Presentation
A 29-year-old Caucasian female with sudden onset of blurred vision and metamorphopsia in her left eye presented for ophthalmic evaluation. She was 20 weeks pregnant at presentation. She denied any history of trauma. She denied any concurrent pain, headache, diplopia, flashes, floaters or photophobia. She denied any symptoms in the right eye. Systemic review of symptoms was negative. Of note, her pregnancy had been uncomplicated up to this point.
History
Past ocular history included myopia in both eyes. Past medical history disclosed celiac disease. Family history included a mother with melanoma of the skin, maternal grandmother with colon cancer, and maternal grandfather with bladder cancer. Social history was significant for rare alcohol consumption, but was otherwise unremarkable. She did not have any known drug allergies. Current medications included pre-natal vitamins.
 |
Examination
The patient’s vital signs were within normal limits. Ocular examination demonstrated best-corrected visual acuity of 20/20 in the right eye and 20/25 in the left eye. Pupils were equally round and reactive in both eyes without afferent pupillary defect in either eye. Intraocular pressures were 10 mmHg in both eyes. Confrontation visual fields were full in both eyes. Extraocular motility was full bilaterally. The anterior segment examination was largely unremarkable and didn’t reveal any abnormalities.
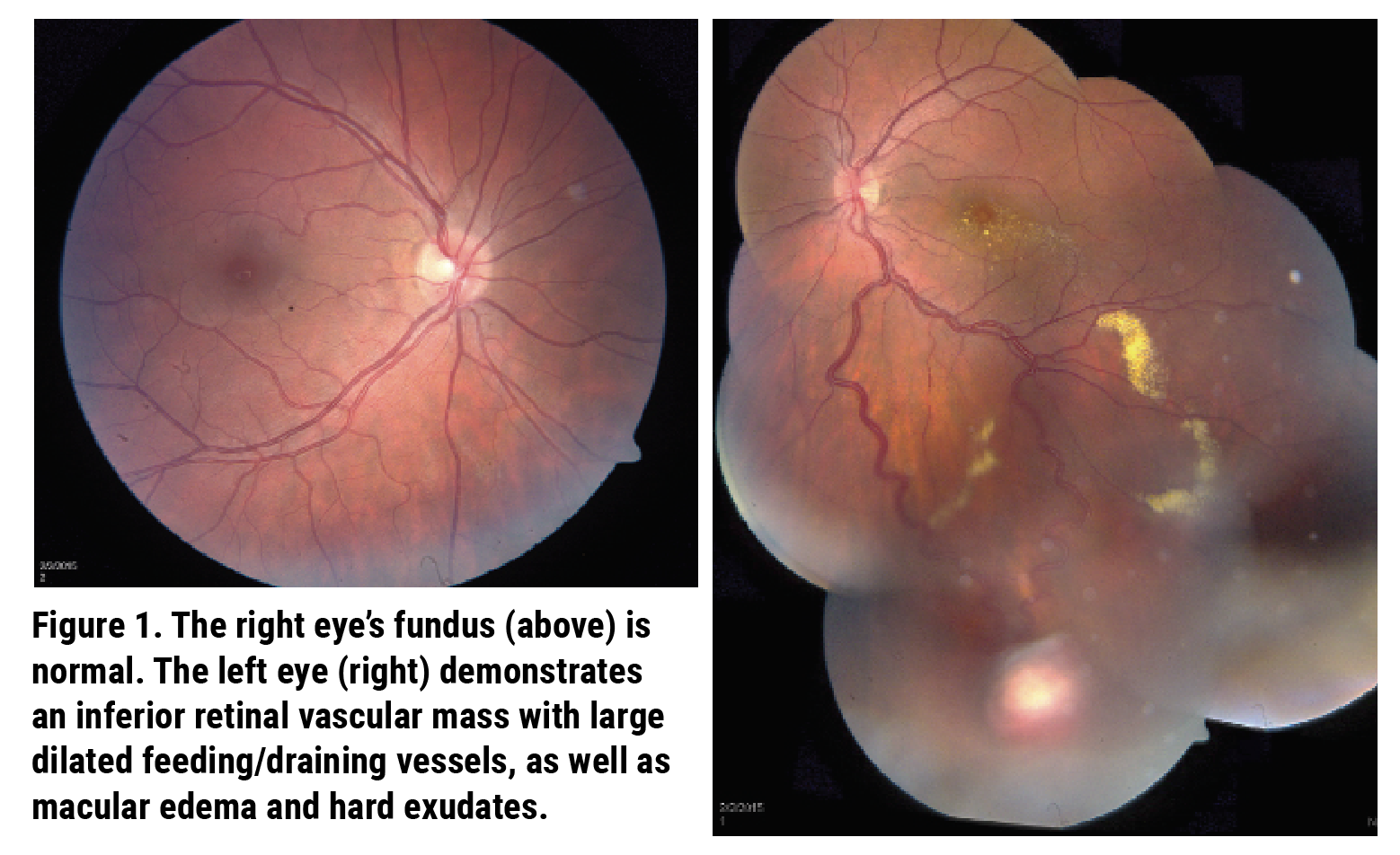
Dilated fundus examination of the right eye demonstrated a normal optic disc, macula, vessels and peripheral retina (Figure 1). The left eye demonstrated a normal optic disc, macular edema with hard exudation, as well as venous dilation and tortuosity inferiorly. Peripheral examination in the left eye revealed a 4x4 mm retinal vascular mass at 5:00 with dilated feeding and draining vessels, as well as additional exudation extending into the periphery (Figure 1).
