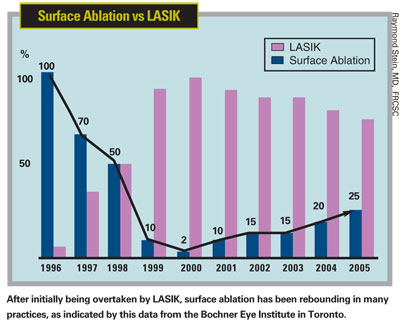
As a patient-pleasing refractive procedure, LASIK has been hard to beat. Some other ablative procedures have offered equally good visual results, but most have had comparative drawbacks such as greater patient pain or longer healing times.
Now, advanced versions of epi-LASIK (in which an epithelial flap is mechanically pushed back using a blunt, plastic oscillating blade, followed by laser ablation at the surface) are eliminating many of these drawbacks. These improvements have made believers out of many surgeons and their patients. If their enthusiasm is any indication, this could signal the beginning of a major shift in the marketplace.
To find out more about the latest iterations of epi-LASIK, we asked five experienced surgeons to share their experience and insights in response to four questions: Why did they decide to shift away from LASIK toward epi-LASIK? How do they minimize patient pain and prevent haze? Should the epithelial flap made during epi-LASIK be replaced on the eye or removed? And what pearls could they offer to help make epi-LASIK more efficient and successful?
The Move to Epi-LASIK
Most of the surgeons we spoke to began using epi-LASIK because some patients were poor candidates for LASIK; eventually, they ended up favoring it. Rick Milne, MD, who is in private practice at the Eye Center in Columbia, S.C., is a case in point. Dr. Milne has now performed close to 1,000 epi-LASIK procedures; his practice was one of the 10 international investigational sites for the prerelease of Moria's epi-K system.
The epithelial flap made during epi-LASIK avoids a host of potential flap complications associated with LASIK, and many surgeons now believe removing it speeds healing.
Barrie D. Soloway, MD, FACS
"Ninety-nine percent of the laser vision correction I do today is epi-LASIK—specifically, a version that most people are calling 'advanced surface treatment,' or AST, in which you completely remove the flap," he says. "Initially, I reserved epi-LASIK for patients who weren't good LASIK candidates, but they did so well that I kept finding more and more excuses to ablate the surface instead of performing LASIK. Eventually I asked, why am I still doing LASIK at all?"
Dr. Milne and others we interviewed mentioned a number of specific reasons they've come to favor epi-LASIK:
• It eliminates potential flap complications. Richard Rashid, MD, associate clinical professor of ophthalmology at the West Virginia School of Medicine in Charleston, estimates that he's performed more than 500 epi-LASIK procedures, and says that in the past year he's done about 75 percent epi-LASIK (with flap removal). "LASIK has a very low rate of complications," he notes, "but 90 percent of the complications that do occur are associated with making the flap, postop slipping of the flap or epithelial ingrowth. Epi-LASIK avoids all of that. And it's a safer eye in case of trauma in the future."
• More patients can be treated. Epi-LASIK can be used to treat many patients with thin corneas who would have to be excluded from LASIK treatment.
• Epi-LASIK doesn't weaken the cornea. Mark A. Swanson, MD, director of the Swann Institute in Sonora, Mexico and Douglas, Ariz., says his group has performed more than 800 epi-LASIK surgeries to date. "In my practice more than 40 percent of our procedures are epi-LASIK, and the number is growing," he notes.
One of the reasons he lists for this shift is that making a flap can undermine the biomechanical strength of the cornea, whereas epi-LASIK does not. "I've checked that with many instruments, including Reichert's Ocular Response Analyzer," he says. "This can be especially important when the patient has glaucoma. Epi-LASIK avoids weakening or thinning the cornea further, so we can continue to accurately monitor IOP."
