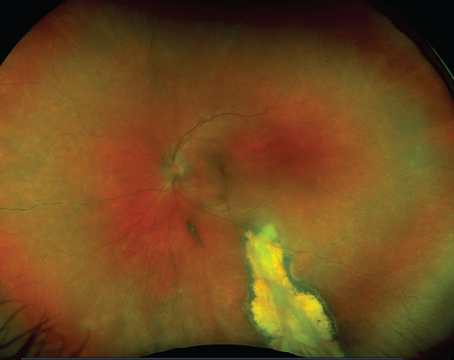
Laser photocoagulation and vit-rectomy surgery have been used successfully in treating severe visual loss from diabetic retinopathy. Despite their effectiveness, however, severe visual loss still develops. Focal photocoagulation from diabetic retinopathy has been effective for preventing visual loss from macular edema. However, even among eyes treated with focal photocoagulation, 15 percent still developed moderate visual loss. In addition, only 17 percent of those treated with focal photocoagulation developed moderate visual gain (See Figure 1).1
The next gain in treating retinopathy will likely be through prevention and modification of systemic factors. If vision is lost to macular edema or to complications of proliferative diabetic retinopathy, restoration is unlikely. Understanding the systemic risk factors and ways to control these factors will be crucial to how ophthalmologists will begin to prevent diabetic retinopathy.

Systemic Risk Factors
There are two common types of diabetes mellitus: Type I or, insulin-dependent diabetes mellitus (IDDM) and Type II, or non-insulin-dependent diabetes mellitus (NIDDM). Type II diabetes is more common, comprising 90 to 95 percent of all diagnosed U.S. cases of diabetes. IDDM patients have a higher risk of developing severe proliferative diabetic retinopathy than those with NIDDM. NIDDM does, however, cause a greater percentage of cases of severe proliferative diabetic retinopathy, because the prevalence of NIDDM is so much higher in the general population. Another very strong risk factor is the duration of diabetes. Unfortunately, neither risk factor is modifiable.
Glycemic Control
To date, the most effective preventive treatment is glycemic control. Two major trials have demonstrated the effect of "intensive" blood glucose control in reducing the incidence and progression of diabetic retinopathy.
The Diabetes Control and Complications Trial2,3 investigated the effect of intensive glycemic control. Patients with no retinopathy and those with existing mild to moderate non-proliferative retinopathy were randomized to either conventional or intensive treatment. The 1,441 patients in the DCCT were followed for a mean of 6.5 years.
In patients with no retinopathy in either eye, the progression of disease was similar between the two groups during the first 36 months. From that point on, the intensive group had a persistent reduction in development of retinopathy. During a mean follow-up of six years, intensive therapy reduced the risk of developing retinopathy by 76 percent (See Figure 2a).
 |
| Figure 2: Cumulative incidence of three-step change in level of retinopathy. (a) Primary prevention cohort represent eyes with no retinopathy. |
In patients with mild to moderate NPR, the intensive group had an increased risk of retinopathy progression in the first year. By 36 months, however, this group also had lower risks of retinopathy progression. Over the study's course, intensive therapy reduced the risk of progression by 54 percent (See Figure 2b).
In the United Kingdom Prospective Diabetes Study (N = 3,867), patients who were assigned to intensive glucose control had a 25 percent risk reduction in microvascular endpoints (P = 0.0099), including the need for retinal photocoagulation.4
 |
| Figure 2: (b) Secondary intervention represent eyes with some retinopathy already present. The intensively treated group shows statistically significant reduction in progression in both cohorts. |
There are important risks to intensive glucose control; the incidence of severe hypoglycemia in the DCCT was three times higher in the intensive group. The DCCT therefore recommends that therapy should be individualized. Therapy should be directed towards achieving the lowest glycemic level that is the safest in terms of hypoglycemic risk for each patient. Although most patients are aware of the benefits of good control, achieving it is difficult. Tight control requires significant effort by patients and their primary-care physician. Because of this extra effort, ophthalmologists should discuss its importance with patients at each visit.
Blood Pressure Control
Blood pressure can also be modified to prevent vision loss. The UKPDS randomized 1,148 hypertensive patients with type 2 diabetes to less tight (<180/105 mmHg) and tight blood pressure control (<150/85 mmHg) with the use of an angiotensin converting enzyme (ACE) inhibitor or a beta-blocker.5 With tight control, patients had a 34-percent reduction in progression of retinopathy and a 47-percent reduced risk of deterioration in visual acuity of three lines. Also reduced were deaths related to diabetes and strokes.
Unlike tight glycemic control, there were no clear adverse reactions to tight blood pressure control. Ophthalmologists may consider checking blood pressure, and if elevated, may need to encourage the patient and his primary-care provider to initiate better control. Like glycemic control, tight blood pressure control requires significant effort; almost one-third of patients required three or more medications to control their pressure.
Lipid Control
A sometimes forgotten systemic risk factor is lipid control. Hyperlipidemia contributes to the incidence and progression of both diabetic retinopathy and macular edema. Among insulin-using patients in the Wisconsin Epidemiologic Study of Diabetic Retinopathy, the presence of retinal hard exudates was significantly associated with increased serum cholesterol levels.6 In the Early Treatment Diabetic Retinopathy Study, patients who had elevated serum cholesterol or low-density lipoprotein levels at baseline were more likely to have retinal hard exudates.7 With increasing hard exudates, there is an increased risk of visual loss. Although this evidence is observational, control of serum lipids should be achieved, because it will reduce not only visual loss but also cardiovascular disease.
