Workup, Diagnosis and Treatment
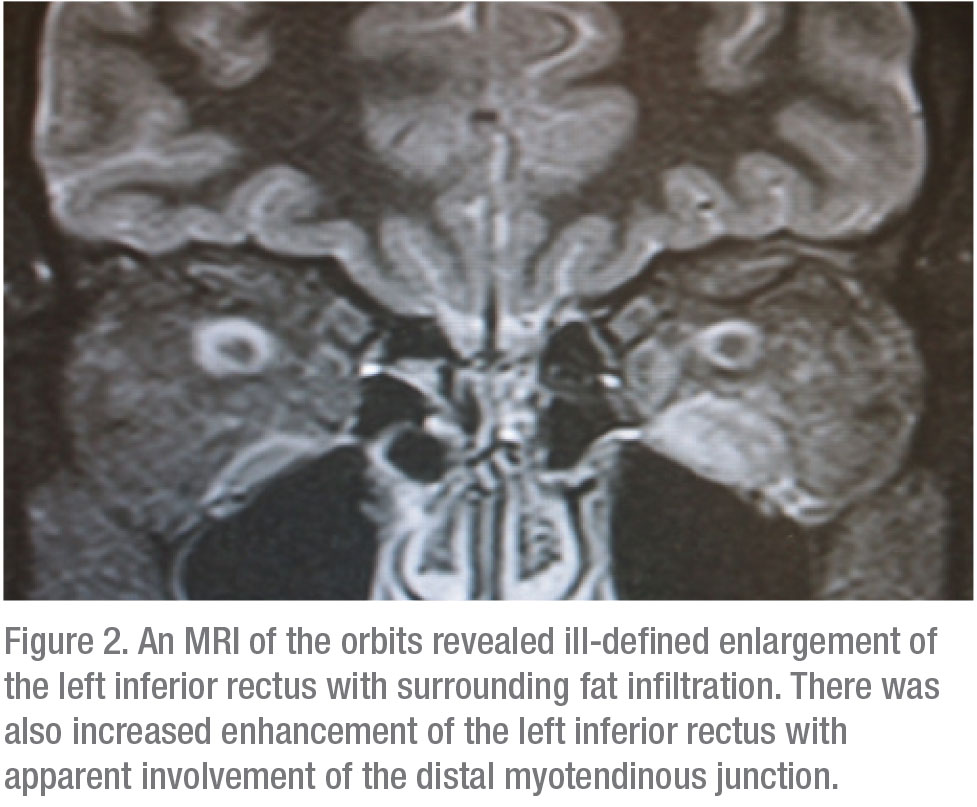
Laboratory studies, including thyroid testing, acetylcholine receptor antibodies, antineutrophil cytoplasmic antibodies and angiotensin converting enzyme returned normal. An MRI of his orbits revealed ill-defined enlargement of the left inferior rectus with surrounding fat infiltration. There was also increased enhancement of the left inferior rectus with apparent involvement of the distal myotendinous junction (Figure 2). A biopsy of his inferior rectus muscle revealed dense fibrous tissue with mild chronic inflammation. There was no evidence of malignancy. This compilation of findings made orbital myositis the most likely diagnosis.
He was started on 60 mg of prednisone daily. He still complained of diplopia in primary gaze, which mildly improved after an intralesional injection of betamethasone/dexamethasone to the scar tissue present in the inferior fornix proximal to the left inferior rectus muscle. His headaches resolved with Botox to the brow area.
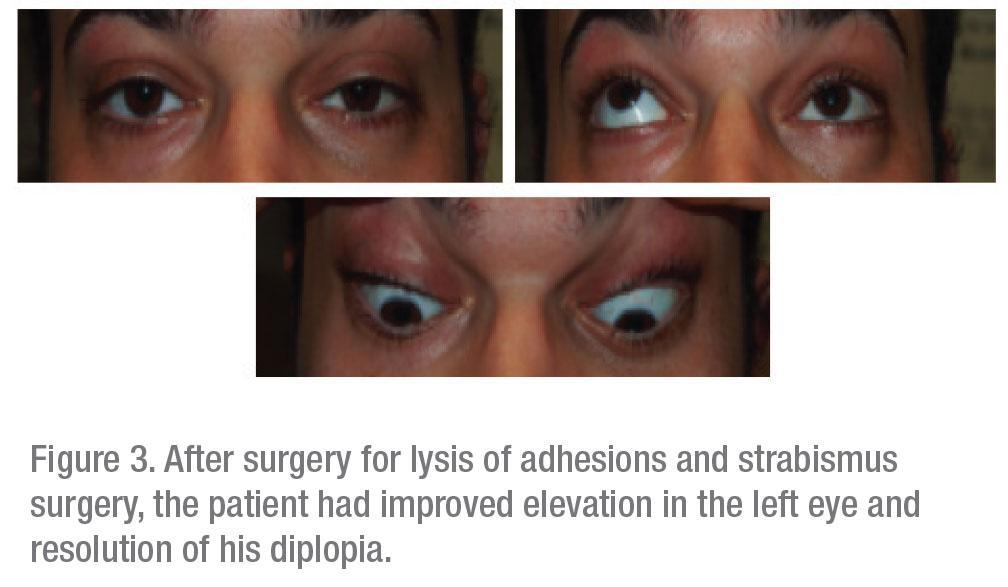
The patient was taken to surgery for exploration of his inferior fornix. During the procedure, it was noted that the left inferior rectus was firmly adhered to the orbital floor and its surrounding structures. A lysis of adhesions was performed, followed by a left inferior rectus recession with adjustable sutures. Finally, a conjunctival graft was placed to prevent re-adhesion.
