People will forgive a lot of things if they get something for free. If a free lunch is a little cold, no problem. When the free vacation's hotel is a little old, that's OK, too. But when they pay for something, especially when they pay a good deal of money for it, almost nothing will be forgiven. As many surgeons will attest, this is the situation the ophthalmologist faces when he implants a premium intraocular lens. Patients have invested a lot of money in their decision to have such a lens implanted, and they've invested a lot of time in making sure their lens choice works for their lifestyle. Though they may stop short of asking for perfection in the postop result, they'd like it to be really, really good. Unfortunately, though premium lenses often give good outcomes, an occasional patient is less than thrilled.
Here are tips on how you can use laser vision correction—either surface ablation or LASIK with the IntraLase—to satisfy, or maybe even impress, such a patient.
Maximize Vision
Though an enhancement with laser vision correction may ultimately be called for in the premium-lens patient, you should try the simple things first for patients with less-than-optimal vision. In the first two or three months after cataract surgery, the three major causes of mediocre vision you should make sure to address are cystoid macular edema, ocular surface disease and posterior capsule opacification. You can sometimes avoid the need for refractive surgery altogether if you successfully treat these problems.
When addressing CME, optical coherence tomography is the most important tool you can have. OCT is sensitive enough to help you identify mildly clinically significant CME that might not bother a typical cataract patient but would be enough to decrease the effectiveness of a presbyopic lens. If you see CME, even of the mild variety, treat the patient aggressively with a non-steroidal anti-inflammatory drop—even more aggressively than you'd usually treat CME.
In cases of ocular surface issues, proper management often stretches back to the preop period, where possible surface problems are identified, noted to the patient and aggressively managed. Be sure to watch for irregular epithelium or punctate keratopathy after the patient's intraocular pressure measurement and retinal exam, and treat blepharitis with lid hygiene and antibiotics, and dry eye with lubricants and cyclosporine if necessary. Postop, you may have to recommend a course of artificial tears and/or Restasis to rehabilitate the ocular surface and sharpen the patient's vision.
If you suspect that the posterior capsule may be the culprit behind the disappointing vision, it can be difficult to sort out whether it's truly the capsule (and therefore you have to open it) or it's actually the patient's ability to neuro-adapt to the IOL. One of the best ways to distinguish whether it's the capsule causing symptoms is to review the early postop vision and history. If the patient was very happy for the first several days, and then had progressive worsening of symptoms, the capsule is likely to blame, especially if the OCT of the macula is normal. In these cases, make sure you're comfortable exchanging an implant with an open capsule, because there will be instances where you're sure it's posterior capsule opacification and a posterior capsulotomy results in a little improvement, but the patient ultimately decides he's not happy with the lens and you have to exchange it. In those cases, you're not only dealing with a lens exchange, but also a vitrectomy. Though this can be a daunting proposition, the ability to offer the patient a lens exchange is a useful tool.
The Laser Option
Even if you eliminate things such as CME and ocular surface disease, the patient may still have spherical or astigmatic refractive error that warrants some type of laser vision correction. Here are some considerations.
The decision about whether to use LASIK or PRK is a choice similar to that in patients without IOLs. So, if the patient has corneal disease such as basement membrane dystrophy, incisions from previous surgeries, a borderline corneal depth or unusual topography, do a PRK. However, if it's someone with a normal cornea, I like to do LASIK with an IntraLase-created flap.
First, you may wonder what is an acceptable result with a premium lens that wouldn't necessitate a postop refractive procedure. In my experience, on the low end, we've had some unhappy patients with 0.5 D of sphere or cylinder. It can be helpful to have such patients try glasses for a while to see if they can appreciate the difference in vision with the refraction. At such a low level of error, they're effectively spectacle-independent and simply would like their vision to be a little better. Ultimately, it may not really be worth going back to surgery for such a low correction. A spherical or astigmatic error of 1 D would probably be worth an enhancement, however. Overall, our enhancement rate in presbyopic IOL patients is currently 12 percent.
