IntraLase Increases Its Skill Set
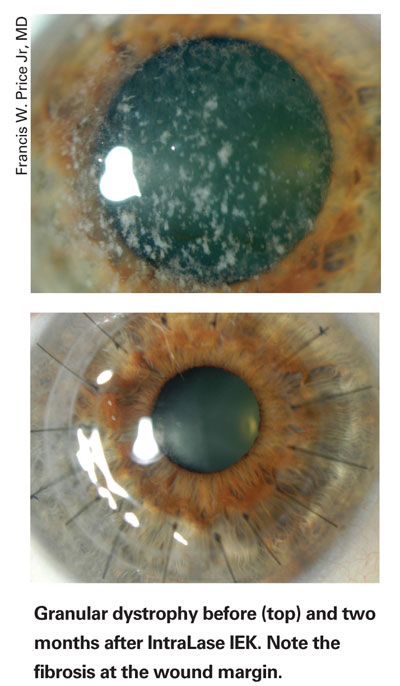
The latest upgrade for the IntraLase/AMO FS Laser increases its functionality in the corneal realm. The IntraLase-Enabled Keratoplasty upgrade enables surgeons to go deeper with their corneal laser cuts and perform penetrating keratoplasty for conditions such as keratoconus and corneal scars.
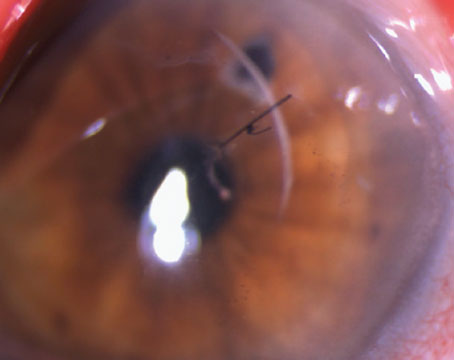
"The upgrade is both a software and a hardware change," says Indianapolis surgeon and IntraLase consultant Francis W. Price Jr., MD, who received the world's first IEK upgrade in July. "It allows you to go deeper than 400 µm, which is the current limit for the laser's LASIK programs. With this, you can go to 1,200 µm, a huge change. Without the upgrade, there are limited programs for different incision contours, but this software lets you do complex incision designs [that] crisscross and intersect." Since he's received the upgrade, he's performed 22 penetrating grafts and some AlphaCor (Coopervision Surgical) artificial cornea transplants with it. The treated conditions have included pseudophakic bullous keratopathy, cornea scars, corneal dystrophies and keratoconus.
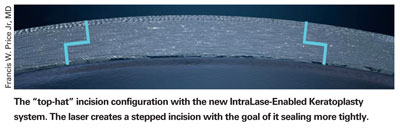
Increased depth aside, however, the main value of the new upgrade is the ability to create incisions in a variety of different shapes, with the goal of having the final graft fit better naturally without the need for ultra-tight sutures to make the wound watertight. The laser's programmability allows the user to specify the shape he or she wants for the best wound closure and overall architecture.
"With the stepped, or contoured, incisions, in many cases you can get very rapid, though not complete, wound closure," says Dr. Price. "You can get partial wound closure to the point where the wound is basically watertight or holds pressure during surgery, if necessary."
Roger Steinert, MD, vice chair of clinical ophthalmology and director of refractive, cornea and cataract surgery at the University of California, Irvine, performed the laboratory work validating the IEK system, and has performed 28 IEK procedures. He says the contoured incisions help solve some of the problems that have been associated with traditional trephine-based keratoplasty procedures.
"The issue has been that corneal transplantation is reasonably successful in getting a clear transplant in most patients, but less successful in getting an optically good cornea," he says. "High amounts of astigmatism, that require a rigid contact lens rather than glasses, and irregular astigmatism are essentially the norm with corneal transplants. So, patients have some real challenges in terms of getting their vision into focus, and commonly don't get their best vision because of these optical distortions, which, in most cases, result from the way the transplant sits in the recipient's cornea; if the graft isn't perfectly aligned, distortions occur." He says that distortions can also occur for several other reasons: if the front surface isn't contoured perfectly; if the patient ends up with more than 50 percent of the graft tissue in less than 50 percent of his available corneal space, which can occur due to the cornea's flexibility; if excess suture tension delays visual recovery; and if wound healing causes the eye's optics to shift over time.
Dr. Steinert says the laser isn't subject to the same constraints as a corneal trephine blade, which simply makes a straight-in cut. Instead, the laser beam rotates, with each pulse cutting a bit of tissue.
"You can bring it from the anterior chamber upward slowly and progressively to the front surface and follow virtually any pattern you want," says Dr. Steinert. "The basic concept is that you can create planar areas in the incision, or steps. So, we're evolving the shape of the incision to be more like the clear corneal incision in cataract surgery that seals itself with an inner flap that pushes up against the back side of the incision."