• Healing is better than with PRK and LASEK. Dr. Swanson notes that some surgeons wonder why purchasing an epikeratome is necessary. "We compared a normal PRK to epi-LASIK done with a keratome," he says. "We found that it's better to take the epithelium off with the machine than with a brush or alcohol. The reason, I believe, is that we don't activate fibroblasts. The healing is a lot faster and pain is almost nonexistent, especially with the medications we use."
Dr. Rashid also prefers epi-LASIK to LASEK. "Epi-LASIK eliminates toxic alcohol symptoms, makes a better flap, provides a smooth Bowman's surface to ablate, reduces pain and saves time," he says.
• Epi-LASIK may reduce the need for enhancements. "My enhancement rate is under 3 percent with custom ablation done on the surface," notes Dr. Milne. "It was 10 percent when I did traditional LASIK."
• It's easier on the surgeon. Dr. Swanson says that he finds epi-LASIK to be much less stressful. "Most of the risk of refractive surgery is in the creation of the flap," he observes. "Epi-LASIK avoids that. You can enjoy doing it, instead of thinking about risks."
Patients Benefit, Too
Our surgeons also mentioned several advantages from the patient's point of view:
• Patients see it as safer. Dr. Milne says his patients have become more conservative in recent years. "Many of them have decided that they don't want LASIK," he says. "When their friends are having procedures that they understand are safe—there's no flap, nothing's being cut—they come in very eager for the procedure. It removes the fear factor. The only thing we needed to do was reduce the postoperative pain." In fact, Dr. Milne notes that his patient referrals have increased. He says this surprised him, but it seems to be a reflection of how satisfied his patients are.
• Patients may get better visual outcomes. Dr. Milne says that in his experience patients subjectively seem to do better, and objectively they have fewer induced aberrations. He believes that this has something to do with the effect of LASIK on Bowman's membrane. "If you've do PRK on top of a LASIK flap because there isn't enough stroma left underneath the flap," he says, "look at Bowman's after you remove the epithelium. It's no longer smooth—it's corrugated, with little micro-ridges throughout. [See image, below.] Once you lay a flap back down, there will be some microscopic contraction of the membrane, because the edges don't re-adhere normally. That's got to have an effect on visual acuity following custom treatments."
• Epi-LASIK doesn't denervate the cornea. This means patients have a much lower risk of post-surgical dry eye, compared to LASIK.
• Recovery only takes two to three days. Dr. Milne notes that one argument in favor of LASIK is the speed of recovery, but he says recovery from AST epi-LASIK is quite rapid. "I did a study of 100 eyes, and in all but three cases the patients were able to return to work by day three," he says. "I do epi-LASIK on Thursday, and Monday morning the patient is back at work, healed with the contact lens out.
Microscopic contraction of Bowman's membrane after the creation of a LASIK flap may result in micro-ridges. Above, epithelium has been removed to show the corrugated appearance of Bowman"s membrane 10 years after LASIK.

Rick Milne, MD
"These patients are in good shape right after the surgery," he adds. "They sit up and read the clock. Their vision may be 20/30 instead of 20/20 one day postop, but for somebody who's been 20/800 for years, that's huge. They're very wowed by it, and their vision continues to improve."
Manfred R. Tetz, MD, director of a private surgical center in Berlin and scientific director of the newly founded Berlin Eye Research Institute (BERI), estimates that he has performed about 1,000 epi-LASIK surgeries; he was the first surgeon in Berlin to offer it. He notes that one factor that helps to speed healing with epi-LASIK is the edge made by the keratome. "You get a very sharp, distinct edge on the flap," he says. "It's not like in the old PRK days when you used a hockey knife to remove the epithelium. The epithelium begins spreading across the cornea again immediately after the surgery."
• Recovery is far easier than recovery from PRK or LASEK. "This is nothing like PRK," says Dr. Milne. "We've all done PRK on patients who were not good LASIK candidates. They have a five- to seven-day recovery period that isn't pleasant, and that's not what people want.
