As femtosecond laser technology has become an increasingly popular way to make LASIK flaps, interest in potential downsides and complications has also grown. Here, surgeons with experience using this technology share what they've learned about potential complications and how to manage them.
Transient Light Sensitivity Syndrome
Most femtosecond laser complications appear to be self-limiting, but one does require some treatment when it occurs: transient light sensitivity syndrome, or TLSS. Several weeks after surgery, these patients develop an intense sensitivity to bright light. This complication is rare—surgeons report rates ranging from one out of 100 cases to one out of 1,000 cases or less—and it is treatable, with no apparent long-term effect on quality of vision.
According to Perry S. Binder, MS, MD, who practices at the Gordon Binder & Weiss Vision Institute in
"Patients with TLSS present between weeks four and eight with symptoms that sound like iritis or cyclitis," says Dr. Binder. "These patients come into your office wearing sunglasses or holding their hands over their forehead to shield their eyes; the glare is just too much for them. However, their vision and refraction are fine; there's no sign of inflammation; the exterior eye is normal; the anterior chamber is free of cells and flare; and there's no ciliary flush. Nevertheless, the symptoms are of ciliary body inflammation."
Several theories have been proposed to explain the occurrence of TLSS. "My theory is that the gases expelled from the interface work their way into the ciliary body through either the trabecular meshwork or above the ciliary space in the episclera," says Dr. Binder. "If this happens, it could cause late-onset ciliary body irritation and trigger the symptoms." Dr. Binder says he suspects this mechanism because the eyes he's seen that have developed anterior chamber bubbles during surgery did not develop TLSS later.
Vance Thompson, MD, assistant professor of ophthalmology at the University of South Dakota School of Medicine, has used the IntraLase laser for more than five years. He believes the occurrence of TLSS is related to untreated ocular surface problems such as dry eye. "Typically, TLSS goes away with time and aggressive ocular surface management, using tools such as topical steroids, Restasis and punctal plugs," he says. He notes that he is aggressive about managing the ocular surface preop and has seen TLSS in less than 1 percent of his patients.
James P. McCulley, MD, FACS, professor and chairman of the department of ophthalmology at the University of Texas Southwestern Medical School in
"When we were using the 15-kHz IntraLase engine in our practice we had a couple of incidences of TLSS, and we noted that the patients appeared to have interface haze," he says. "We have tandem through-focus scanning confocal microscopy capability in our department, so we assessed those patients using that technology. We found that they had significant activation of keratocytes in and around the LASIK bed interface—more than you would see with a blade.
"Having observed that, we did two things: We lowered the energy of the laser and increased the postop topical steroids," he continues. "We found that this produced less activation of keratocytes and no cases of TLSS." He notes that the same approach has worked with the more recent versions of the IntraLase.
Dr. McCulley advises that surgeons make sure the energy settings are maximized for the side cut and the bed. "Some lasers are a little hot, some a little cold," he observes, "so you need to work with the company to make sure everything is as it should be. The spots should be 8 µm apart. In terms of steroids, I'd recommend q1h steroids for the first 24 hours postop while the patient's awake, then q.i.d. for a month, if you're using a 30-kHz engine. If you're using an FS60, I'd recommend q1h for the first 24 hours while awake, then q.i.d. for a week. Basically, if you start to see haze, you need to decrease the amount of energy being delivered and put the spots closer together. If that doesn't completely take care of it, increase the steroids a little bit."
Dr. Binder also treats his TLSS patients using steroids: hourly prednisolone acetate for about a week. "By then, in all but an extremely small number of cases, the symptoms are gone," he says. "And in all cases there are no permanent effects on vision or refractive error."
