As you know, despite the many advances we’ve seen in refractive surgery, some postop patients with seemingly good or even perfect outcomes return to us in an unhappy state. Various factors—such as personalities, optics, ocular surface and not-so-obvious issues—can lead to these complaints. Using a retrospective case analysis of eight dissatisfied patients, we’d like to help you meet the high expectations of patients in your practice. By identifying what we call, “biomarkers of happiness” and responding to them properly before surgery, you can transform “20/20 unhappy” to 20/20 happy.
What Causes Unhappiness?
We’ve often wondered what drives unhappiness in some of our patients, even those who no longer need to wear glasses after surgery. The evidence of discontent can be found in the many lawsuits filed against surgeons. Although we usually prevail in court, settlements reached before sympathetic juries can be costly.1
How can we avoid this? One way is to look more closely during preop workups for those biomarkers of happiness, which requires us to understand the role of each aspect of refractive surgery, including the ocular surface and tears, meibomian glands, corneal surface, optics, epithelium, pupils, posterior segment, systemic factors and—the clinically unmeasurable biomarker—patient personality. Let’s review each of the cases that we’ve selected.
Patient #1: A Case of Tears
A 25-year-old female post-femtosecond LASIK patient came to us complaining of glare. Her corneal topography revealed a central island around a relatively flat area in her right eye, an “irregular’ finding reported by her previous physician. In collaboration with the physician, our plan was to fit her in scleral RGP lenses and, if they worked, replicate their effect with topography-guided surface enhancement.
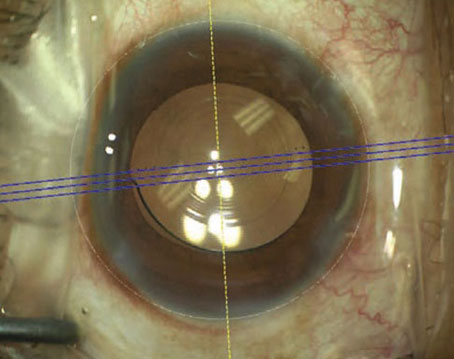
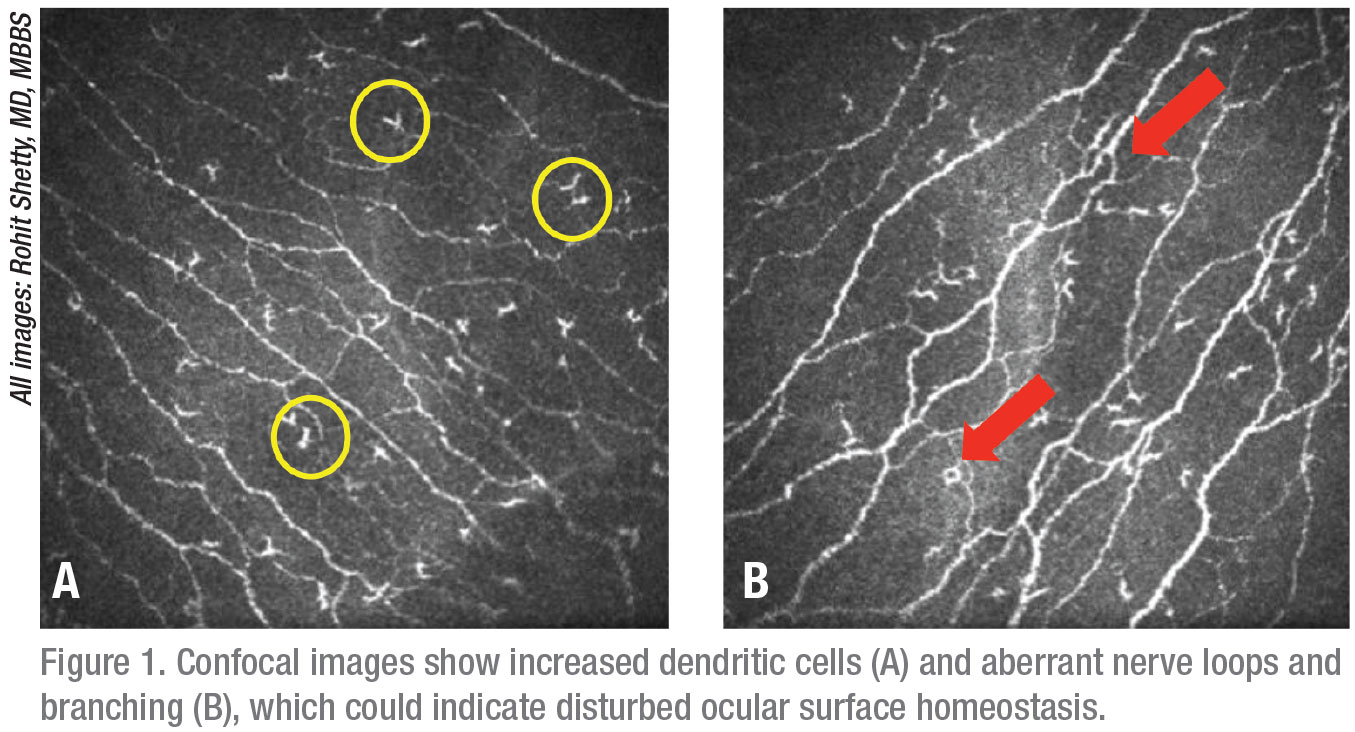
However, the RGP lenses only made the patient’s signs and symptoms worse. We determined that she had a normal pupil size and aberration profile. Then, after questioning her closely, we learned that she actually had a history of severe preop contact lens intolerance. During an ocular evaluation, we found that she had a low tear-film breakup time (three seconds OD, four seconds OS) and a high ocular disease index (24 points and 50 percent on the scale, indicating a severe degree of ocular surface