What’s your diagnosis? What further work-up would you pursue? The diagnosis appears below.
Work-up, Diagnosis and Treatment
Ancillary imaging was obtained including optical coherence tomography (Figure 2) and ophthalmic ultrasonography of the left eye (Figure 3). OCT of the left eye demonstrated macular edema in the outer nuclear layer with associated hard exudation in the outer plexiform layer and shallow subretinal fluid involving the fovea. Ultrasonography revealed an echodense retinal mass with 3.7 mm basal diameter and 1.7 mm retinal thickness.
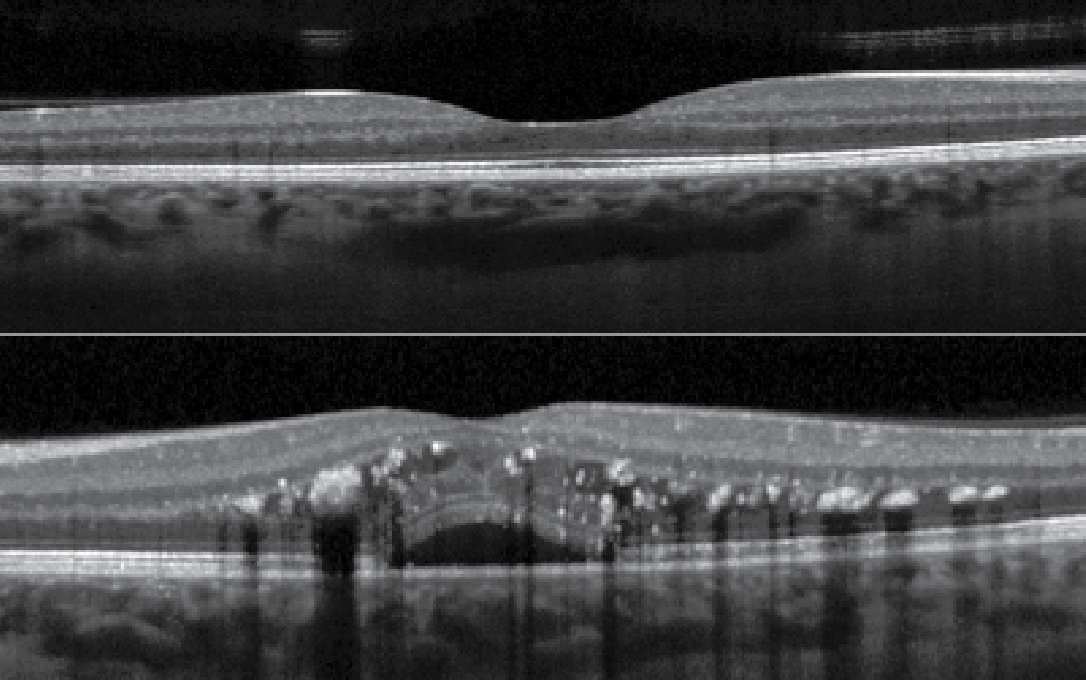 |
| Figure 2. OCT through the macula and optic nerve of the right eye demonstrating normal retinal layers and contour. The left eye demonstrates macular edema in the outer nuclear layer with hard exudates in the outer plexiform layer, and subretinal fluid. |
The differential diagnosis in this patient with unilateral vision loss, found to have a retinal vascular lesion associated with macular edema and hard exudation, includes retinal hemangioblastoma (RH), cavernous hemangioma, acquired vasoproliferative tumor, choroidal hemangioma and retinal racemose hemangiomatosis. Given the dilated and tortuous feeder vessels of the lesion, the presence of associated exudation, and the lack of other ocular conditions, a diagnosis of retinal hemangioblastoma was made. Treatment options, including verteporfin-enhanced photodynamic therapy, fluorescein-enhanced argon laser photocoagulation, transpupillary thermotherapy, cryotherapy and radiotherapy were discussed. The patient chose to defer treatment until the post-partum period. Genetic testing for von Hippel-Lindau (VHL) syndrome was performed and was negative.