"Epi-LASIK patients don't go through that at all," he continues. "It's the non-traumatic way you remove the layer of cells; the remaining cells heal very differently. That, combined with the postop medication combination I use has made this a very pleasant practice. [See "Pain Management: Key to Success."] The patients are really happy."
Should You Remove the Flap?
One ongoing epi-LASIK controversy centers around the question of whether the epithelial flap should be replaced or removed following the ablation. Four of the five surgeons we spoke to currently favor removing it.
Like many surgeons, Dr. Tetz initially replaced the epithelial flap. "The first year, we put it back," he says. "Then I lost one flap when a patient blinked before I could put the contact lens in. We soon discovered that that eye was healing faster." Dr. Tetz says he later tried doing one eye with the flap and one without in a small sample of patients. "I'd say that nine out of 10 times the patients preferred the removed-flap eye in the immediate postop period. Nowadays I completely remove it."
Dr. Tetz has noted problems with the flap that could account for the apparently slower healing when it's replaced. "I think that using a mechanical device to create the flap destroys some epithelial cells within the flap," he says. "When I used to put it back, I'd see little whitish islands in the flap for the first two or three days. Those islands were probably dead epithelial cells. I think that may account for the slightly longer initial recovery period. Also, the flap never fits. It seems to be stretched a little by the keratome, so it's always too large for the bed. If you try to put it back, you always have overlap."
Dr. Milne says that in his experience, replacing the flap can also cause problems that have a major impact on visual recovery. "With my first 100 epi-LASIK patients, I laid the flap back down," he says. "For 5 or 6 percent of those patients, visual recovery was delayed several months because they grew epithelial cells either on top of or underneath the flap. They ended up with multiple basement membranes, which affected their vision until the epithelium sorted it all out.
"In contrast, when you remove the flap, visual recovery is very quick," he continues. "The skin cells right next to where you've lifted the flap are completely healthy—they haven't been traumatized in any way. So they heal back across much more quickly than when they're removed with alcohol debridement or with a brush. And the cells that get pushed to the center are vital, so there's no central area of dead cells—one of the problems with PRK."
Some surgeons remain skeptical about the need to purchase a special instrument to push back the epithelial flap. However, surgeons with extensive epi-LASIK experience report that unlike other methods, this produces a clean edge with undamaged cells, leading to faster and more straightforward healing.
Barrie D. Soloway, MD, FACS
Dr. Milne adds that the main argument he's heard for putting the flap back is to reduce the incidence of haze. "If I'm doing a laser treatment that will go below 75 µm in depth, I use mitomycin-C 0.2 mg/cc for 20 to 30 seconds," he says. "I've treated almost 500 patients with this technique, and no one has developed haze."
Drs. Swanson and Rashid also started by putting the flap back on the eye, but have since decided to remove it. "At first, we did everything we could to salvage the flap," recalls Dr. Rashid. "We thought it formed an extra barrier against infection, and that it would make the patient more comfortable. We now believe patients are more comfortable without the flap, and we haven't seen any infections.
"If you leave the flap on," he continues, "the eye has two jobs to do: It has to remove the flap, and then replace it. By removing it, you take away one extra job for the eye. And you don't have the epithelial flap putting out cytokines and other inflammatory mediators to stimulate scar tissue."
The Jury's Still Out
Despite these observational reports, not all the data is conclusive. Barrie D. Soloway, MD, FACS, director of vision correction at the New York Eye and Ear Infirmary and assistant professor of ophthalmology at the New York Medical College, says his group has done more than 500 epi-LASIK cases. "We do about one-third surface ablation, and roughly 80 percent of those cases are epi-LASIK," he says.
Dr. Soloway's group at the infirmary is conducting a small, randomized study in which the flap is removed from one eye while the other eye has the flap replaced; no mitomycin is used. "As much as possible, we're doing it as a masked study," he says. "The patient isn't aware which eye had the flap put back on, but the examiner usually figures it out." Rather than checking Snellen acuity, Dr. Soloway's team asks patients which eye has better vision.