symptoms). Findings from an Optical Quality Analysis System evaluation (Visiometrics, Costa Mesa, California) correlated with symptoms of dry eye.2 Confocal laser scanning microscopy revealed dendritic corneal cells and aberrant, branching nerve loops, confirming disturbed ocular surface homeostasis.3 (See Figure 1.) These results, combined with ocular surface fluorescein staining and her history, pointed to dysfunctional tear syndrome, leading to fluctuating vision and light scattering the patient had described as glare.4
We treated her with lubricants and meibomian gland massage, as well as steroids and cyclosporine drops for ocular surface inflammation. A week later, the patient responded favorably. She was relieved that she wouldn’t need to wear contact lenses or undergo an enhancement. We provided regular follow-up care, including a repeat topography, and she maintained stability. OSDI scores decreased. She’s now a much happier 20/20 patient.
The key to success was to listen more closely—specifically to her description of past contact lens intolerance. Of course, this should have occurred before her surgery. Ocular surface disease needs to be confirmed and treated both before and after surgery. We concluded that the patient would have fared better if she had undergone SMILE, a potentially nerve-sparing surgery, especially in view of her history of contact lens intolerance.
Biomarker of happiness: Listen to your patient more closely before choosing a mode of refractive surgery.
 |
Patient #2: Microdistortions
A 27-year-old male SMILE patient, four weeks postop, OU, was unhappy with the quality of his vision despite a 20/20 outcome. We don’t expect an acute visual recovery one day after SMILE, so we didn’t evaluate the patient until he returned for his four-week postop visit with unclear vision, despite an expected full qualitative visual recovery.
The patient had normal topography findings and no signs or symptoms of dry eye. Microdistortions in his Bowman’s layer, which would have been expected soon after surgery, were still evident. Althought difficult to visualize with a slit lamp, the microdistortions were clearly visible when we used anterior segment OCT.
We concluded that intraoperative recognition of striae and subsequent cap repositioning could have increased the chances of improving this patient’s outcome significantly, likely avoiding his blurred vision.