Vertical Gas Breakthrough
"When a femtosecond laser creates a light-induced optical breakdown in the interface, gases are produced," explains Dr. Binder. "These gases have to go somewhere. Usually, they dissect along the plane of least resistance, which is parallel to the surface along the collagen lamellae. But if there's an abnormality in the anterior cornea—either because of an abnormality in Bowman's such as map dot dystrophy, or because of a previous physical break in Bowman's such as pterygium surgery or foreign body injury—the gases will follow the path of least resistance and migrate vertically. This can also happen if for some reason the surgeon is cutting with very little stroma between the interface and the epithelium. In this situation the gases may escape through the epithelium and end up between the glass applanation plate on the patient interface and the patient's epithelium, where they'll prevent the excimer laser energy from getting through."
"The only way to get vertical gas breakthrough is if there's a defect in the corneal collagen," agrees Dr. Thompson. "That's why a good slit lamp exam is important. If a patient has a foreign body, contact lens or RK scar, or if the patient has had astigmatic keratotomy or conductive keratoplasty, you need to consider that a special situation. I warn these patients that gas breakthrough is a risk, and that if it happens we'll stop and have them return at a later date for a blade flap or PRK. Be sure to get proper informed consent in this situation."
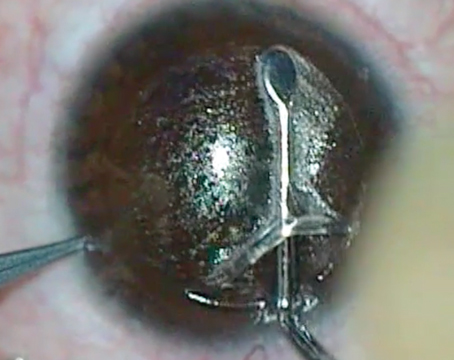
Dr. Binder says that if vertical gas breakthrough occurs it's easy to recognize through the microscope. "If the bubbles break through it looks like a big, black wet spot," he explains. (See image, below.) "If you see this, take your foot off the pedal and don't go any further. You can come back 30 minutes later, or the next day, the next week or the next month and cut deeper by 40 to 50 µm, as long as you leave sufficient residual stroma. The key message here is that if you stop, there's no harm and no foul, at least with the IntraLase. Unlike some other femtosecond lasers, the IntraLase has only cut into stroma at this point. You haven't touched Bowman's layer, which could induce refractive error." (For more on this, see "Continuing After a Partial Cut" below.)
"If you don't realize that you have vertical gas breakthrough and you continue with the procedure, the flap will have a 1-, 2- or 3-mm diameter section that wasn't cut," he continues. "If you then try to lift the flap, you'll tear a hole in it where it wasn't cut, creating what looks like a buttonhole. This is the only vision-threatening complication you can have if you're making a flap with the IntraLase. Of course, if it happens, it's the surgeon's fault, not the laser's." Dr. Binder adds that if the cornea is very thin and you have vertical gas breakthrough, the best option becomes PRK.
Anterior Chamber Gas Bubbles
Occasionally during surgery, the gases created by the laser migrate out through the peripheral cornea and make their way through the angle into the anterior chamber. "Anterior chamber gas bubbles that can appear during surgery are totally innocuous," says Dr. Binder. "They have no side effects and they're reabsorbed on their own. The only short-term effect is that they can interfere with some of the excimer laser trackers. In that case, you wait 30 minutes to an hour so the tracker will work, or do the case without using a tracker. It's as simple as that."
Dr. Thompson says that he has encountered anterior chamber gas bubbles on several occasions. "If I see two or three I pay close attention, in case more appear," he says. "My concern is that too many bubbles might lead to a rise in intraocular pressure, in which case I'd want to stop the procedure. So far, I've only ever seen a few bubbles."
Dr. Thompson notes that it's possible the bubbles could also interfere with fixation. "The bubbles rise to the highest spot, and when the patient is lying on his back that's the dome of the cornea," he says. "So the patient is looking through the bubbles. If it becomes a problem, you can simply lay the flap down and come back a different day to do the ablation component when the bubbles are gone."
