The Preop Process
Implant surgeons say that proper patient evaluation and education increase the odds of a good outcome.
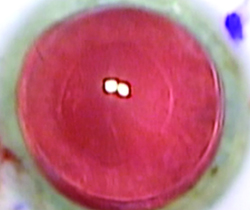
 |
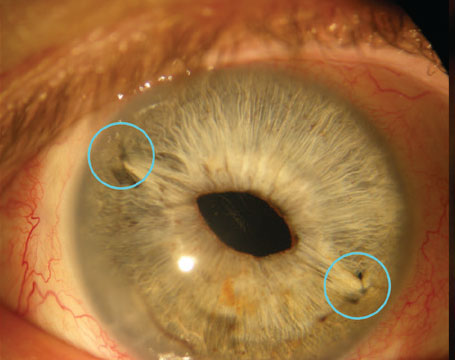
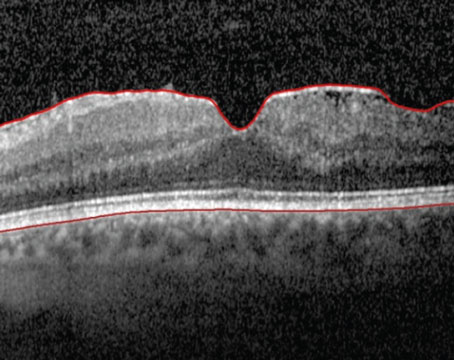
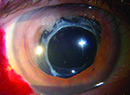
| Surgeons say it’s vital to protect the corneal graft in the post-PK patient undergoing cataract surgery. (All images courtesy Bryan Lee, MD.) |
Bryan Lee, MD, of Los Altos, Calif., says it may take some time for the eye to become stable, but it’s a crucial element to achieving success. “The patient should be one in whom the transplant appears to be able to last a while, you know you’re not going to have to do anything with the sutures and the cornea looks really good,” he says. “Ideally, the sutures should be out for three months or so, though that’s not a hard-and-fast rule. If you’re unsure, repeat your measurements to make sure they’re stable. Also, the patient must have realistic expectations and know that your biometry beforehand will be limited and that you’re doing something with the IOL that’s off-label, since patients post-corneal transplant have, by definition, irregular astigmatism, and the toric lens is labeled for patients with regular astigmatism.”
Matthew Wade, MD, assistant clinical professor of cataract, cornea and refractive surgery at the Gavin Herbert Eye Institute, University of California, Irvine, says it’s important to inform the patient about possible complications. “Have a frank discussion with the patient regarding the risks of intraocular surgery to the graft.” he says. “The patient should be informed that if the graft needs to be repeated in the future, the spherical and cylindrical power of the lens likely won’t match the new cornea and the lens may need to be exchanged. “If a graft fails, keep in mind that a DSAEK or a DMEK graft can be placed underneath it. This preserves the same anterior surface astigmatism that the toric IOL is treating. We haven’t seen any graft failures yet in our cohort of patients with PKPs who have received toric IOLs.”
Surgeons say the ultimate goal isn’t to get a hyper-accurate correction of the astigmatism, but simply to knock down the bulk of it so the patient can be comfortable wearing spectacles. “If there’s so much irregularity or irregular astigmatism in the cornea postop that the spectacle correction of their remaining cylinder won’t be satisfactory, and therefore the patient will have to go back to—or start—wearing a rigid contact lens that’s the rub,” says Dr. Miller. “This is because when putting a toric lens in an eye to correct the corneal cylinder, that toricity will show through into the spectacle plane when you cover the cornea and nullify the corneal astigmatism with the rigid contact lens. So, the patient will be really unhappy if you correct the cylinder inside the eye and he has to wear a rigid contact lens as well as spectacles to correct the astigmatism that you put in the eye with the toric lens.”
Dr. Miller says you can catch some clues as to who will be happy with his result postop. “If a patient has just had a transplant and is wearing a rigid contact lens to get the best vision, and thinks the quality of vision from spectacles is too low, that patient is highly likely to appreciate and demand really crisp vision after his cataract comes out,” he says. “He may not be a good candidate for a toric lens. However, if someone has dry eye and isn’t going to wear a contact lens no matter what, he is an ideal candidate for a toric IOL even if he’s got a fair amount of irregular astigmatism.”
Tips for Surgery
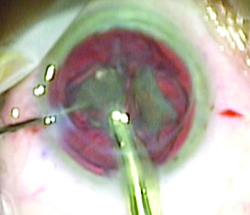
Surgeons say the cataract extraction and IOL implantation actually proceed in a fairly standard fashion with these patients, though the presence of the graft needs to be accounted for.
Dr. Wade says maintaining visibility is important in these cases. “Visibility through the graft can often be difficult so I have a low threshold for using trypan blue,” Dr. Wade says. “One nice way to keep the trypan away from the endothelium is to place it under Healon 5. During phaco I use extra viscoelastic to protect the endothelium. I place corneal cataract incisions as far away from the graft as possible. Also, I always place a suture in these patients as the corneal biomechanics are altered due to the corneal transplant. I’ll leave the suture in for a few weeks.”
Dr. Lee says the choice of viscoelastic may be a factor in certain cases, and that a dispersive type is probably best. “One consideration is, if you’re using the ORA intraoperative aberrometer, mixing viscoelastics and probably even using a dispersive viscoelastic may affect the accuracy,” he says.
 |
| Cataract incisions in graft patients should be peripheral, well away from the graft incision, surgeons say. |
Results to Expect
Even though these eyes have issues, and the bar for sharp vision isn’t as high as in a normal eye, surgeons have found that the results can still be more than satisfactory in the right patient.
Dr. Wade and his colleagues reviewed cases of toric IOLs in post-PK patients and found that the predictability of postoperative manifest astigmatism correction was good.1 “We had 21 eyes in the study, and 16 were 1 D or closer to the predicted postop manifest astigmatism,” he says. “The predicted astigmatism tries to take into account that we can only treat 4 D at the corneal plane with the toric IOLs we have available to us in the United States. The 4-D limit is one limitation of using toric IOLs to correct post-PK astigmatism.”
In another paper, this one from a group in New Zealand, researchers retrospectively analyzed 26 post-PK eyes that received either an Alcon AcrySof toric lens or a Rayner T-flex. At a follow-up of 14 months, the mean spherical equivalent decreased significantly from -3.67 to -0.58 D, and the astigmatism decreased significantly from -5.49 to -2.61 D. The surgeons were able to correct greater amounts of astigmatism since they had access to higher cylindrical lens powers that aren’t available in the United States.
In terms of vision results, in the study there was a significant improvement in the average uncorrected distance acuity from 1.12 to 0.45 logMAR (a little worse than 20/200 to just worse than 20/50). The best-corrected distance acuity improved from 0.70 to 0.15 logMAR (20/100 to a little worse than 20/25).2
In the right patient, Dr. Wade says that a toric lens offers benefits that an incision can’t match. “When you place a toric IOL in a post-PK patient,” he says, “you’re not only correcting the astigmatism, but the spherical refractive error, as well.” REVIEW
Dr. Miller is a consultant for Alcon. Drs. Wade and Lee have no financial interest in the products mentioned.
1. Wade M, Steinert RF, Garg S, et al. Results of toric intraocular lenses for post-PK astigmatism. Ophthalmology 2014;121:3:771.
2. Lockington D, Wang E, Patel D, et al. Effectiveness of cataract phacoemulsification with toric intraocular lenses in addressing astigmatism after keratoplasty. J Cataract Refract Surg 2014;40:12:2044-9.