A surgeon's choice of phaco tip design is largely based on comfort and selection of the right tip for the job, such as hard cataract vs. soft nucleus, etc. While fluidics ranks higher when surgeons list their top concerns in phacoemulsification, the impact of tip design on a successful phaco procedure cannot be overlooked. This article reviews how form follows function in tip design and looks ahead to the demands placed on tips as bimanual phaco and refractive lens removal grow in practice.
Why Tips Matter
Tip design is extremely important for two reasons, says Richard Mackool, MD, of Astoria, N.Y. The first reason he lists is dealing with dense nuclei, the second is maximizing the benefit of fluidics. He says that simple principles of physics show us that use of a relatively pointed tip, as opposed to a blunt tip, will provide more force at the tip and better attack a dense nucleus. "Highly beveled tips should be used sideways. Whenever the surgeon wants to im-pale, then the plane of the port will be parallel to the plane of the nucleus, making it very easy to occlude, impale, et cetera," he says.
Concerning fluidics, Dr. Mackool notes that a good phaco tip will be efficient in both removing the nucleus and permitting infusion. By using a tip designed with great infusion capacity and mating it with software and a phaco console that recognize changes in vacuum levels and adjust flow rate accordingly, Dr. Mackool says that he can use flow rates and vacuum levels that are "absolutely unprecedented in our profession."
As an example, he describes how he can use a flow rate up to 100 cc per minute and a vacuum level up to 700 mmHg using Alcon's Infinity Vision System and a 1.1 flare tip. "These numbers are approximately double what many surgeons consider to be their maximum." Dr. Mackool calls this procedure's efficiency "high" in terms of time—getting done quickly—and "minimal" in terms of ultrasound use. "This combination of tip and console gets you a lot more miles per gallon with your ultrasound because you are removing the tissue with flow rate and vacuum and not a lot of ultrasound." It's safe, too, he says, since the high rate of vacuum keeps the nuclear particles close to the tip and "they don't go chattering off. It's generally the movement of nuclear pieces against the endothelium and working too close to the endothelium that cause endothelial cell loss," he says.
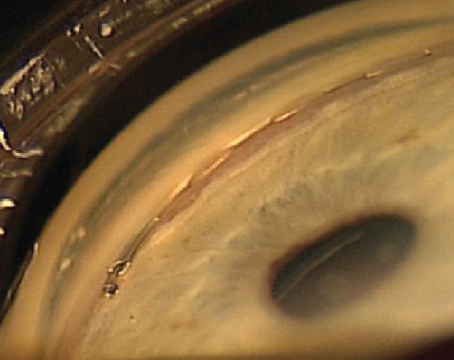
 |
| Tip modifications for both flow and power are demonstrated in Alcon Laboratories' flared ABS tip. The result is increased control and more power. |
Variations Meet Surgeons' Needs
Variations in tip design meet surgeons' procedural needs for size, angulation, power delivery and flow. "Diameter of the tip has traditionally been around 19 gauge, but as we go to smaller incisions, we're seeing 20- or 21-ga. tips," says Tucson's William J. Fishkind, MD, FACS. "The tip choice impacts the procedure here because, by virtue of the de-creased diameter, the phaco procedure slows down a bit. You can't take as large a piece of material at any one time, but that's the compromise a surgeon makes if he wants to use smaller incisions."
Choice of tip angulation (30 degree, zero degree) is related to the phaco technique and to what the physician likes in delivery of energy within the anterior segment, explains Dr. Fishkind. For divide and conquer phaco, he prefers a bevel-down sculpting technique, and finds that a 30-degree tip works nicely. His preferred phaco technique is phaco chop either horizontally or vertically dependent upon the maturity of the nucleus. For this, his preferred tip choice is a zero-degree, 20-ga. tip. "The zero-degree phaco tip puts the energy directly in front of the tip. I just line everything up ahead of the tip and it's quicker and easier for me," he explains.
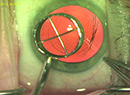
 |
| Using the phaco tip model he designed with Alcon Laboratories, Richard Mackool, MD, can use high flow and vacuum levels with low risk of incision burn. |
Consideration of the degree of cataract also may be a factor in phaco tip choice, acknowledges Dr. Fishkind. "Many surgeons will say that if the cataract is very hard, they will use a 45-degree tip. If it's softer, they'll use a 30 or a zero. But others will always use a specific-degree tip and modify the procedure for the tip. For example, a surgeon may want to use a 30-degree tip all the time. He likes to do a chop, and so he just turns the tip bevel down to get into the nucleus for the chop, and then once the fragments come, he'll turn it sideways toward the fragment. Hard cataract or soft, he'll do the same thing." He emphasizes, "It comes down to surgeon comfort."
The design of the phaco tip can change the procedure in one additional way: modification for power and/or flow. Power modification is another outcome of changing the tip angulation, as discussed above. Flow modification generally involves the sleeve. Thinking about flow modification, Dr. Fishkind points to tips with ribbed sleeves: "The ribbed sleeves don't get compressed around the needle and that's a flow modification, because that lack of compression changes the inflow and allows a tighter incision." Another flow modification occurs with the design of the ABS tip from Alcon, offers Dr. Fishkind. "The ABS tip is a standard phaco tip with a 0.175-mm hole drilled in the shaft. When that tip occludes with a piece of material on it, the flow continues through the hole in the shaft. So it never creates extreme elevations in the vacuum; that's equivalent to a flow modification," he says.
