Though it's impossible for one device to be all things to all surgeons, femtosecond lasers are doing their level best to be just that. Originally used as alternatives to microkeratomes for making LASIK flaps, these Swiss Army lasers can now cut oval flaps, vary the shape of side cuts, perform cuts for keratoplasty procedures and create intrastromal refractive changes. Here's a look at the latest developments with the femtosecond lasers that are approved for use in the
AMO IntraLase FS-150
In terms of enhancements to the FS-150, Perry Binder, MD, medical director for Abbott Medical Optics, says there are three main features that help set it apart. "The first is speed," he says. "By running at 150 kHz, it allows the user to place the laser ablations closer together individually and row by row. This makes for easier flap lifts, smoother surfaces and overall faster procedures. So, for example, if you chose to use a spot/line separation of 8 µm and want a 9-mm diameter flap, you can complete that flap in 10 seconds, as opposed to about 21 seconds or so with the [previous] 60-kHz laser.
Increased speed also decreases the risk of such things as suction loss and decentration.
This is important not only for LASIK but also for the corneal transplant procedure known as IntraLase-enabled keratoplasty. These transplants take a lot longer and a lot of bad things can happen the longer you're ablating a cornea. By increasing the speed, you decrease the chances of having an error when creating the donor cornea."
The next feature is the creation of oval-shaped flaps. "The FS-150 can create up to a 12-percent oval in the vertical meridian, in which the vertical is going to be shorter than the horizontal," Dr. Binder explains. "That allows the surgeon to push the hinge away from the ablation, which avoids ablating it by accident. In the past, to avoid ablating the hinge, users have either decentered their flap or they switched to a temporal hinge. The latter can be done easily with a femtosecond laser by way of software, but is more difficult to do with a mechanical microkeratome. The advantage of pushing the hinge to the side with an oval flap is that you don't have to go through these machinations, and you can still use a temporal hinge if you want. The other advantage is that you're cutting fewer peripheral lamellae because you're cutting fewer vertically than horizontally, and that may not weaken the structure of the cornea as much as if the greater number were cut. Oval flaps are mainly used for hyperopic ablations."
The IntraLase system also allows surgeons to vary the angle of the flap's side cut to a greater degree than with previous generation lasers. The side cut is the final ablation that allows the flap to be lifted from the bed. "With the previous generation lasers you could cut as shallow as 30 degrees and as steep as 90 degrees," explains Dr. Binder. "Now, you can go an additional 60 degrees, from 90 to 150. This helps the flap to seat a lot more easily, the wound to heal faster and the surgeon to use less energy in creating that side cut. The theory, which we have yet to prove, is by having that inverted side cut you cut fewer corneal nerves because in that anterior lip from 90 to 150 there are nerves that you're not severing. That could lead to improved sensation and, we hope, decreased dry eye. The disadvantage of having an inverted side cut is that it takes longer to create the flap. Also, having an inverted side cut decreases the diameter that the excimer laser has to work with, because now the tissue is coming inward in the anterior part of the bed. For instance, if you have a base of 9 mm and you have a 150-degree side cut, the anterior part of that bed is about 8.4 mm. So, what most users are doing is going in between: They're going for about a 120-degree side cut, which gives all the advantages of an inverted cut but doesn't decrease the diameter as much."
AMO is also planning to release two software modules for the IntraLase in 2010, one of which will allow users to create intrastromal pockets and another that will enable the device to perform a presbyopic treatment.
Dr. Binder can't reveal much about these new add-ons, other than to say that he'll be presenting preliminary data from the new modules at this year's meeting of the American Society of Cataract and Refractive Surgery.
Technolas Perfect Vision 520 FS
The first major change with this laser is that the device's maker, 20/10 Perfect Vision, entered into a joint venture with Bausch & Lomb in April of 2009, forming Technolas Perfect Vision. The name of the laser was also changed from the Femtec to the 520 FS. Though the device is currently approved in the
The company plans to roll it out here in February or March of this year.