Decentered Flap
While not necessarily the end of the world, a decentered flap can become a problem if it contributes to a decentered ablation, or if the surgeon tried to recut it and doesn't follow protocol. Our surgeons described three situations that can result in a decentered flap:
• Inaccurate suction ring placement. "Probably the most difficult part of the procedure is getting the suction ring well centered," says Dr. McCulley. "To help center the suction ring, I place ink marks at the limbus at three, six and nine o'clock, with the patient sitting up at the slit lamp just before going to the IntraLase, whether the patient is dilated or not. When the suction ring is placed, if I see one ink mark clearly and I don't see the other two, then I know I'm decentered. If I see no ink marks, then I know I'm pretty well centered. Most of the time I see just the border of all three marks. I try to position the suction ring so I see them equally."
• Pupil shift. "Pupil centroid shift can occur temporally with dilation," notes Eric D. Donnenfeld, MD, co-chairman of cornea and external disease at
• An abnormal pupil center. Dr. Binder notes that this is rare, but possible. "Ninety-nine percent of the time, if you just center treatment on the geometric cornea you're not going to get into trouble," he says. "However, a few pupils are not geometrically centered. You have to be aware of that prior to operating so you know where to center your surgery."
Lamellar Keratitis
With mechanical microkeratomes, this problem usually appears as diffuse lamellar keratitis; cells appear within the visual axis and grow more dense as they coalesce, eventually affecting vision. In some cases the flap must be lifted to allow irrigation.
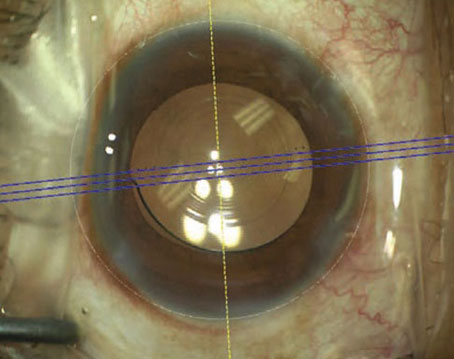
"With the femtosecond laser the problem appears as focal lamellar keratitis (FLK), although some people still call it DLK," explains Dr. Binder. "This has been described as a dusting of cells in the periphery in a doughnut shape, where the visual axis is spared. (See image, top of the page.) I saw this with the earlier IntraLase engines. It's related to two things: side-cut energies and flap lift technique. A new user who lifts the flap traumatically, and/or uses high energy when cutting the edge of the flap, may experience this. As you decrease your side-cut energies and improve your flap lifting technique, the problem disappears."
Dr. Binder says that when he first started using the IntraLase, he used 6 µJ of laser energy to cut the flap edge, which was recommended by the company. "Today, my side-cut energy is 1.1 µJ using my 60-kHz engine," he notes. "Some people use even less: 1 µJ or 0.9 µJ. If you look at my patients today, you won't see any FLK.
"In any case, the problem is not vision-threatening like the DLK you sometimes see described with microkeratomes," he continues. "That problem occurs as a result of something contaminating your procedure. When we encountered DLK in our practice we discovered that the enzymatic cleaner we were using to digest cellular remnants on our nondisposable instruments was contaminated with fungus. Since then, I've spoken to several new IntraLase users who said they were having DLK in the visual axis. When I walked them through the steps of their procedure they always found some contamination. Their DLK outbreaks were not related to the laser."
Epithelial Ingrowth
Epithelial ingrowth has been a frequent issue with microkeratome-created LASIK flaps, most often following enhancement surgery when the flap has been lifted for a second time and replaced. Days or weeks later, surface cells can grow through a defect in the peripheral wound and enter the interface.
