Presentation
A 72-year-old Caucasian female was referred to the neuro-ophthalmology clinic for gradual development of diplopia and a drooping right upper eyelid. Six months prior to presentation, she struck her head against her car trunk door and developed a mild headache that resolved on its own. She didn’t pursue medical attention at that time. Two weeks after the incident, she noticed drooping of her right upper lid. Over a period of months, she developed binocular diplopia.
Medical History
Her past ocular history included dry-eye syndrome. Her medical history included diabetes, hypertension, hyperlipidemia, hyperthyroidism and remote history of breast cancer, for which she underwent mastectomy. She was on several medications including citalopram, ferrous sulfate, metformin, levothyroxine, losartan-hydrochlorothiazide, simvastatin and tamoxifen. She had no allergies to medications. Social history was significant for smoking one-half pack per day and occasional alcohol use. Her family history was noncontributory.
Examination
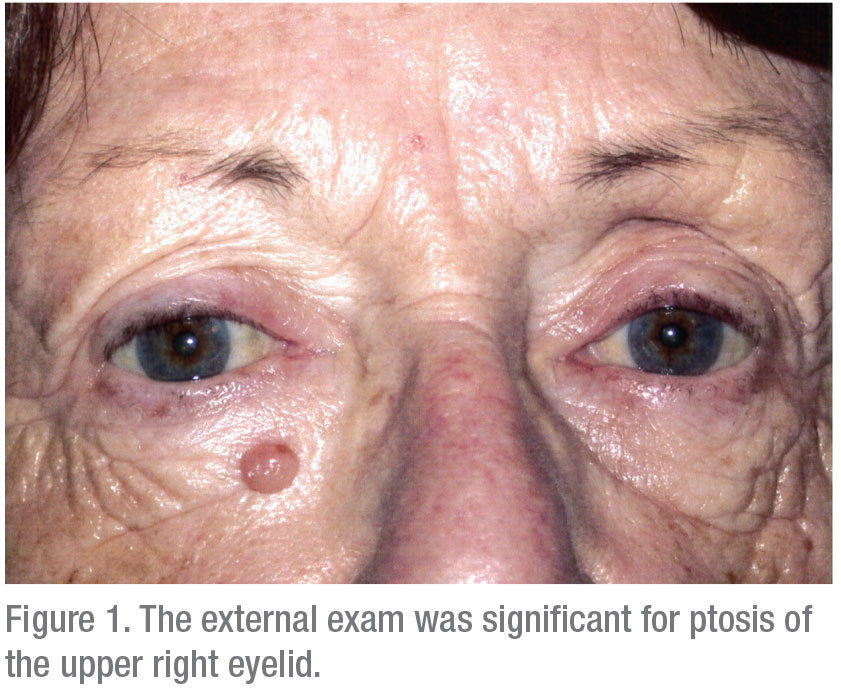
Ocular examination at her local ophthalmologist demonstrated visual acuity of 20/50, pinholing to 20/40 in the right eye and 20/20 in the left. Pupils were equal, round and reactive. Intraocular pressures and confrontational visual fields were within normal limits. Extraocular motility was notable for limited supraduction, infraduction and adduction in the right eye, but was full in the left eye. Her external exam was significant for ptosis of the right upper eyelid. Anterior exam and dilated fundus exam were otherwise noncontributory. The patient was referred to neuro-ophthalmology but was then lost to follow-up for several weeks.
Six weeks later, on presentation to neuro-ophthalmology, her examination was significant for anisocoria, a 3-mm pupil in the right eye and a 4-mm pupil in the left, with a greater difference in the dark. No afferent pupillary defect was noted. She was found to have 20 percent normal elevation and adduction, 60 percent normal depression and 80 percent normal abduction in the right eye. Left eye demonstrated full motility. On external exam, 3 mm of ptosis of the right upper lid was noted. She was orthophoric in primary gaze, with an exotropia in left gaze measuring 30 prism diopters and an esotropia in right gaze measuring 4 prism diopters. She also demonstrated downward displacement of her right globe and resistance to retropulsion of the right eye. Hertel measurement was significant for a 3.5-mm difference, right greater than left.
 |
What is your diagnosis? What further workup would you pursue? Please click this link for diagnosis, workup, treatment and discussion.