So far, the following three types of incision shapes have emerged with the IEK upgrade:
• The top hat. Dr. Price says he uses this design the most. "With the top hat, you have a central cut diameter of about 7 mm, with an anterior cut going down into the stroma 200 to 300 µm," he explains. "Then there's a flange, called a ring cut, that goes out a millimeter or two, then another vertical cut into the anterior chamber at about
9 mm in diameter. It's kind of like a drain plug, where you have more tissue in the posterior part, so the pressure in the eye naturally closes it. You also get more endothelial cells posteriorly compared to the anterior part, so it's a nice alternative for people with endothelial problems, like pseudophakic bullous." (A cross-section of a top-hat cut appears above.)
• The mushroom. This is essentially the opposite of the top hat, explains Dr. Price. "With the mushroom, you do the 9-mm diameter cut anteriorly on the corneal surface, go down through 300 µm and do a ring cut that actually goes inward," he says. "Then, when you perforate into the anterior chamber, it's at the 7-mm diameter. This is an edge configuration you might want to use for people who have good endothelial cells, so you'd like to preserve as many as possible to minimize the chance of corneal decompensation if there's rejection of the donor. It's nice for keratoconus patients or those who have scars but a good endothelium."
• The zigzag. Dr. Steinert developed this pattern. "I moved quite rapidly from the top hat to this configuration," he says. "It's called the zigzag because it looks kind of like a lightning bolt or the letter 'z' in cross-section. The incision angles up from the anterior chamber then goes across on a horizontal, giving the ceiling effect, then it angles upward again to the surface."
In terms of restoring functional vision, Dr. Price says that depends on how the surgeon does the sutures. "The fact that the wounds are contoured gives you the ability to not have to put as much tension on the sutures to get the incision to be watertight," he says. "This allows better visual recovery because the sutures cause visual distortions on the surface." Drs. Steinert and Price say the contoured incisions let them remove the sutures at an earlier time, on average, compared to conventional PKs. They say the nature of the IntraLase's effect on the tissue, its micro-explosions that cut the cornea, may also stimulate a keratocyte reaction and increased scar formation that enhances healing time. However, this hasn't been proven yet.
"The fact that I can get these sutures out at six or eight months postop instead of one and a half or two years is a tremendous improvement for these patients," says Dr. Price.
In terms of astigmatism results, Dr. Steinert has some preliminary observations. "The optical results with this technique would require a prospective, randomized study to determine," he says. "But, based on historical PK results as controls, we're doing better with IEK. For example, in my initial patients with sutures in at three months, there was an average of 3 D of cylinder, 75 percent were under
3 D, and some were below 0.5 D. That's not impossible to get with a regular transplant, but it would be unusual. The early astigmatism in our historical control patients was 5 to 6 D on average with the sutures in place at three to six months."
The other aspect of the IEK system that the surgeons and IntraLase researchers are trying to perfect is the creation of radial guide marks on both the recipient and the host.
"Since the laser is cutting the donor and the host in exactly the same way, and everything is known about the parameters of the cut, the pattern of those cuts could be laid down in the same way," says Dr. Steinert. "This would help the surgeon enormously in putting the eye back together and getting everything lined up correctly with the graft in place and avoiding optical distortions postoperatively."
The benefits of IEK come at a price, however. The IEK cutting step is just the first phase in the procedure. The surgeon makes the initial incision wounds in his laser suite, but doesn't finish them there. Once they're made, the patient goes to the operating room, either at a hospital or an ambulatory surgical center, where the transplant is finished manually. "Using IntraLase doesn't speed up the procedure," says Dr. Price. "You still have to cut the uncut portion and put in some sutures, so the transplant in the operating room essentially takes the same time as before, but with the extra time to perform the IntraLase on the patient in the laser center." Dr. Price notes that adding IEK to the graft process also costs more, since the surgeon needs the sterile supplies for the IntraLase and staff to carry out the procedure. "Our estimate is that it basically doubles the cost of doing the procedure," says Dr. Price. "However, I think it pays off in the end. It gives the patient the option to choose more rapid visual recovery if that is important to him. There's no comparison between manual incisions and IEK; it's like night and day."
The Femtec Adds Functions
Another femtosecond laser from Europe, the Femtec by 20/10 Perfect Vision (Heidelberg, Germany), is approved by the U.S. Food and Drug Administration but isn't yet available for sale in the United States, though the company intends to distribute it here eventually. Its maker recently added new features to the device.
The first upgrade is a modification to the corneal interface, incorporating a two-part spherical patient interface consisting of a spherical contact interface and a separate suction ring. The spherical interface is attached to the laser cone, while the surgeon manually applies the suction ring to the eye and in that way secures a proper centration. The modification incorporates a softer suction lip that enables a gentler fixation of the suction ring on the eye, and which the company says virtually eliminates hemorrhages.
"The system is really built around the spherical patient interface, which provides the area of interface between the patient and the system," says 20/10 Perfect Vision's Sales Manager, Gwillem Mosedale. "In our case, the interface is spherical, so it's much more adapted to the cornea than a flat interface. You don't get the intraocular pressure increase that you get with a flat interface, patients normally don't suffer blackouts during the procedure, and it gives us increased precision, particularly at greater depths."