Dr. Binder notes that the side-cut architecture created by a femtosecond laser can be totally different from that produced by a mechanical microkeratome. "A mechanical microkeratome cuts at an angle of about 28 degrees and doesn't generate significant wound healing," he says. "Most IntraLase users make the side cut at a 60- to 75-degree angle, making it more difficult for the epithelium to grow into it. Also, the wounds heal pretty solidly. I can lift up a mechanical MK flap that I made in 1995 without much difficulty. In contrast, lifting up a 60-kH IntraLase flap that was done six months ago is much more difficult because the wound is tighter. For these reasons, I don't see epithelial ingrowth very often. I suspect it will be much less common with any femtosecond laser than with mechanical microkeratomes."
Dr. Donnenfeld notes that in his experience epithelial ingrowth has been dramatically reduced by the laser flaps. "The edge of the flap is more of a perpendicular turn than a gradual slope," he observes. "It's harder for epithelial cells to migrate around a corner."
"There's also much less risk for flap slippage," says Dr. McCulley. "After my subspecialty day talk, a fellow came up to me and said his laser flaps sometimes slip. It turned out he was making a 30-degree side cut. The manhole cover cut essentially eliminates this problem."
Not everyone has seen a decrease in epithelial ingrowth with femtosecond laser flaps, however. Dr. Thompson says that he believes his rate of epithelial ingrowth with flap lifting for laser enhancements has been slightly higher since he began making laser flaps. "I've wondered whether epithelial ingrowth is related to the fact that the side cut, no matter how thin a laser makes it, is an excision, not an incision," he says. "When I enter at the side of the flap to separate the interface, I try to avoid pushing in too much epithelium with my spatula. Then I separate the edge of the flap from the inside out as much as possible. After I lift the flap, I carefully inspect the area where I did push in, looking for epithelial cells, which I can remove with a Weck-cel because they're not yet adherent.
"Also, I remove any epithelium from the back of the flap, not just the corneal bed," he adds. "That's helped lower my rate of epithelial ingrowth significantly. If ingrowth happens again, I clean off the epithelium and suture the flap." He notes that a suture can securely close that potential space and prevent any further recurrence of epithelial ingrowth, but says the need for this in his practice is rare.
Preventing Problems
Our surgeons offer the following additional suggestions:
• Stay focused during flap creation. "Surgeons sometimes focus a little less when the laser is doing the job," observes Dr. Thompson. "In fact, we need to be thinking about angles, energy levels and accurate placement and stay alert for problems. We can't just point and shoot."
• Coach the patient to prevent a partial flap. "I try to get the patient into a comfortable position with the head or face parallel to the floor, so the chin isn't too high or low," says Dr. Thompson. "Once I've achieved quality suction I remind the patient to not let the chin drift up or down, which people tend to do when they're nervous."
• Applanate sufficiently. "If you don't applanate enough, you may get a pseudo-meniscus, so you're operating on too moist of a surface," says Dr. Thompson. "The flap could come out thinner than it's supposed to be, or very thin on the edges."
• Measure your flaps. "IntraLase lasers are all calibrated at delivery and they self-calibrate every day when you turn them on," says Dr. Binder. "They're also calibrated monthly by technicians who come to your office, but you can still have unexpected changes in ablation depth. You have to keep measuring your flaps in order to be very accurate and to know when something has changed.
"One advantage of the femtosecond laser is that you can take a single measurement to determine flap thickness," he continues. "Once you've cut the flap, before you lift it, the signal from an ultrasound probe will be reflected by the gases at the interface. So, you can get a direct reading of the thickness of the flap without lifting it, which is called Eisner bubble pachymetry. This is a big advantage because you can see what you've got before you lift the flap up. If you have limited tissue to work with and for some reason the cut has ended up deeper than you expected, you don't have to lift it. This will also allow you to adjust the setting before doing the second eye."
Dr. Binder says this has helped him avoid problems on more than one occasion. "In one case the bubble pachymetry on the first eye repeatedly read between 40 and 50 µm," he says. "That meant I was cutting right below Bowman's layer, and I was able to verify this at the slit lamp. So I didn't lift that flap at all. I waited for two weeks and made a new, thicker flap and never had a problem. That saved me from violating the patient's cornea." Dr. Binder notes that he probably could have gone back and completed the procedure the next day, but says he prefers to be conservative in this situation.