From Hyperglycemia to Retinopathy
Hyperglycemia can lead to the formation of free radicals (produced by glucose auto-oxidation), increased flux through the polyol pathway, and protein glycation. Free radicals can directly damage the retinal vasculature. High levels of glucose can lead to a buildup of intracellular sorbitol from increased aldose reductase activity. This rise in sorbitol is thought to result in osmotic damage to vascular cells.
High serum glucose also can lead to binding of glucose to protein side chains, resulting in the formation of dysfunctional proteins called advanced glycation end products (AGE). Finally, hyperglycemia may lead to protein kinase C (PKC) activation.
Protein kinase Cs are enzymes, distributed in many tissues, that transfer "high energy" phosphate groups to proteins. This phosphorylation results in regulation of the activity of certain proteins. High levels of AGEs, diacylglycerol (DAG) and free radicals from hyperglycemia is thought to activate protein kinase C. Activated PKC-ß sub-form, present at high levels in the brain and retina, in turn leads to the synthesis of a number of factors, including vascular endothelial growth factor. VEGF then can interact with the kinase domain receptor in the retinal vascular endothelium, leading to phosphorylation of other cytoplasmic signaling proteins.
VEGF might also lead to inflammation which then can directly damage the retinal vascular endothelium. Investigators have shown that VEGF can lead to increased leukocyte migration by elevation of adhesion molecules such as intercellular adhesion molecule-1 (ICAM-1). Increased leukocytes are seen with the onset of diabetic retinopathy.
Implications
To prevent diabetic retinopathy, investigators have suggested inhibiting VEGF production. Direct inhibition of VEGF production has been produced in experimental models by intravitreal injection of anti-VEGF antibodies, VEGF receptor chimeras (comprising the binding site of a VEGF receptor molecule complexed to an immunoglobulin), and strands of VEGF anti-sense DNA. Anti-sense DNA may inhibit the synthesis of the VEGF protein.
Oral inhibition of VEGF has also been attempted. One such compound is LY333531 (Eli Lilly Co., Indianapolis), which specifically inhibits PKC-ß and has been found to block vascular complications of diabetes, including abnormalities in retinal blood flow, neovascularization, and VEGF-mediated effects on permeability in animal models. In a small trial (N = 29) of diabetic patients with no or minimal retinopathy, the effect of LY333531 was compared with that of placebo over a one-month treatment period. The drug was well-tolerated, and no difference in adverse events was noted between the groups. Mean circulation time and retinal blood flow abnormalities were normalized in a significant and dose-dependent manner.8 Completed and on-going clinical trials will provide more information on its effectiveness in treating diabetic macular edema and retinopathy.
If VEGF acts through an inflammatory mechanism, anti-inflammatory agents should reduce the progression of retinopathy. Aspirin therapy in dogs has been shown to prevent certain features of diabetic retinopathy, but human studies have not confirmed this effect. The lack of efficacy in studies such as the ETDRS (650 mg/day) may be due to insufficient dosage. Animal studies typically study doses two to four times higher than that used in the ETDRS.
Preliminary studies of intravitreal steroid injection and steroid releasing intravitreal implants do appear to suggest a protective effect. More research is needed to confirm the role of inflammation and anti-inflammatory agents.
Medical treatment aimed at modifying systemic risk factors has been shown effective at preventing diabetic retinopathy. Understanding the systemic factors and new pharmacologic treatments that affect them will help the ophthalmologist achieve the next goal of treating diabetic retinopathy: prevention.
Dr. Fong is the associate director for clinical trials in the Department of Research and Evaluation, Southern California Permanente Medical Group, 100 S. Los Robles, Pasadena, CA 91101. Contact him at dsfong@ucla.edu.
1. Early Treatment Diabetic Retinopathy Study research group. Photocoagulation for diabetic macular edema. ETDRS report number 1. Arch Ophthalmol 1985 Dec;103(12):1796-806.
2. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977-86.
3. Davidson M. Why the DCCT applies to NIDDM patients. American Association of Clinical Endocrinologists: AACE Guidelines for Management of Diabetes Mellitus. Clin Diabetes 1994;12:141-144.
4. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study Group. Lancet. 1998 Sep 12;352(9131):837-53.
5. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:708-13.
6. Klein BE, Moss SE, Klein R, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XIII. Relationship of serum cholesterol to retinopathy and hard exudate. Ophthalmology 1991 Aug;98(8): 1261-5.
7. Chew EY, Klein ML, et al. Association of elevated serum lipid levels with retinal hard exudate in diabetic retinopathy. Early Treatment Diabetic Retinopathy Study Report 22. Arch Ophthalmol 1996 Sep;114(9): 1079-84.
8. Aiello LP, Bursell S, et al. Protein kinase C beta selective inhibitor LY333531 ameliorates abnormal retinal hemodynamics in patients with diabetes. Diabetes 1999;48:A