Instead, he needed to wait longer for recovery to occur at the microstructural and cellular levels. We now recommend repositioning the cap and anterior surface of the cornea during SMILE surgery in cases when this approach is prudent.
Although refractive error before surgery determines the extent of microdistortions, intraoperative cap repositioning can reduce them, expediting acute visual recovery after SMILE.5 The cap is repositioned by stroking the anterior surface of the cornea with a spatula in a superior to inferior direction with mild to moderate pressure over the cap area.
Biomarker of happiness: Consider the use of intraoperative cap repositioning to reduce microdistortions in SMILE surgery.
Patient #3: Mesopic Pupil
Two years after undergoing femtosecond LASIK, OU, a 23-year-old male presented with 20/20 vision (-025 -0.75 x 140 degrees), with normal topography maps. However, he was complaining of glare. Our examination revealed normal corneal optics and a normal ocular surface. We noticed, though, that he also had a mesopic pupil—measuring 6.58 mm—that appeared to be a possible cause of distortion and higher-order aberrations. These symptoms can increase proportionately with the increasing size of a pupil in a post-LASIK patient.6,7
This case reinforced a key objective we share. We strive to ensure that the effective optical zone is always greater than the peak scotopic pupil size in refractive surgery. Also, just as important, we need to consider that increasing the effective optical zone should be weighed against the risk of excessively increasing the ablation depth.
Biomarker of happiness: Assess your patient’s pupil size and optical zone and plan accordingly to ensure an optimal outcome.
Patient #4: Blurriness and Glare
A 40-year-old female visited us after six months of blurred vision and glare. She had undergone femtosecond LASIK, OU, three years earlier and an enhancement, OS, one year earlier. Her refraction was -0.25 -0.25 x 40 and her vision was 20/20. We found dominant internal higher-order aberrations.
Biometry and a slit lamp exam didn’t show significant findings, so we decided to monitor her symptoms. The patient was lost to follow-up but returned a year later, still complaining of blurred vision.
This time, we saw obvious crystalline lens changes. The take-home message: For patients in the pre-presbyopic and presbyopic age group, watch for lenticular aberrations and a concerning “dysfunctional lens index.” (The index is a measure of the lens’s health/opacity used on the Tracey iTrace system; some surgeons use it to decide whether to offer patients refractive-lens exchange before they develop a textbook-definition cataract.) The DLI is an objective measure of the earliest, most appropriate time to consider RLE for the aging, dysfunctional lens.
This case highlights the importance of lens optics. Instead of an enhancement of previous refractive surgery, this patient needed cataract surgery, which we eventually provided.
Biomarker of happiness: Examine the crystalline lens of every refractive surgery candidate to precisely understand the origin of the refractive error.
Patient #5: Severe Dry Eye
A 37-year-old female was referred to us with severe dry eye. She had 20/20 vision three years after undergoing LASIK, but was extremely unhappy, noting that she was unable even to drive her car because of her symptoms. A dry-eye workup produced a TBUT of two seconds OD and three seconds OS. Her Schirmer’s result showed
14 mm and 12 mm of moisture, OD and OS. Her optical profile was normal. After lubricants, hot fomentation (compress) and meibomian gland massage failed to improve her symptoms, we scanned the meibomian glands.