Dr. Fishkind adds that some tips are modified for both flow and power. These tips have narrow shanks and flare out at the tip. The widened tip creates power closer to the tip and acts as a power amplifier. The narrow shank creates a restriction to flow, rendering the chamber more stable. "There is increased control and more power with these tips, like the Alcon ABS flare tip," describes Dr. Fishkind.
Tips for Microphaco
Salt Lake City's Randall Olson, MD, prefers a bimanual, or microphaco, technique and agrees that the best tips for this job are indeed different from those used in traditional coaxial phacoemulsification. "The main difference in microphaco tip design is that you've got a wound that you want to have relatively tight around your phaco needle. Therefore, the profile of your needle has to be fairly consistent," he explains. For this reason, he believes that some tips, flare tips, for example, don't work in microphaco, since they produce a significantly larger outside opening.
As a manufacturer, Mr. Laks says that MicroSurgical Technology's objective is to design tips appropriately for a given incision size. "We design everything to work together. So if a surgeon wants to do a 1.2-mm incision, our phaco tip and knife are sized properly (20 ga.) for that," he explains.
Dr. Olson has abandoned the zero-degree tip as he's moved to microphaco. "If you have a moderately tight wound, you can't get a zero-degree tip started," he says. "It's near to impossible to get the type of tight wound I think I should have working with a zero-degree tip." Dr. Olson believes that a 30-degree tip is the minimum needed to easily get into a microphaco incision, but again bows to user preference.
"Bimanual phaco changes the fluid flow relationships in the anterior segment, by virtue of the unsleeved tip and the change in diameter," says Dr. Fishkind. He says that the critical issue in bimanual phaco is heat. "There's a lot of debate about which tips and machines generate little or no heat; a factor upon which a surgeon may make his choice of tip for microphaco."
Mr. Laks finds a significant opportunity to design tips specifically for bi-manual phaco. "You need to develop them on their own and not just adapt what the coaxial tip does," he maintains. In addition to cooling issues, which Mr. Laks notes are addressed by some of the advanced phaco machines themselves, he points out that surgeons have functional needs unique to microphaco, related to tips, irrigating choppers and knives. He mentions that some surgeons have been using tools designed for vitreoretinal surgery or laser phaco, bringing them over to microphaco and finding they're not op-timal. "They're not the right tools for the job, because they were designed for something else," he says.
Soft-lens Removal
Dr. Olson calls microphaco "tailor-made" for refractive lens exchange. He says that, with a soft lens, sometimes all you need to free the particles are the ir-rigation instruments. "The irrigation will move all the material up off the capsule and you never need to approach it with the ultrasound tip," in-creasing the safety of the procedure. He says that is an advantage over coaxial phaco, where he's seen surgeons working very near the capsule. "It's going to be near to impossible to break the capsule with microphaco in refractive lens exchange." He believes the new tips being designed for microphaco will set a new standard for capsular breakage rate: Fewer than one in 1,000.
Dr. Mackool, an adherent to coaxial phaco, predicts that, in five years, surgeons will remove more lenses for re-fractive purposes than for cataracts. He sees phaco tip design following that market. "We'll probably need ultrasound less and less because the lenses will be relatively soft. A technology such as AquaLase (developed by Alcon) will become more popular for lens removal." He says refractive lens exchange will have soaring success rates because patients can get good vision at both distance and near and have no further significant refractive changes for the rest of their lives.



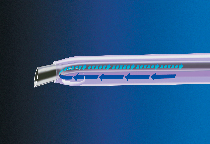
MicroSurgical Technology designs unique tips for bimanual phaco as well as new generations of coaxial phaco tips.
Where Tips Stand
All that being said, neither Dr. Mackool nor Dr. Olson says that tip design can make or break a phaco procedure. "I don't find the new designs in tips particularly important for my technique," says Dr. Olson. "But other techniques with different approaches may benefit." Dr. Fishkind agrees: "Tip design makes small modifications in the way phaco is done, but they are far less important than the advancements in the phaco machines and resulting fluidics that have changed the procedure dramatically over the years."
MicroSurgical Technology's Mr. Laks sees the tip as enhancing the overall effectiveness of the phaco system. He says issues remain for which phaco-tip designers are seeking solutions. "Phaco tips can be designed with elements to help control post-occlusion-break surge," he says. To answer surgeons' procedural needs, he says MicroSurgical Technology is developing tip designs with attributes that can be used for a variety of phaco techniques (chop procedures or divide and conquer) as well as unique tips for bimanual phaco, or are better used with one than the other. "Again," he summarizes, "our philosophy is to provide the right tool for the job, for the surgeon and the particular phaco machine."
Dr. Fishkind is co-director of the Fishkind & Bakewell Eye Care & Surgery Center and a clinical professor of ophthalmology at the University of Utah in Salt Lake City. He may be reached at (520) 293-6740 or wfishkind@earthlink.net.
Dr. Mackool is director of the Mackool Eye Institute and Laser Center and senior attending surgeon at the New York Eye and Ear Infirmary. He may be reached at (718) 728-3400 or mackool@worldnet.att.net.
Dr. Olson is director of the John A. Moran Eye Center and chairman at the University of Utah Department of Ophthalmology and Visual Sciences. He may be reached at (801) 585-6622 or randall.olson@hsc.utah.edu.
All interviewees have served as consultants for companies mentioned in this article and have developed products for these companies and others.
Mr. Laks of MicroSurgical Technology may be reached at (425) 861-4002 or llaks@microsurgical.com.