|
J. Fernando Arevalo, MD, FACS |
Age-related cataract is the most common cause of reversible blindness worldwide, whereas the most common cause of irreversible legal blindness in this group of patients is age-related macular degeneration. Both cataract and AMD may contribute to visual disability in patients age 60 years or older. Recently, some studies have demonstrated that cataract surgery may improve vision in AMD patients in the short term.1,2 Other studies, however, suggest that cataract surgery may be a "risk factor" for exudative or neovascular AMD in the long term.2,3
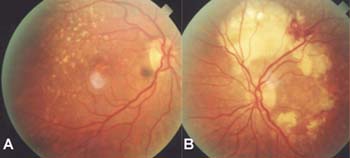
This article will discuss the evidence for and against an association between cataract surgery and the development of advanced AMD. (See Figure 1).
Epidemiological Studies
 |
| Figure 1. Phacoemulsification combined with foldable intraocular lens implantation. |
Various studies have suggested an association between cataract and the development of AMD. In the Beaver Dam Eye Study, nuclear sclerosis at baseline was associated with an increased incidence of early (soft drusen) but not late (choroidal neovascularization or geographic atrophy) AMD.4 The hypothesis proposed to explain this association states that both AMD and cataract may share one or more common risk factors including age, diet, light exposure and/or genetic factors. The association of AMD and nuclear sclerosis was also observed in the Chesapeake Bay Watermen Study,5 however the Framingham Eye Study6 and the Blue Mountains Eye Study7 did not find this association. While the reasons for such varying results are not clear, confounding factors or ascertainment biases related to life-long exposure histories could account for the differences.8
Pathophysiology and Clinical Studies
The major protective barrier to near-ultraviolet radiation (300 to 400 nm) is provided by the crystalline lens. It has been theorized that this "yellow filter" further protects the retina against blue light in the visible spectrum.9 Therefore, cataract may be protective against the development of AMD, and cataract removal may result in an increased risk of AMD. Other possible mechanisms proposed for this association include:
1) Post-surgical inflammation and the invasion of lymphocytes known to release angiogenic cytokines.10
2) Macular exposure and toxicity related to the operating microscope and light.11
3) Improved visualization and detection of AMD after cataract surgery.
4) An as-yet unidentified common risk factor or stimulus shared by both AMD and cataract.12
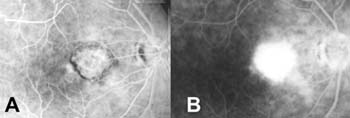
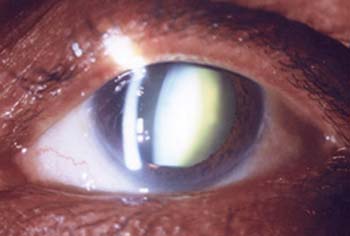
A retrospective/prospective study evaluated progression of AMD after unilateral extracapsular cataract extraction and intraocular lens implantation (ECCE + IOL) in bilateral, symmetric, early AMD patients.13 Wet AMD developed in 19 percent of eyes that underwent surgery compared to 4 percent of fellow unoperated eyes. Risk factors associated with wet AMD development were soft drusen, and male gender (See Figure 2). A 1998 prospective study reported on patients with bilateral early AMD who had undergone unilateral cataract surgery with a history of stable AMD and previous cataract surgery in the fellow eye: 27 percent of second operated eyes showed progression to wet AMD (See Figure 3). In addition, pseudophakic eyes with stable AMD for at least one year underwent YAG-laser posterior capsulotomy and developed wet AMD in 13 percent of eyes within 12 months compared to none of the fellow eyes. Soft drusen, systemic hypertension, and YAG-laser posterior capsulotomy were believed to be important risk factors (See Figure 4).14
Nevertheless, other authors have found significant improvement in both visual function, and quality of life in patients with AMD who underwent cataract surgery.2 One retrospective study designed to determine if there was functional and subjective benefit of cataract extraction in patients with AMD included 99 cases.1 The researchers found that 81 percent of cases had an improvement in best-corrected visual acuity, and 67 percent felt that the operation had been worthwhile. Another group reported a prospectively designed study of 187 patients with and without AMD who underwent cataract surgery; significant improvements both in terms of quality of life and visual function were achieved.15 The group observed no increased incidence of wet AMD. In addition, a 2002 report presented the Age-Related Eye Disease Study (AREDS) data and concluded that cataract surgery did not increase the risk of developing neovascular AMD. (Ferris FL, Chew EY. Recent new findings in age related macular degeneration (AMD) in the Age-Related Eye Disease Study (AREDS), part 2. The 35th Annual Retina Society Meeting. San Francisco, CA 2002.)
