drugs were significantly associated with deviations in standard OCT inner retinal measures, underscoring the importance of considering systemic health when assessing OCT data.
The study employed a retrospective, cross-sectional analysis of 705 consecutive participants with bilateral normal, healthy optic nerves and maculas. Mean age was 46.6 and 59 percent were women. One-third (33.1 percent) were white, 24.2 percent were Asian, 15.7 percent were categorized as “other” and 26.8 percent did not disclose their group. The mean refractive error was mildly myopic (-0.92 D). The most prevalent non-ocular pathologies were hypertension (10.5 percent), migraine (7.2 percent) and asthma (5.4 percent), while the most prevalent drugs were lipid-lowering agents (15.7 percent), ACE inhibitors (9.5 percent) and diabetes drugs (7.4 percent).
Data such as vertical cup/disc ratio, cup volume and macular ganglion cell layer-inner plexiform layer thicknesses were extracted from Cirrus OCT scans. These measures were then regressed against predictor variables that included participants’ physiology, demographics, non-ocular pathology and pharmaceutical drug use following the World Health Organization classifications.
The results showed that several non-ocular pathologies and pharmaceutical drug uses were significantly associated with deviations in standard OCT inner retinal measures, which exceeded the impact of other factors like age and intraocular pressure. Specifically, the use of systemic corticosteroids or sex hormones/modulators and the presence of diseases like vasomotor or allergic rhinitis were linked to thinner inner retina and larger optic nerve cup measures. Conversely, antineoplastic agents and the presence of liver or urinary diseases were associated with thicker inner retina and smaller optic nerve cup measures.
“Relatively novel findings included that the use of sex hormones/modulators were associated with compromised inner retinal integrity, while unspecified liver or urinary diseases and antineoplastic agents were associated with diffuse macular GCL-IPL thickening,” the researchers wrote.
1. Trinh M, OK, La M, Ly A. Linking physiology and demographics, non-ocular pathology and pharmaceutical drug use to standard OCT measures of the inner retina: The PPP project. Ophthalmic Physiol Opt. July 7, 2024. [Epub ahead of print].