There have been developments other than the name change, however.
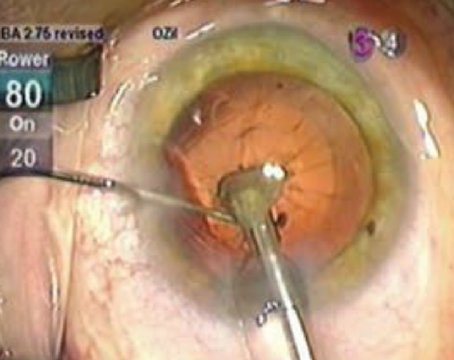
The device's new feature that's probably garnered the most attention is the ability to perform the intrastromal Intracor refractive procedure. In the Intracor treatment for emmetropic or slightly hyperopic presbyopia, the device creates a series of rings, starting in the posterior stroma, coming forward through mid-stroma and stopping in the anterior cornea. This serves to steepen the anterior corneal surface and generate a multifocal hyperprolate shape. To treat low myopia or astigmatism, the device adds radial intrastromal ablations, though the effect of such treatments is currently limited.
According to the surgery's pioneer, Luis Ruiz, MD, of
In a study of 245 Intracor procedures performed by Dr. Ruiz, 184 reached one-year follow-up. At one year, the average distance acuity was 20/20, and the average near vision was just below J1. Distance-corrected near vision was J1. In the group available for one-year follow-up, 97.8 percent see both 20/25 or better and J3 or better.
In a published report on Intracor, all of the patients reported halos after surgery, especially in dark conditions, but many didn't have trouble driving at night because of them; also, near vision was reduced somewhat in dim light due to the dilated pupil detracting from the benefit of the hyper-prolate cornea.1 The procedure hasn't yet been submitted for U.S. Food and Drug Administration approval, though it has received the CE Mark in Europe for low presbyopic treatments ranging from +0.25 to +0.75 D with 0.5 D of cylinder. Lindsay Brooks, PhD, the company's manager of medical communications, says Technolas Perfect Vision will apply for an investigational device exemption for Intracor from the FDA this year, and, if everything goes according to plan, approval could arrive in five years.
"The other new application that was released as a software modification is a procedure for crosslinking," explains Michael Behrend, a senior specialist in applications and global product support for Technolas Perfect Vision. "With it, the device makes an intrastromal bed for the riboflavin before the surgeon exposes the eye to the UV light. This speeds up the crosslinking procedure by at least 20 minutes."
The system has also added computer-controlled centration. "Basically, you dock the patient and then the software allows you to adjust the centration of the device in 50-µm steps to a maximum radius of 400 µm," says Mr. Behrend. The device also has a curved corneal interface, rather than a planar applanation plate. Mr. Behrend says this curved interface allows the cornea to maintain a natural curvature, and is one of the aspects of the technology that actually makes Intracor possible. The laser also uses a spiral ablation pattern rather than a raster scanning pattern. "Basically, we use that because we have a curved patient interface," says Mr. Behrend. "The result is that, for flaps and keratoplasty, we get no central opaque bubble layer. Instead, we get an occasional OBL in the peripheral area, but that doesn't usually affect the lifting of the flap." Mr. Behrend says the device has a lot of potential, and surgeons should stay tuned for new procedures to become available. "There's some exciting stuff coming," he says.
Zeiss Visumax
The Visumax is another speedy femtosecond laser that's being used for things other than making flaps.
"Originally, the Visumax was 200 kHz, now the speed is 500 kHz," says
The Visumax also touts a curved patient interface that Zeiss says requires less suction to keep on the eye. "The lower suction pressure means the patient can see the fixation light throughout the procedure without any blackout of vision from suction," says Dr. Dishler.
"It also makes the procedure more comfortable for the patient." He says the curved contact glass also helps tailor a cut to the patient's eye. "Some lasers in which a disposable cone is placed on the eye assume that each cone is of the same dimension as the others, and that the bottom is the zero point," says Dr. Dishler. "However, there's variability in how the cones are manufactured. With the Visumax, each time you situate the disposable curved contact glass, the laser uses a proprietary method to scan the glass, map it and determine exactly where on that disposable glass the zero point is. The laser computer will reject any glass that has an imperfection, such as a manufacturing glitch."