 |
| Figure 2A. Color fundus photograph showing high-risk soft drusen and pigmentary retinal pigment epithelium changes in the right eye. B. Disciform scarring in the left eye. Such patients may be at highest risk for the progression of AMD following cataract surgery. |
A recent presentation at the EURETINA Congress 2005 involved a randomized, multicenter prospective study of 320 patients with dry AMD and concluded that cataract surgery does not seem to influence the progression of the disease in its early course. (Binder S, Brunner S, Krebs Ilse, Stolba U, Falkner C. AMD and cataract surgery: The ECAM Study. Intermediate report. 5th EURETINA Congress 2005. Barcelona, Spain 2005.)
 |
| Figure 3. A patient with stable, dry maculopathy for at least six months who developed neovascular AMD four months following cataract surgery. Note the late hyperfluorescence with fluorescein angiography early (A) and late (B). |
Some studies, however, have suggested a role for cataract surgery in the development or progression of AMD. The findings to date from previous studies in the literature warrant clarification of the hypothesis that cataract surgery could increase the long-term risk for late-stage AMD. At the 1999 American Academy of Ophthalmology Annual Meeting in Orlando, Fla., a prospective study of progression was reported involving patients with bilateral dry AMD who underwent unilateral cataract surgery by phacoemulsification and foldable IOL (See Figure 5). Of 22 patients, 3 (14 percent) developed wet AMD compared to none of the fellow eyes. A group using three large population-based studies (the Salisbury Eye evaluation with 2,520 subjects between 65 and 84 years, the Proyecto VER with 4,774 Hispanic patients aged 40 and older, and the Baltimore Eye Survey with 4,396 subjects aged 40 and older) found modest evidence that cataract surgery may be associated with a greater prevalence of late-stage AMD.12 Such findings have prompted investigators to suggest that cataract extraction may be best considered in eyes in which the cataract has caused a decrease in function, and that close follow up of such eyes is indicated.2 Similarly, others have proposed ECCE plus IOL surgery in patients with moderate dry AMD only when their visual acuity is less than 20/200 based on their results showing that all patients who demonstrated aggravation of AMD after surgery were less than 20/200.16 (See Figure 6).
 |
| Figure 4. An aphakic patient after YAG-laser posterior capsulotomy, a possible risk factor for the development of neovascular AMD following cataract surgery. |
IOLs with Blue-light Protection
Exposure to ultraviolet light has been postulated as a cause of AMD, perhaps through damage to the retinal pigment epithelium. It seems logical, therefore, to replace the aging, yellowing lens with a blue light-absorbing yellow IOL in cataract surgery.18 However, there are conflicting reports in the literature regarding this issue. It has been difficult to prove the role of light exposure in AMD epidemiologically because it is hard to determine an individual's cumulative light exposure retrospectively.17 In fact, cumulative ultraviolet exposure has been found to be only weakly associated with AMD in epidemiological studies.8 Although the AcrySof Natural IOL (Alcon Labs) decreases acute retinal phototoxic damage from intense violet light in cell culture and experimental animals, much longer-term, lower light-level experiments will be needed to establish the relevance of these studies to the human aging retina.19 Based on different published studies,4,5,8,19 we have graded in order of importance the epidemiological risk factors of AMD and we could categorize them as follows:
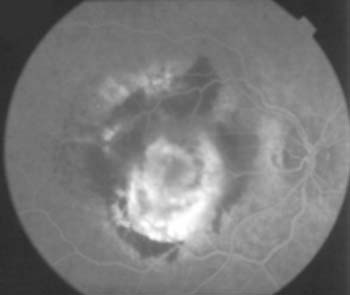
Figure 5. A patient with bilateral dry AMD who underwent unilateral cataract surgery in the right eye by phacoemulsification plus foldable IOL, who developed neovascular AMD after surgery. Note the active hemorrhage within the lesion and leakage in the fluorescein angiogram.
• Category 1 (definitive proof): age and smoking;
• Category 2 (controversial results): race, systemic hypertension, cardiovascular disease, low serum omega-3, high intake of saturated fats and cholesterol, and hereditary factors;
• Category 3 (no conclusive evidence): sunlight exposure and alcohol use.