"So far, patients report slightly better vision on day one with the flap removed, and slightly better on day three with the flap left on," he says. "From one week forward, we've found no difference between the eyes. In terms of pain, patients initially report less pain with the flap left on. But by the third day, there's no difference in reported pain. In terms of haze, we've seen a trend toward slightly less haze in eyes in which we put the flap back. However, there was not much haze in either case, so this is just a trend."
He admits that putting the flap back on is more work for the surgeon. But asked what his preference is at this point, he says that he feels it's a function of the flap's viability. "It seems to me that if the flap is nice and clear and in good shape, it's worth putting it back on," he says. "Sometimes the flap can be hazy if it's been left to dry out, or it's been manipulated a lot. Probably in that case, you're better off not replacing it. I don't think there's hard and fast evidence that one option is better than the other."
Making the Most of Epi-LASIK
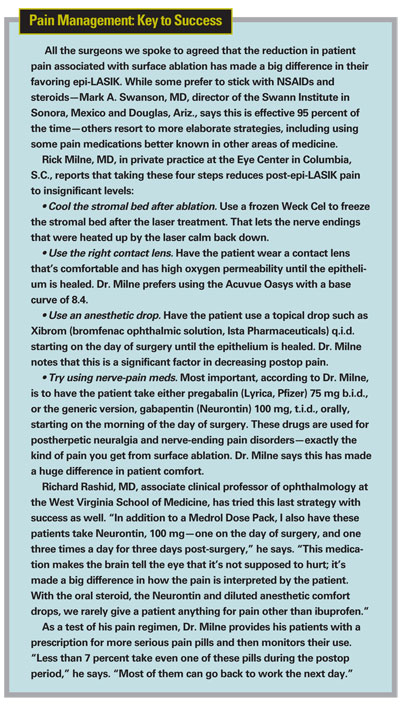
In addition to advice for managing pain (see "Pain Management: Key to Success"), our surgeons offered the following pearls for those considering offering epi-LASIK to their patients:
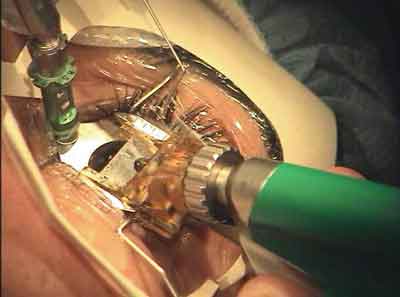
• Try using a "Rashid popsicle" after the ablation. Dr. Rashid says the following regimen, used after the surface ablation, has done a lot to enhance patient comfort and prevent haze. "I freeze two drops of Zymar and two drops of Acular, or a combination of Vigamox and Xibrom, in a special ice tray that has a rounded bottom like a test tube," he explains. "After I do the surface ablation I use mitomycin-C to prevent postop corneal haze, in every case. First I put a GenTeal gel barrier around the edge of the incision to protect the epithelial edge and stem cells in the limbal epithelium; then I apply the mitomycin within the GenTeal gel barrier on a sponge for an average of 15 seconds. Next, I put the frozen disk with the antibiotic and NSAID on the eye. [See image below.] It melts in 45 to 60 seconds.
"Finally, I irrigate all of that out with part or all of a bottle of cold BSS," he says. "This rinses away some of the antibiotic and NSAID, but whatever has soaked into the stroma will stay there. Once we put the bandage contact lens on, we apply more of the NSAID and antibiotic. Our results have been very good."
A "Rashid popsicle" is made by freezing a few drops of antibiotic and anti-inflammatory meds. Richard Rashid, MD, reports that allowing this to melt on the eye following ablation and use of mitomycin-C helps to enhance patient comfort and prevent haze.

