A 60-year-old Caucasian man presented with a chief complaint of progressively worsening floaters in both eyes, with the left eye being worse than the right. His symptoms began three months prior to presentation, and the floaters progressively increased over the three weeks preceding his presentation. He also noted a gradual decrease in vision OS.
Medical History
The patient had no prior ocular or medical history. His past surgical history was significant only for inguinal hernia surgery. He smoked a pack per day for approximately 20 years. Family history was non-contributory and there were no known drug allergies. He was not taking any medications. Review of systems revealed no new
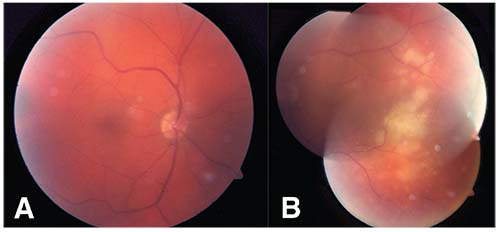 |
| Figure 1. Fundus photograph of the right eye demonstrating slight vitreous haze but otherwise normal fundus (A) and the left eye demonstrating multiple creamy yellow sub-RPE lesions in the temporal macula (B). |
Examination
On examination his best corrected visual acuity was 20/40 OD and 20/200 OS. His pupils were equal, round, reactive to light with no relative afferent pupillary defect. Extraocular eye movements were full bilaterally. His intraocular pressures were 20 mmHg OD and 19 mmHg OS with applanation tonometry. Slit lamp examination was only remarkable for 1-2+ fine vitreous cells bilaterally.
Funduscopically, the right eye was normal with the exception of mild vitreous haze. The left eye revealed multiple creamy yellow subretinal pigment epithelial lesions in the temporal macula, suspicious for a subretinal, sub-RPE or choroidal infiltrative process (See Figure 1).
Click here to view the Diagnosis & Discussion.