The laser can also create side cuts that are beveled in, similar to the inverted side cuts of the IntraLase. "So, the flap is larger in the deeper part and slightly smaller near the surface," explains Dr. Dishler. "This allows the flaps to kind of tuck in at the edge of the bed, making them more secure."
In
The surgeon then lifts the flap and removes the lenticule. The removal of the tissue is what causes the refractive change when the flap is put back into place. "It's similar to the old automated lamellar keratoplasty procedure," says Dr. Dishler. "However, it's more sophisticated. It's just as accurate with a -12 D procedure as it is with a -2 D, while, with an excimer, the accuracy tends to not be as good in the higher ranges."
Rupal Shah, MD, of
The next evolution of the FLEx is the small-incision lenticule extraction (SMILE) procedure, in which a small, 2-mm incision is created and the lenticule is pulled out through that. "It's kind of like the difference between extracapsular cataract extraction and phaco," says Dr. Dishler. "The benefit of SMILE is that you can use the femtosecond laser to cut the lens shape and remove it through a small incision without incurring any issues with dry eye, cutting corneal nerves, inducing weakening through ectasia and the like." Neither procedure has been submitted for approval by the FDA.
However, the company has submitted data for approval of penetrating and lamellar keratoplasty. "Being able to perform lamellar keratoplasty would be a big step forward," says Dr. Dishler.
Ziemer Femto LDV
The Femto LDV still holds the distinction of being the fastest femtosecond laser approved in the
The Ziemer has several design features that make it different. First, the laser optics are in a handpiece that sits at the end of an articulated arm that can be swung in and out of the operative field. In that sense, it's designed to work in a way similar to a microkeratome, in that the handpiece fits beneath the excimer, which allows the surgeon to create the flap and then swing the handpiece out of the way so the ablation can be performed. Second, the laser also sits on lockable wheels that allow it to be moved around an office. Finally, to determine the thickness of the flap that will be cut, the surgeon must insert a spacing device called an intershield. Currently, there are intershields for 140-, 110-, 100- and 90-µm flaps.
Phillips Kirk Labor, MD, of Grapevine, Texas, was the first U.S. solo private practitioner to own a Femto LDV and says he's gotten comfortable with it over the years since its approval. "From my perspective as a surgeon, one of the big things Ziemer did was put an aiming and centration circle within the handpiece," says Dr. Labor. "That's really helped in terms of centration and making sure the flaps are where they need to be."
The company plans to add the ability to create intracorneal pockets for corneal inlays and intracorneal channels for the placement of corneal ring segments. Both functions are currently in testing.
"We have software available that can cut any kind of pattern," says Dr. Wirthlin. "When you create a flap, you cut around the cornea and make a hinge. Creating a pocket in the cornea is similar, but instead of a hinge you cut a small exit incision and it remains closed, kind of like a flap that you don't open. The Femto LDV is currently being used by the Accufocus company in the clinical trials of its corneal inlay. "For channels, you can create an incision that's exactly the shape and size of the particular device you want to insert," Dr. Wirthlin continues. "We usually make two separate incisions for the two segments." The creation of channels, however, requires the use of a different laser handpiece that enables cutting at depths greater than 250 µm, which is the limit of the standard handpiece.
"The other procedure we're working on is lamellar keratoplasty," reveals Dr. Wirthlin. "This could be done at any depth down to 450 to 500 µm, allowing surgeons to do lamellar procedures in the upper cornea as well as procedures close to Descemet's membrane. It's possible that the lamellar procedure software will be released sometime in 2010." 1
1. Ruiz LA, Cepeda LM, Fuentes VC. Intrastromal correction of presbyopia using a femtosecond laser system. J Refract Surg 2009;25:847-54.