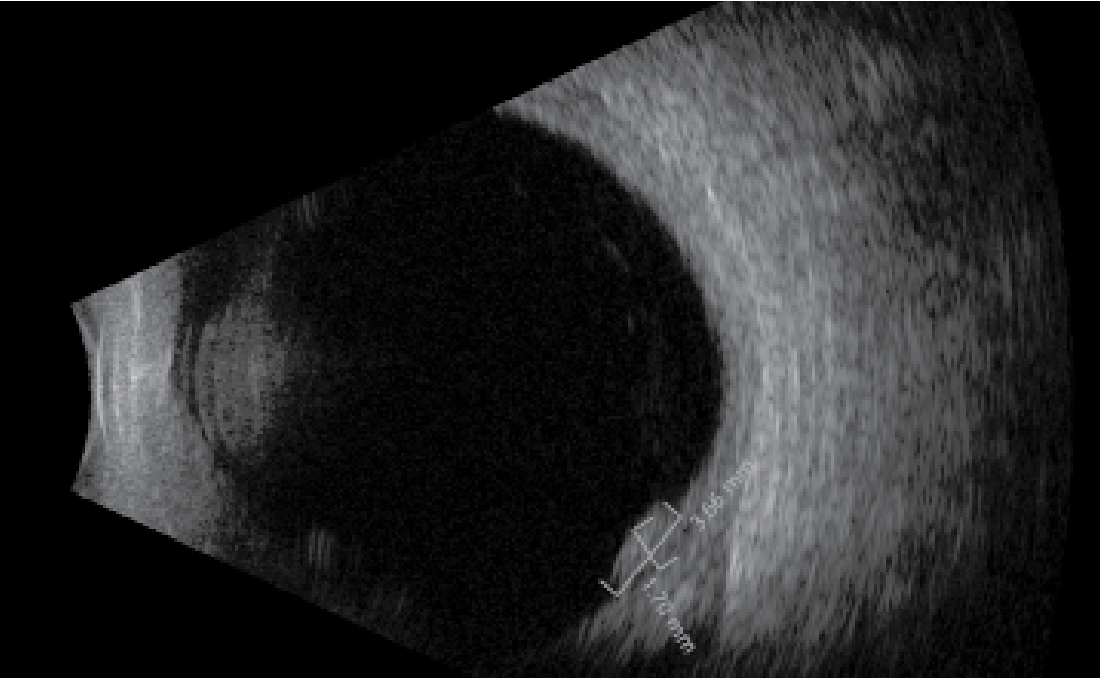 |
| Figure 3. Ultrasonography of the left eye demonstrating an acoustically solid retinal mass measuring 3.7 mm in basal length with 1.7 mm thickness. The retina appears attached. |
At the seven-month follow-up visit, now three months post-partum without any intervention, the patient reported a subjective improvement in her vision. Visual acuity OS improved to 20/20 from 20/25 on initial presentation. Dilated fundus examination revealed a vascular lesion, stable in size, with persistently dilated vessels. OCT demonstrated spontaneous resolution of the macular edema and exudation. The patient continued to defer treatment until cessation of breastfeeding one year from presentation (seven months post-partum). At this time, visual acuity was 20/20 and OCT showed a flat macula without exudation. The RH tumor was unchanged in size. Transpupillary PDT was performed. On postoperative day #1 the patient presented with a visual acuity of 20/400 OS and was found to have severe cystoid macular edema with an exudative retinal detachment (Figure 4). She was treated twice with intravitreal ranibizumab with resulting resolution of the macular edema and retinal detachment. At the most recent follow-up visit, seven years from initial presentation, visual acuity in the left eye was 20/30. Examination and imaging demonstrated a regressed fibrotic retinal lesion measuring 3 mm x 3 mm with nondilated feeder vessels and without the presence of macular edema or exudation (Figure 5).