A second addition to the system is a radial-force detector.
"The radial-force display helps you determine that the suction ring is level and that you, therefore, have good contact across the whole area of the interface lens and the cornea," explains Mr. Mosedale. "The device consists of a star-shaped group of LED lights that give you the direction of any radial force that's detected on the cone, which could be a sign of imperfect docking. The ideal docking procedure is one where there's no radial force, just upward pressure on the cone."
If the docking is grossly off-center, a red light will activate and the laser won't fire. A green light indicates that there are no shearing forces that could interfere with the procedure.
The system has also received software upgrades to allow it to further enhance different procedures, namely lamellar keratoplasty, penetrating keratoplasty, channel cuts for Intacs and astigmatic keratotomy.
"Our system is very proficient at greater corneal depths," says Mr. Mosedale. "We increased the depth at which it can work to 1,500 µm, which permits us to cut even edematous corneas. We're working on new shapes, as well. At the moment, we're getting good results with the incision shapes we have [for keratoplasty], with faster healing time and the ability to take the sutures out in about half the usual time."
As to when the system might reach the United States, Mr. Mosedale can't give a definite time, but says it's going to happen. "We will certainly enter the United States," he says. "We're currently looking for a partner to provide distribution and support when we enter the U.S."
The Visumax Enters the Arena
In mid-January, Carl Zeiss Meditec received U.S. FDA approval for its femtosecond laser, the Visumax. Here's an early look at its features.
The company says the applanation glass that contacts the eye is designed such that it minimizes any increase in intraocular pressure and doesn't impair perfusion of the central retinal artery, allowing patients to continue seeing the fixation light. "We have a curved contact lens, so the flap cut isn't a direct across-the-eye cut as you'd have with a mechanical microkeratome," says James Taylor, president and chief executive officer of Carl Zeiss Meditec. "Rather, it's a cut that tries to keep a uniform flap thickness throughout the cut, while following the shape of the cornea."
The company also mentions the laser's potential to not only be used for LASIK flap creation, but for an actual refractive procedure, as well.
"Basically, what we've demonstrated from a feasibility standpoint, at the same time we were doing essentially standard flap cutting, was the ability to do a lenticule extraction," explains Mr. Taylor. "So, rather than vaporizing the tissue, you cut a slice of corneal tissue and then remove it.
"We recognize that there's a significant amount of clinical development work that needs to continue to demonstrate what the real advantages of that would be, both from a clinical outcomes standpoint as well as a patient procedure standpoint."
The Visumax can also be used as part of a system that includes the MEL-80 excimer laser, enabling a surgeon to just enter patient data one time and use the same patient bed. In this way, instead of performing the flap cut, then moving the patient across the room or into another room for the refractive cut, the staff just pivots the patient bed, placing him or her beneath the MEL-80.
The company isn't discussing the laser's price at the moment. That will be set as the device nears commercialization, which looks to be around the middle of 2007.
"As we get closer to the commercialization time point, we will be releasing detailed specs plus further detail on the clinical data," says Mr. Taylor.
"We think the femtosecond platform is one that clearly has significantly broader potential than has been explored thus far in previous generations of systems," he says. "And we think the overall system solution approach makes a great deal of sense."
The Femto LDV Progresses
The Femto LDV (Ziemer Ophthalmics; Port, Switzerland), formerly known as the DaVinci, though approved in the United States, is in the middle of real-world clinical validation in Europe.
The company has two pre-production lasers that it transports to several sites for use on normal LASIK cases. Surgeons at these sites have performed just over 200 LASIK cases with the Femto LDV as of early January.
"The purpose of the validation is, among other things, to fine-tune the nomograms for practical use in standard refractive practice, and that is proceeding well," says Anton Wirthlin, PhD, Ziemer's vice president of marketing. "Using the mobile setup is actually part of the validation, if you will, by proving to ourselves that the claim of mobility is well-founded. It's no problem to put this device in a van, take it someplace hundreds of miles away, unload it and have it working." He says that this mobility may be interesting only to users who plan a mobile setup, though this number could increase if Ziemer adds the ability to perform different procedures with the Femto LDV.
"People are interested in the laser having multiple applications," he says. "They're interested in using the Femto not just as a flap maker, but as a device for a variety of corneal surgeries, such as carving tunnels for Intacs, lamellar keratoplasty and penetrating keratoplasty. In order to do keratoplasties in real life, you'd need a laser you can take in and out of the operating theater in a reasonable amount of time, because these surgeries have to be done there." Dr. Wirthlin says the company is committed to enabling its laser to perform these other procedures, and expects it to be able to sometime in 2007.
Dr. Wirthlin says Ziemer has currently taken several European orders for the laser, but it hasn't shipped yet. He expects the first production units to ship out in late January or early February. He also says a unit has been earmarked for shipment to the United States.
"One of the first will go to the United States," he says. "I believe that model, though it will be for use in general refractive practice, will also serve as a demonstration and referral site. The surgeon there will also do some clinical validation studies."