After the surgery, the patient’s diplopia fully resolved and he was able to taper off of all steroids (Figure 3).
 |  |
Discussion
The differential diagnosis of extraocular muscle inflammation is broad and includes inflammatory (i.e., orbital myositis, thyroid eye disease, sarcoidosis, ocular myasthenia gravis), infectious (TB, lyme, trichinosis, cysticercosis), trauma-related, and neoplastic (lymphoma, metastatic) etiologies.
The findings in our case suggested orbital myositis as the etiology. Orbital myositis is a rare inflammatory disorder of single or multiple extraocular muscles.1 The most classic symptomatic manifestations are diplopia, unilateral presentation and orbital pain. Compared to thyroid eye disease, orbital myositis isn’t commonly associated with systemic symptoms and is less likely to present with proptosis.2
Orbital myositis falls into a larger disease spectrum called idiopathic orbital inflammation. IOI was first described by Birch-Hirchfield in 1905 and was initially referred to as “orbital pseudotumor” because of its appearance as a benign, non-infectious, space-occupying lesion in the orbit or enlargement of an orbital structure. IOI can either be nonmyositic—such as dacryoadenitis or orbital fat inflammation—or myositic. The pathogenesis is unknown, but it has been associated with infectious processes, including upper respiratory illnesses and flulike viral illness. There may also be a link between orbital myositis and systemic immunologic disorders, such as Crohn’s disease, systemic lupus erythematosus and rheumatoid arthritis.
The Orbital Society’s defined criteria for the diagnosis of IOI include the presence of orbital pain, pain with eye movements and an acute or subacute onset (days or weeks) with slow progression. Imaging such as CT or MRI assist in localizing the inflammation. Atypical findings, including irregular edges, nodularity, focal intramuscular mass on imaging, orbital fat infiltration, lacrimal gland enlargement or swelling, orbital nerve enlargement and/or sinus disease may be indications for biopsy. Serologies such as inflammatory markers and autoantibodies may be falsely negative in patients with disease limited to the orbit, or with mild systemic disease. Myositic IOI can be diagnosed by clinical resolution or improvement in symptoms within 48 hours of starting steroids. The diagnosis may also be made with a biopsy, in which case histopathology will show a nonspecific, polymorphous infiltrate of small, well-differentiated lymphocytes (primarily T cells), plasma cells and neutrophilic and eosinophilic granulocytes. Indications for biopsy include the absence of pain, subacute onset, a loss of function resulting in extraocular motility deficits, failure to respond to corticosteroids, or a disease recurrence while tapering corticosteroids.3
A myriad of treatment options are available for treating IOI. If the case is mild, observation is an option. A three-week trial of nonsteroidal anti-inflammatory drugs is recommended prior to moving on to corticosteroids.4 Corticosteroids are also considered a treatment mainstay for their immunosuppressive and anti-inflammatory effects.5,6 The vast majority of patients respond well to steroids; however, steroid intolerance and dependence are potential side effects.7 For those who fail steroid therapy, alternatives include radiation or immunosuppressive agents.8 In our case, surgical resection was needed for IOI that was refractory to treatment.
In conclusion, IOI is an orbital inflammatory disease of children and adults, of unknown etiology. It occurs in the absence of known systemic disease. IOI usually responds to steroids, but it may require biopsy followed by other types of immunosuppression in refractory or recurrent cases. REVIEW
1. Fraser CL, Skalicky SE, Gurbaxani A, McCluskey P. Ocular myositis. Curr Allergy Asthma Rep 2013;13:315-21.
2. Schoser BG. Ocular myositis: Diagnostic assessment, differential diagnoses, and therapy of a rare muscle disease—five new cases and review. Clin Ophthalmol 2007;1:37-42.
3. Mombaerts I, Bilyk JR, Rose GE, et al. Consensus on diagnostic criteria of idiopathic orbital inflammation using a modified delphi approach. JAMA Ophthalmol 2017;135:769-776.
4. Mannor GE, Rose GE, Moseley IF, Wright JE. Outcome of orbital myositis. Clinical features associated with recurrence. Ophthalmology 1997;104:409-13; discussion, 414.
5. Espinoza GM. Orbital inflammatory pseudotumors: Etiology, differential diagnosis, and management. Curr Rheumatol Rep 2010;12:443-7.
6. Jacobs D, Galetta S. Diagnosis and management of orbital pseudotumor. Curr Opin Ophthalmol 2002;13:347-51.
7. Yuen SJ, Rubin PA. Idiopathic orbital inflammation: Distribution, clinical features, and treatment outcome. Arch Ophthalmol 2003;121:491-9.
8. Lanciano R, Fowble B, Sergott RC, et al. The results of radiotherapy for orbital pseudotumor. Int J Radiat Oncol Biol Phys 1990;18:407-11.