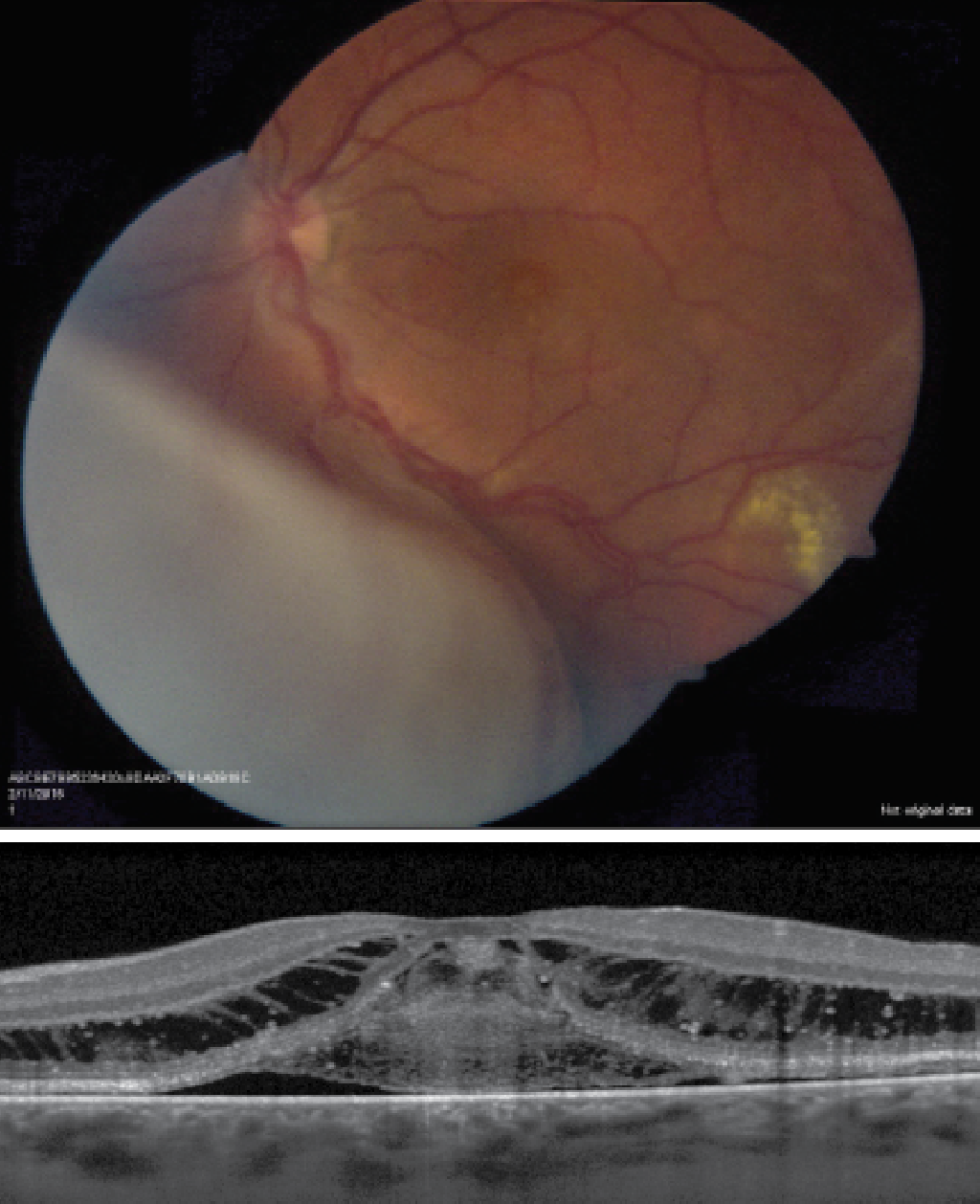 |
| Figure 4. Widefield fundus photo of the left eye demonstrating an exudative retinal detachment in the inferonasal region, as well as dilated vessels and peripheral hard exudation inferiorly. OCT through the macula of the left eye demonstrates cystoid macular edema with subretinal fluid and scattered hard exudation. |
Discussion
Retinal hemangioblastoma is a benign, slow-growing retinal vascular tumor that appears clinically as a red-orange mass.1 This tumor classically presents with prominent feeder vessels extending from the optic disc and can be located in the peripapillary or peripheral retina.1 This tumor can be associated with accumulation of subretinal fluid, sub- and intraretinal exudation, and vitreoretinal fibrosis, which can result in profound visual loss.1 The exudation often accumulates in the macula and presents as a macular star.2 Diagnosis can typically be made on dilated fundoscopic examination, though additional imaging is helpful, particularly in the cases of small tumors. In some cases, this tumor can be detected on fluorescein angiography as hyperfluorescent, before it becomes symptomatic.2 Biopsy isn’t required for diagnosis.