• Vitamin C may prevent haze. Although mitomycin-C is a popular way to prevent haze—Dr. Swanson says his patients who received more than 6 D of correction often developed haze until he began using mitomycin-C 0.2% for 20 seconds—other alternatives also appear to work. Most notably, Dr. Tetz has his patients take one gram of vitamin C (any type) every day for one week before and two months after surgery. "Ever since we started having patients take oral vitamin C, I haven't seen any haze," he says. "Vitamin C seems to modify the wound healing, especially given in a dose like this."
• Treat infections first. "If you have an infection of the eyelids, such as blepharitis or chronic blepharitis, or patients with acne, you need to treat that condition before doing epi-LASIK, because chronic infections tend to activate fibroblasts and can result in haze," observes Dr. Swanson.
• If you remove the flap, don't worry about the hinge. Our surgeons agree that the clean, undamaged edge left by a mechanical epikeratome is a key to the fast, even healing that follows flap removal. Dr. Swanson says that he usually aims to leave no hinge at all, but that if one remains, it's no problem. "We control hinge size with a stop on the machine," he notes, "so we let the stop go free. Most of the time we take the flap off completely in one pass. But if a hinge remains, we just lift the epithelium and it detaches."
• If healing is abnormal, stop the steroids. Dr. Milne says that most patients are 20/30 or better once he removes their contact lens on day three. However, he occasionally encounters an outlier. "Some people's epithelium heals a little thick centrally compared to peripherally, and they have some astigmatic issues or unusual refractive errors," he says. "When they come in like that postop, I stop their steroids completely.
"Without the steroid drops, they remold the epithelium much more quickly," he continues. "I tell these patients that their vision might be fuzzier than they'd like for a week or two. By a month postop, they're all doing as well as I expect them to be doing."
• If you replace the flap ... Dr. Soloway offers these pearls if you plan to replace the epithelial flap:
1. Keep the epithelium wet. Dr. Soloway says that keeping the epithelium (not the bed of the ablation) wet allows him to move the flap around by squirting it with BSS. "I get the flap pretty wet with the BSS cannula and then use the cannula to bring it back over the eye," he explains. "The metal tool doesn't stick to the flap, unlike a Merocel or Weck cel. And the flap usually goes back into place in one fell swoop." Dr. Tetz also says that adding fluid while creating the flap helps to make it come off more easily.
2. Touch the flap as little as possible. "Leave it alone," says Dr. Soloway, noting that this can be hard for surgeons to do. "Manipulation tends to decrease the flap's viability."
3. Don't aim for an exact fit. "You're not looking for the same kind of fit that you want with a LASIK flap," he says. "The epithelial flap will be stretched a little bit, causing some overlap, and that's acceptable. If you try to put the flap back into a 'perfect' position, you'll manipulate it a lot, and you won't gain any benefit from having it put it in a different position."
LASIK: Is the End in Sight?
Given the apparent shift in the direction of epi-LASIK, we asked whether LASIK's days might be numbered.
Dr. Swanson says the option of not offering LASIK is questionable—at least right now—because of patient pressure. "LASIK has been on the market for many years, and the marketing has been so good that patients tell us they want it," he notes. "Sometimes it's hard to convince them that epi-LASIK is better, even if they're at risk with LASIK. The pressure from patients is still so great that I feel I can't change entirely. However, a lot of doctors in our four clinics now only do epi-LASIK, and that's a good thing."
Dr. Rashid believes epi-LASIK won't replace LASIK completely any time soon. "Epi-LASIK with the flap removed takes a few days longer to heal, and there's minimal discomfort in one out of 10 patients," he says. "Also, a lot of people have paid a lot of money to buy a femtosecond laser. They're not going to throw that laser away and start doing something else."
Nevertheless, the excitement about epi-LASIK is unmistakable. "It seems to be what patients are looking for," says Dr. Milne. "I can't find a downside to it. I've had a number of eye-care providers come in for laser correction, and all of them have wanted this procedure.
"I'll never go back to LASIK," he adds. "I don't see a reason to ever do it again."