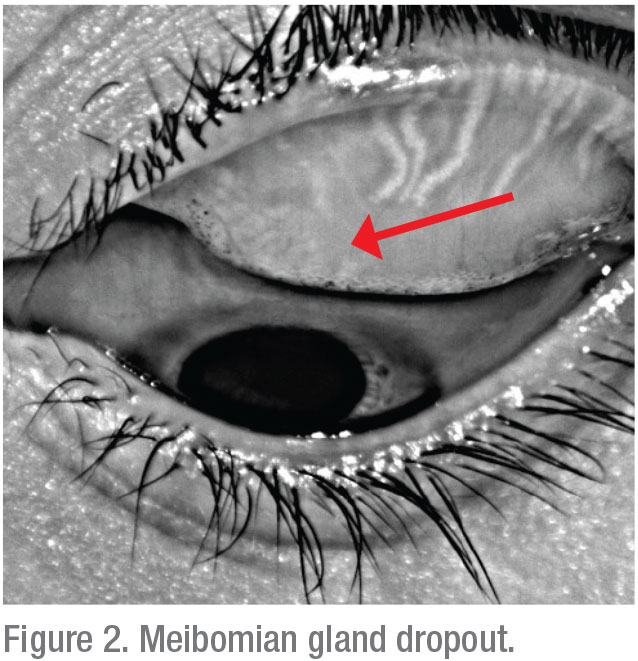 |
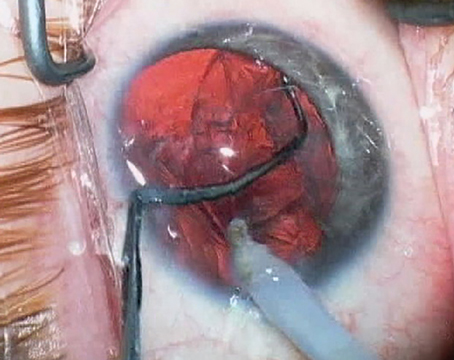
The scans showed significant gland drop-out (See Figure 2). This condition, missed preoperatively, had wreaked havoc in this patient’s life. Merely prescribing continued hot fomentation would have been futile. We recommended thermal pulsation therapy, such as treatment with LipiFlow, followed by topical steroids, antibiotic ointment for meibomian gland dysfunction, frequent lubrication and oral omega-3 fatty acids. These treatments improved her overall status.
Biomarker of happiness: A preop dry-eye workup can safeguard against an avalanche of postop inflammation.
Patient #6: Low-Vision Issues
A 25-year-old female high hyperope (+10 D) was experiencing glare. She had undergone RLE with a multifocal lens because she wasn’t a candidate for corneal refractive surgery.
Vision measurements of the operated eye showed a low modulation transfer function. A multifocal electroretinogram (mfERG) revealed subclinical maculopathy. We also evaluated the retina using a fundus exam and OCT.
Biomarker of happiness: Conduct preop retinal exams in all patients, investigating any degree of low vision.
Patient #7: Systemic Disease
A 22-year-old female came to us to undergo LASIK surgery. During preop testing, we found that she had low contrast sensitivity. After seeing pristine results in her anterior and posterior segment exams, we noted that she had no signs or symptoms of systemic illness and, as a result, determined that a possible neurologic problem could not be ruled out. The patient was referred to an internist and, subsequently, to a neurologist, who ordered an MRI and later diagnosed her with multiple sclerosis.
With this experience in mind, we now maintain a low threshold for referral when encountering complaints such as low contrast sensitivity, sudden vision loss, weakness of any part of the body, headaches and related symptoms. We know that optic neuritis is the most common visual disorder associated with MS. Besides loss of contrast sensitivity, of course, other symptoms of optic neuritis include blurred vision, dimming of colors and pain. In this case, we obviously couldn’t satisfy a patient intent on undergoing refractive surgery to improve her vision. However, we were able to take actions that led to her receiving the care she needed.
Biomarker of happiness: Always take time for a systemic evaluation, with the hope that your intervention can identify a disease process before it gets more serious.
Patient #8: Perfect—and Bitter
We saw a 25-year-old male one year after he had undergone SMILE, OU. He’d experienced no surgical complications and had achieved perfect visual results. However, this patient was bitter about his outcome, despite an emmetropic refraction. His topography, aberration profile and dry-eye workup were all markedly normal. So why was he bitter?
To find out, we reviewed his preop evaluation and expectations to discover that the patient had a history of anxiety. He also had been alternately compliant and noncompliant with his pharmaceutical regimen for obsessive compulsive disorder, and he was addicted to a number of drugs.