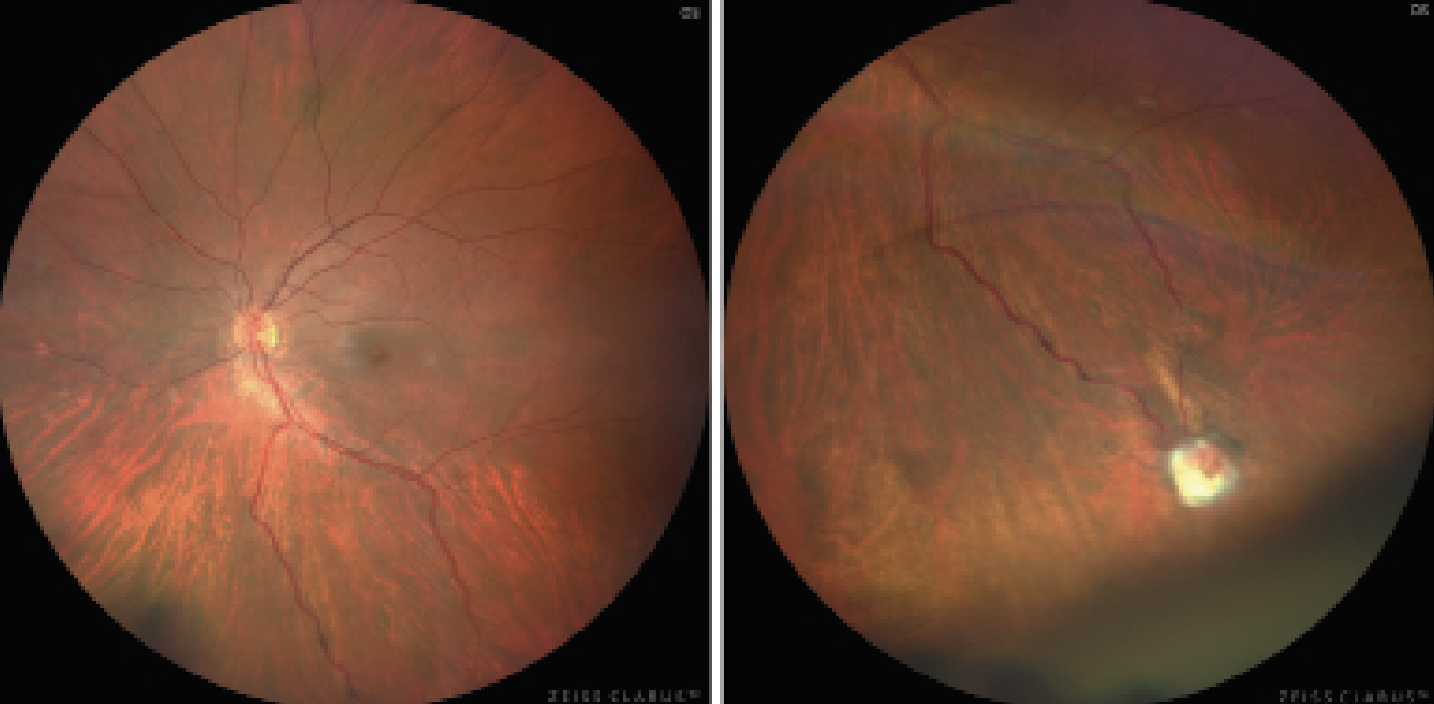 |
| Figure 5. Fundus photographs of the left eye demonstrate normal macula (left) and treated, fibrotic retinal hemangioblastoma in the inferior periphery (right). The feeder vessels demonstrate reduced dilation. |
Clinical onset occurs most commonly in the first three decades of life.1,2 Importantly, retinal hemangioblastoma can be associated with VHL syndrome, and a thorough workup is required for any case of suspected hemangioblastoma. VHL syndrome is an autosomal dominant disorder caused by a mutation in the VHL tumor suppressor gene, located on chromosome 3.3,4 This mutation has a prevalence of 1 in 40,000 to 50,000.4 Detection of these tumors by an ophthalmologist is critical, as 70 percent of individuals with VHL syndrome are diagnosed by detection of RH tumors.5 This prompts a full systemic workup for other tumors, including renal cell carcinoma, which constitutes the greatest cause of mortality in these patients.2
Treatment for RH is varied and depends on the size and location of the tumor, as well as the VHL association. Some believe that this tumor can be safely observed in select cases when asymptomatic without subretinal fluid.2,3,6 However, most are treated and those with VHL association tend to be more aggressive.2,6 Those near the macula can lead to profound vision loss, and thus also require prompt treatment. Treatment methods vary based on tumor size. Small lesions (<3 mm) can be treated with laser photocoagulation or PDT; medium lesions (3 to 6 mm) can be treated with PDT or cryotherapy; and large (>6 mm) lesions can be treated with PDT, plaque radiotherapy or internal resection by pars plana vitrectomy.6 Therapy with PDT can be associated with a transient exudative response, as was noted in 24 percent of patients in a recent case series of 17 patients.7,8 Anti-vascular endothelial growth factor (VEGF) therapy is useful in reducing macular edema and subretinal fluid, but has no demonstrated effect in reducing tumor size.3,8
This case was unique in that our patient initially presented with an RH tumor during pregnancy; similar cases aren’t well-documented in the literature. She demonstrated a spontaneous resolution of secondary macular edema post-partum, as has been seen in cases of macular edema associated with other underlying conditions such as diabetic retinopathy and circumscribed choroidal hemangioma.9 The tumor remained stable in size; however, treatment was deemed necessary due to the threat of recurrence of subretinal fluid.