• Use appropriate flap lifting technique. "All of the IntraLase lasers cause a more vigorous keratocyte activation in the bed adjacent to the side cut of a LASIK flap," notes Dr. McCulley. "That means the LASIK flaps heal in place more vigorously in the periphery. So, when lifting a flap for a retreatment you have to do blunt dissection not only in the side cut, but often in the peripheral portion of the bed. Once you've broken through that section, the flap will lift with not much more difficulty than a microkeratome flap."
Dr. McCulley describes his retreatment lifting technique as follows: "At the slit lamp I outline roughly a clock hour, or an hour and a half, of the side cut using marking ink on a Sinskey hook," he says. "Then I use a Sinskey hook to start my dissection down through the side cut. Later, when the patient is under the laser, I take that same Sinskey hook and bluntly dissect down to the bed. Then I direct the Sinskey hook under the peripheral edge of the flap to bluntly dissect that portion of the seal between flap and bed. Finally, I place my retreatment spatula through that area. The rest differs very little from lifting a microkeratome flap."
Dr. Thompson describes the technique that has helped him minimize problems when lifting laser flaps. "It's important to try to enter the side cut at the same relative angle that you used when you created the side cut," he explains. "If it's a 70-degree angle side cut, I try to enter at 70 degrees. (If you enter with too little of an angle you can get under the epithelium and think you have a partial flap.) You want to pop through the side cut to its base in the stroma and then angle your separating tool to be more parallel with the cornea.
"Some surgeons would then try to dissect the interface in one sweep," he continues. "That can put a lot of stress on the cornea. If you have an 8-mm-diameter flap and a 45-degree hinge, there's a good chance you'll tear the flap from the hinge. Remember, in many cases we're making 110-µm flaps with 50 µm of epithelium and only 60 µm of collagen, which is thinner than a human hair."
Dr. Thompson says he often makes three or four gentle swipes to dissect the interface. "It depends on how much friction I encounter," he says. "If there's a lot of friction, I do a lot of passes to separate the adhesions. If it's just a little bit of friction, then one or two swipes is often enough."
Dr. Donnenfeld offers another suggestion: During dissection, press down rather than lifting up. "You can tear a flap if you're too aggressive with the spatula, especially when working with very thin flaps," he notes. "So, when you're passing your spatula into the interface, press down against the stromal bed rather than lifting up. Your force will be dispersed posteriorly rather than stressing the flap."
• Consider not lifting ultrathin flaps for enhancements. "I'm a big believer in thin flaps, although I would never go thinner than 80 µm," says Dr. Donnenfeld. "Thin flaps lie better and cause less dry eye and fewer folds. I've lifted microkeratome flaps eight or nine years later, but I think you run the risk of damaging a very thin laser flap if you attempt to lift it years later, especially if it's well adhered. I'll probably be doing more PRK enhancements in the future as a result."
A Move in the Right Direction?
All of the surgeons we spoke to feel that in general, femtosecond laser technology has reduced the number and seriousness of LASIK flap complications they experience. "The earlier generations of the IntraLase weren't as good as a keratome, but the most recent generation —the 60-kHz version—has resolved all of my concerns," says Dr. Donnenfeld. "It doesn't eliminate complications completely, but it reduces them significantly compared to mechanical microkeratomes."
Dr. Thompson agrees. "I haven't seen any vision-threatening complications," he says. "I don't have to worry about the laser creating a partial flap, a buttonhole, a free cap or a flap that's too thin or thick or wide or narrow. Any issues with this laser really arise from how the surgeon uses it. It does what you ask it to do."
"The fact that we have significantly fewer complications has probably added about 10 years to my life," adds Dr. McCulley. "It makes my job a lot less stressful."