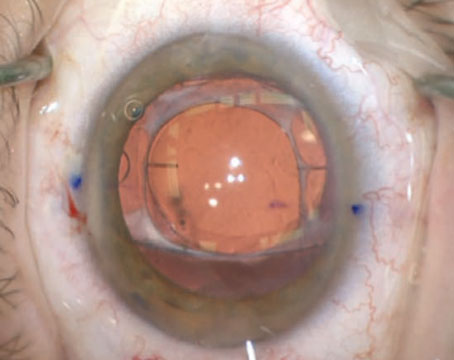
When dealing with an unhappy toric IOL patient, your first inclination may be to try to rotate the IOL onto its ideal axis. However, we've found that rotating might not always be the best alternative. John Berdahl, MD, a fellow at our practice in 2009, developed a computer spreadsheet that gives the cylindrical effect of rotating the lens, so you can determine whether rotation or laser enhancement would be preferable. For instance, if the patient had 1 D of astigmatism at axis 180, and the implant was an AcrySof T5 sitting at 155 degrees, the program would inform you that rotation of the implant to the ideal position of 165 would result in an error of 0.77 D at 157 degrees. Therefore, it probably wouldn't be worth rotating the implant just for 0.23 D of effect. You're be better off doing a refractive procedure. The other benefit of laser is that the surgery will correct any spherical error, too.
There's also the decision between performing wavefront-guided treatment or conventional. The presence of the premium lens can negatively affect the accuracy of the aberrometry and result in false readings, and a conventional treatment might be better. For example, the wavefront may show a refractive error of -2.5 D in a patient who sees 20/25 or 20/30, which doesn't make much sense.
To quantify the problem, we analyzed 60 premium-IOL eyes who needed laser vision correction postop. We found that in 80 percent of the cases the wavefront information didn't add up, and we did a conventional treatment instead. The good news is that there wasn't a statistically significant difference between the custom and the conventional groups in terms of outcomes. As an aside, most of the 20 percent on whom custom was feasible in our study were Crystalens patients. Also, when planning the procedure and the patient has a Crystalens, we've found it's best to target one eye for some near vision.
Lenses such as the ReZoom and the Array, which use a refractive multifocal design, often yield nonsensical wavefronts, so they almost always dictate the use of a conventional treatment. We've been able to capture wavefronts on a few ReSTOR lenses, but were unsuccessful with a few others. So far, we've only had to enhance one Tecnis multifocal patient out of a few hundred implanted, and we're not sure if it's because the effective lens position of that lens is very good, we're better with biometry with that lens, or the fact that it's newer in our practice than the other lenses we use.
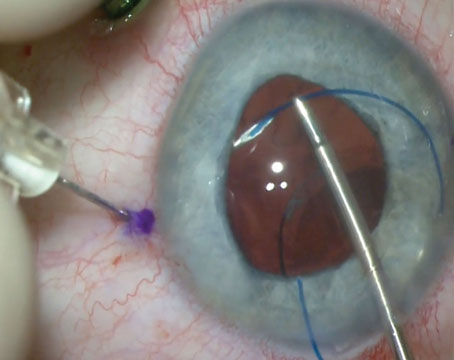
The techniques and approach to the surgery itself are the same as with any other case. If I'm going to use the IntraLase, however, I first measure the diameter available for a flap to make sure my femtosecond flap won't cross any of my previous incisions, which would result in a flap complication.
Though premium IOLs provide good near and distance vision to many, there will be some who'll need extra attention postop. I hope the advice I've shared here can address patients' complaints and allow them to enjoy life with their new vision.
Dr. Hardten is on the adjunct faculty in the department of ophthalmology at the University of Minnesota Medical School. His email is drhardten@mneye.com. Dr. Berdahl can be reached to get the latest toric IOL rotator at
johnberdahl@gmail.com.