During our workup, we uncovered an interesting finding—a fluctuating pupil diameter, accompanied by a fluctuating refraction. Dynamic accommodation testing also revealed accommodation spasms. After testing, in collaboration with the patient’s psychiatrist, we documented a psychiatric evaluation that produced the following findings:
• Agreeableness: very low
• Conscientiousness: very high
• Neuroticism: high
We noted that a psychologically disordered state can cause pupil
fluctuations.8 The psychiatrist restarted the patient on treatment for his OCD.
This case shows the potential effect of any number of maladies on patient behavior. It also demonstrates the importance of patient behavior, one of the key factors for achieving refractive surgery success.
Biomarker of happiness: Always keep in mind that successful refractive outcomes depend on a combination of the eye’s optics and the patient’s mind.
From Tears to Brain
To solve a refractive surgery problem that defies explanation—which we must all try to do at times—we propose this type of systematic investigation, following a diagnostic trail that can lead from the tears to the brain.
By identifying any biomarkers of happiness that were missed in any of your patients, you can make sure you don’t miss them in the future.
Each biomarker discussed here provides an approach to decode sources of patients’ unhappiness before such unhappiness can occur in other patients, helping to advance our refractive surgery practices. The processes we’ve used can be replicated and expanded in your practice.
By understanding our patients, studying and perfecting optics, working up potential dry-eye cases, treating ocular surface disease, remaining mindful of lens profiles, utilizing retinal exams, relying on systemic evaluations, collaborating with other clinicians and harnessing research, we can achieve “20/20 happy” outcomes in the vast majority of cases. REVIEW
Dr. Shetty is a clinician, translational scientist and vice chairman of Narayana Nethralaya Eye Institute in Bangalore, Karnataka, India. He is also a professor at Sri Devaraj Urs Medical College in Kolar, Karnataka; an adjunct associate professor at MS Ramaiah Medical College in Bangalore; and BS affiliate associate professor and PhD guide at the Maastricht University in The Netherlands. Dr. Dhami is an ex-fellow of Narayana Nethralaya trained in cornea and refractive services and is currently heading the Cornea & Refractive department at Dhami Eye Care hospital, Ludhiana, Punjab, India. Dr. Israni is a consultant in cataract and refractive services at Infigo Eye Care, Mumbai, Maharashtra, India. Drs. Shetty, Dhami and Istrani report no financial relationships related to this topic.
1. Custer BL, Ballard SR, Carroll RB, et al. Refractive surgery: Malpractice litigation outcomes. Cornea 2017;36:10:1243-1248.
2. Herbaut A, Liang H, Rabut G, et al. Impact of dry eye disease on vision quality: An optical quality Analysis system study. Transl Vis Sci Technol 2018;12:7:4:5.
3. Shetty R, Sethu S, Deshmukh R, et al. Corneal dendritic cell density is associated with subbasal nerve plexus features, ocular surface disease index, and serum vitamin D in evaporative dry eye disease. Biomed Res Int. 2016;2016:4369750.
4. Koh S. Mechanisms of Visual Disturbance in Dry Eye. Cornea 2016;35 Suppl 1:S83-S88.
5. Shetty R, Shroff R, Kaweri L, et al. Intraoperative cap repositioning in small incision lenticule extraction (SMILE) for enhanced visual recovery. Curr Eye Res 2016; 41:12:1532-1538.
6. de Castro LE, Sandoval HP, Bartholomew LR, et al. High-order aberrations and preoperative associated factors. Acta Ophthalmol Scand 2007;85:1:106-10.
7. Wang Y, Zhao K, Jin Y, et al. Changes of higher order aberration with various pupil sizes in the myopic eye. J Refract Surg 2003;19:2 Suppl:S270-4.
8. Burley DT, Gray NS, Snowden RJ. As Far as the eye can see: Relationship between psychopathic traits and pupil response to affected stimuli. PLoS One 2017;12:1.