Some have suggested that blue light is needed for optimal vision.19 In theory, the Acrysof Natural IOL decreases the risk of acute UV-phototoxicity but psychophysical studies have found that filtering blue in addition to violet light can reduce scotopic sensitivity, a natural function which declines with aging and is even worse in people with AMD.19 Yellow IOLs have been reported to provide 50-percent less ultraviolet protection than sunglasses, prompting some to recommend that Acrysof Natural IOL users should wear sunglasses in bright environments, and that the optimal IOL should transmit as much blue light as possible to ensure good VA.19 Moreover, light exposure may play a role in the development of AMD in some people, but little or no role in others.
 |
| Figure 6. A patient with a cataract and a visual acuity of less than 20/200. |
The issue of whether cataract surgery is a risk factor for the development or progression of AMD remains controversial, with some studies supporting and other studies refuting an association. While both subjective and objective visual function improvement can clearly be achieved after cataract surgery in most eyes with AMD, the possibility that AMD might develop or progress in some eyes would seem to suggest that cataract surgery in patients with AMD should be reserved for those patients who stand to gain the most by the removal of their cataract.
|
This article was supported in part by the Arevalo-Coutinho Foundation for Research in Ophthalmology (FACO), Caracas, Venezuela. The authors practice in the Retina and Vitreous Service, Clinica Oftalmológica Centro Caracas, and the Arevalo-Coutinho Foundation for Research in Ophthalmology, Caracas. They have no proprietary or financial interest in any products or techniques described in this article.
Contact Dr. Arevalo at Clinica Oftalmologica Centro Caracas, Edif. Centro Caracas PH-1, Av. Panteon. San Bernardino, Caracas 1010, Venezuela. Phone: (58-212) 576-8687. Fax: (58-212) 576-8815. E-mail: areval1@telcel.net.ve.
1. Shuttleworth GN, Luhishi EA, Harrad RA. Do patients with age related maculopathy and cataract benefit from cataract surgery? Br J Ophthalmol 1998;82:611-6.
2. Armbrecht AM, Findlay C, Aspinall PA, Hill AR, Dhillon B. Cataract surgery in patients with age-related macular degeneration: one-year outcomes. J Cataract Refract Surg 2003;29:686-93.
3. Wang JJ, Klein R, Smith W, Klein BE, Tomany S, Mitchell P. Cataract surgery and the 5-year incidence of late-stage age-related maculopathy: pooled findings from the Beaver Dam and Blue Mountains eye studies. Ophthalmology 2003;110:1960-7.
4. Klein R, Klein BE, Wong TY, Tomany SC, Cruickshanks KJ. The association of cataract and cataract surgery with the long-term incidence of age-related maculopathy: the Beaver Dam eye study. Arch Ophthalmol 2002;120:1551-8.
5. West SK, Rosenthal FS, Bressler NM, Bressler SB, Munoz B, Fine SL, Taylor HR. Exposure to sunlight and other risk factors for age-related macular degeneration. Arch Ophthalmol 1989;107:875-9.
6. Sperduto RD, Hiller R, Seigel D. Lens opacities and senile maculopathy. Arch Ophthalmol 1981;99:1004-8.
7. Wang JJ, Mitchell PG, Cumming RG, Lim R. Cataract and age-related maculopathy: the Blue Mountains Eye Study. Ophthalmic Epidemiol 1999;6:317-26.
8. Klein R, Peto T, Bird A, Vannewkirk MR. The epidemiology of age-related macular degeneration. Am J Ophthalmol 2004;137:486-95.
9. Smith BT, Belani S, Ho AC. Light energy, cataract surgery, and progression of age-related macular degeneration. Curr Opin Ophthalmol 2005;16:166-9.
10. van der Schaft TL, Mooy CM, de Bruijn WC, Mulder PG, Pameyer JH, de Jong PT. Increased prevalence of disciform macular degeneration after cataract extraction with implantation of an intraocular lens. Br J Ophthalmol 1994;78:441-5.
11. Libre PE. Intraoperative light toxicity: a possible explanation for the association between cataract surgery and age-related macular degeneration. Am J Ophthalmol 2003;136:961.
12. Freeman EE, Munoz B, West SK, Tielsch JM, Schein OD. Is there an association between cataract surgery and age-related macular degeneration? Data from three population-based studies. Am J Ophthalmol 2003;135:849-56.
13. Pollack A, Marcovich A, Bukelman A, Oliver M. Age-related macular degeneration after extracapsular cataract extraction with intraocular lens implantation. Ophthalmology 1996;103:1546-54.
14. Pollack A, Bukelman A, Zalish M, Leiba H, Oliver M. The course of age-related macular degeneration following bilateral cataract surgery. Ophthalmic Surg Lasers 1998;29:286-94.
15. Armbrecht AM, Findlay C, Kaushal S, Aspinall P, Hill AR, Dhillon B. Is cataract surgery justified in patients with age related macular degeneration? A visual function and quality of life assessment. Br J Ophthalmol 2000;84:1343-8.
16. Hawkins WR. AMD after ECCE with IOL implant. Ophthalmology 1997;104:900.
17. Nilsson SE. Are there advantages in implanting a yellow IOL to reduce the risk of AMD? Acta Ophthalmol Scand 2004;82:123-5.
18. Mainster MA. Intraocular lenses should block UV radiation and violet but not blue light. Arch Ophthalmol 2005;123:550-5.