In conclusion, retinal hemangioblastoma can present with decreased visual acuity, commonly secondary to macular edema with exudation, as was the case with our patient. For those tumors diagnosed in pregnancy, spontaneous resolution of subretinal fluid may occur in the postpartum period. Treatment modalities vary based on size, location and association with VHL syndrome. Management with PDT, which is used to treat tumors of all sizes, can cause a transient exudative response. Anti-VEGF therapy can be useful in treating associated macular edema and subretinal fluid.
1. Singh A, Turell M. Vascular tumors of the retina and choroid: Diagnosis and treatment. Middle East African Journal of Ophthalmology 2010;17:3:191. doi:https://doi.org/10.4103/0974-9233.65486.
2. Singh AD, Shields CL, Shields JA. von Hippel-Lindau disease. Surv Ophthalmol 2001;46:117-42.
3. Wiley HE, Krivosic V, Gaudric A, et al. Management of retinal hemangioblastoma in von Hippel–Lindau disease. Retina 2019;39;12:2254-2263. doi:https://doi.org/10.1097/iae.0000000000002572.
4. Maher ER, Neumann HP, Richard S. von Hippel–Lindau disease: A clinical and scientific review. European Journal of Human Genetics 2011;19:6:617-623. doi:https://doi.org/10.1038/ejhg.2010.175.
5. Şahin Atik S, Solmaz AE, Öztaş Z, et al. Von Hippel-Lindau Disease: The importance of retinal hemangioblastomas in diagnosis. Türk Oftalmoloji Dergisi 2017;47:3:180-183. doi:https://doi.org/10.4274/tjo.90912.
6. Singh AD, Nouri M, Shields CL, Shields JA, Perez N. Treatment of retinal capillary hemangioma. Ophthalmology 2002;109:10:1799-1806. doi:https://doi.org/10.1016/s0161-6420(02)01177-6.
7. Di Nicola M, Williams BK, Hua J, et al. Photodynamic therapy for retinal hemangioblastoma: Treatment outcomes of 17 consecutive patients. Ophthalmology Retina 2022;6:1:80-88. doi:https://doi.org/10.1016/j.oret.2021.04.007.
8. Borgia F, Giuffrida R, Caradonna E, Vaccaro M, Guarneri F, Cannavò SP. Early and late onset side effects of photodynamic therapy. Biomedicines 2018;6:1. doi:https://doi.org/10.3390/biomedicines6010012.
9. Muslubas IS, Arf S, Hocaoglu M, Ozdemir H, Karacorlu M. Spontaneous regression of serous retinal detachment associated with circumscribed choroidal hemangioma after childbirth. Published online January 1, 2017. doi:https://doi.org/10.1097/icb.0000000000000274.



