To the Editor:
I enjoyed reading the article, “The IOL in the Sulcus, When, Why & How,” (July 2018) on sulcus placement of IOLs, and I’d like to contribute my take on this.
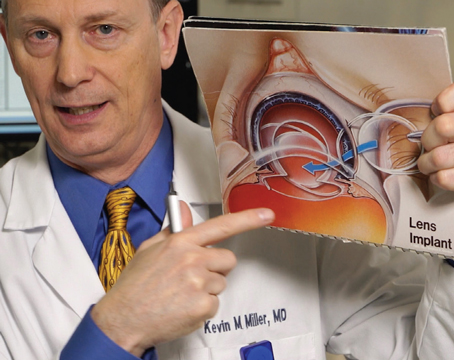
Sulcus placement is usually necessitated due to zonular instability or a capsular break, and I agree that a three-piece lens is mandatory when a sulcus placement is being contemplated. These lenses are 13 mm in length with a 10-degree forward angulation of the haptics.
In the early days of intraocular lenses, before in-the-bag implantation was emphasized, these lenses were widely used in routine cases, and were incredibly versatile, since they could be placed in the bag, in the sulcus, or at times (inadvertently) with one haptic in the bag and the other in the sulcus, all with reasonably good results.
In my experience, if I have a central posterior capsular break with an intact anterior capsular bag and an intact peripheral posterior capsular bag, I’m often able to place the Alcon MA30AC three-piece lens in the bag, rather than resorting to a sulcus-placement-with-optic-capture approach.
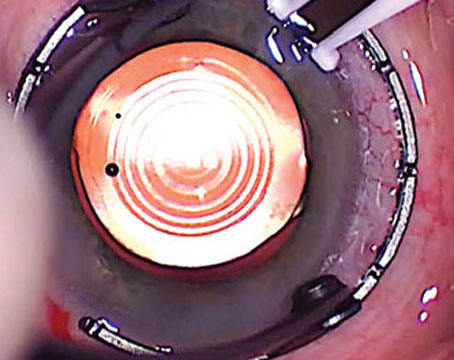
To implant the lens in this manner, I first place Provisc (sodium hyaluronate) to deepen the anterior chamber and bag and push back the intact or broken vitreous face. A Kuglen hook is useful for retracting the iris to make sure the peripheral posterior bag is intact 360 degrees or close to it. (If the posterior capsular bag is intact in some areas but absent in others, then caution should be the order of the day: Sulcus implantation is indicated.) After confirming the intact bag, I’ll open the wound to 6 mm, preserving the same wound architecture that was used to make the initial 2.7-mm incision. I am averse to folding the lens in this scenario; I would rather make a larger incision and place the three-piece lens unfolded. This does add time to the case, and several sutures are needed to close the incision at the conclusion of the case.
The leading haptic then glides in underneath the anterior capsular flap, if possible, with the superior haptic rotated clockwise (as close to its junction with the optic as possible) with a Sinskey or Lester Hook, in order to “pop” the trailing haptic in.
Alternatively, a McPherson or microsurgical forceps (MST Techology) can be used to grab the haptic and bend it inferiorly and then release it underneath the capsular flap edge. Even with an open central posterior capsule, these maneuvers can be done without extending the capsular tear or causing the vitreous to move forward.
If the IOL can’t be placed directly in the bag, but lands instead in the anterior chamber, one can manipulate it intracamerally to obtain in-the-bag positioning of both haptics. This is more apt to occur if the corneal incision is tight (slightly less than 6 mm), or if you choose to introduce the lens folded into the chamber.
If you attempt this in-the-bag placement but see a downward drift in the lens towards the vitreous, this means that you are anterior to the bag and that the peripheral posterior capsule-zonular complex where the haptic is being placed is not intact. Through your limbal incision, pop the optic in front of the anterior capsule and position the IOL haptics in the sulcus where the posterior capsular zonular complex is still intact (it must be intact both where the first haptic is being placed and 180 degrees away).
Keep in mind that the optic will generally remain well-centered if both haptics are properly positioned, even if you are unable to capture the optic behind the anterior capsular bag.
Wherever you decide to position the intraocular lens, be mindful of the effective lens position and adjust your lens power accordingly.
Lawrence Stone, MD
Chicago