The COVID-19 pandemic is a double whammy for many ophthalmic products. Pandemic-based limits on “non-critical” visits and procedures have virtually eliminated the use of many cataract-surgery-related products. At the same time, the economic consequences of the pandemic could be devastating, making the more costly, optional offerings a hard sell after the crisis ends.
One group of items that could arguably be in trouble in this situation is premium intraocular lenses. Here, surgeons discuss the reasons lenses in this category may or may not be big sellers after this resolves; describe some new advanced-technology options that may rise to the top in an economically challenged future; and recap some basic guidelines for successfully offering these options under any circumstances.
The Effects of a Crisis
Samuel Lee, MD, a cornea and cataract surgeon at Sacramento Eye Consultants in California and a member of the clinical faculty at University of California Davis, believes the current crisis is likely to negatively impact the popularity of premium options. “People will have less disposable income,” he points out. “Patients who might have budgeted $2,000 to $3,000 per eye for a premium lens upgrade may either reconsider and save that money for a rainy day or just cut their expenses because they lost money in the stock market or lost their job. Typically, the medical profession is fairly immune to recessions, but the first things to go are cosmetic and elective procedures.”
On the other hand, some factors could actually result in increased interest in these options after the crisis:
• More people could end up wanting freedom from glasses and contact lenses. “The current crisis has generated a lot of fear of not having independence and freedom,” notes Norfolk, Virginia’s Elizabeth Yeu-Lin, MD, an assistant professor in the Department of Ophthalmology at Eastern Virginia Medical School and medical director of the Virginia Surgery Center. “I think that will really hit home in the next few months while we’re restricted and stuck indoors, especially for individuals who rely heavily on glasses or contact lenses. As long as the economy is able to rebound after the crisis abates, that could lead to an uptick in LASIK and premium lenses.”
• A pause in service availability leads to pent-up demand. Mark Packer, MD, president of Packer Research Associates in Boulder, Colorado, sees reason to believe that rather than disappearing, demand for premium options may simply be in a holding pattern during the pandemic. “If you think about the rate at which cataract surgery is normally done, and the fact that it’s at zero right now, there will be a lot of demand for it once the crisis is over,” he says. “Meanwhile, the same number of people will still want to have freedom from glasses.
“I’m paying close attention to what’s going on in China,” he continues. “The largest hospital chain in the world is a Chinese group called Aier Hospitals. They closed down for about six weeks after the pandemic started, but then they gradually reopened. They’re now doing a higher volume of all types of eye surgery than ever before, which appears to be about managing pent-up demand. Of course, they’re using extreme personal protection protocols to minimize the risk of disease trans-mission while treating large numbers of patients, and I’m not sure if it would be possible to implement some of those protocols over here. People in the United States are more resistant to following orders from a doctor or the government. But I see their success as a hopeful sign. They’re up and running, the demand is higher than ever, and they’ve been able to adapt to minimize the danger.”
• Payment options could proliferate after the crisis abates. “How the economy will fare is hard to predict, but I think there will be a variety of mechanisms to help patients go ahead with those choices—people willing to make loans, and so forth,” says Dr. Packer. “In a recovery period there are always people who are betting that something will work out in the long run, and to them it might be a perfect time to loan people money.”
• The lenses are better than ever. “The latest generation of lenses has brought incremental but significant improvements that produce excellent vision and allow patients greater freedom than ever,” notes Dr. Yeu. “The current trifocals are especially remarkable. We know from international data, supported by my own experience as an investigator in the FDA study, that trifocal lenses provide a high quality level of vision at multiple ranges. That translates to greater freedom for our patients.”
She also points out that the range of issues such as astigmatism that can be corrected keeps expanding. “Previously, we could only correct total corneal astigmatism of 1 D or more with monofocal toric lenses,” she says. “Now, thanks to Bausch + Lomb’s enVista lens, we can correct down to 0.8 D of corneal astigmatism. This is particularly fantastic for with-the-rule astigmatism patients, who generally possess less total WTR corneal astigmatism than what’s observed in the anterior cornea.”
Dr. Yeu adds that dysphotopsias are much less of an issue with the current lenses. “It’s always a tradeoff between benefits and side effects,” she notes. “Today, the overwhelming majority of patients are so pleased with the benefits afforded by the trifocal lenses and other current options that the mild to moderate amount of glare and halo they experience is seen as well worth the tradeoff. For example, the FDA trifocal study found that more than 99 percent of patients would have the same lens implanted again.”
• Toric IOLs arguably can save patients money over the long run. “Studies have shown that a toric lens pays for itself pretty quickly over time because you don’t need to purchase glasses to correct astigmatism,” Dr. Packer points out. “That means there’s a cost-effectiveness argument to be made for toric lenses.
“Unfortunately,” he adds, “we can’t make that same argument for presbyopia-correcting lenses, because reading glasses are cheap.”
New Options on the Horizon
 |
Often, new products emerge during a crisis that meet people’s needs better than previous options. Dr. Packer notes that a recently developed new IOL design, referred to as enhanced monofocals, could end up becoming a major player in the marketplace, particularly if there’s an economic crunch. (None have been approved in the United States to date.)
“These lenses simply increase the asphericity of a monofocal lens to provide more depth of focus,” he explains. “Doing this gives you an additional line of visual acuity at intermediate range, so if you’re 20/20 at distance, you’d be around 20/25 or 20/30 at arm’s length. This is a big deal because so many people use screens now, and screens are usually held at about arm’s length. With the enhanced monofocal lens you won’t need a pair of glasses to use your laptop or phone.
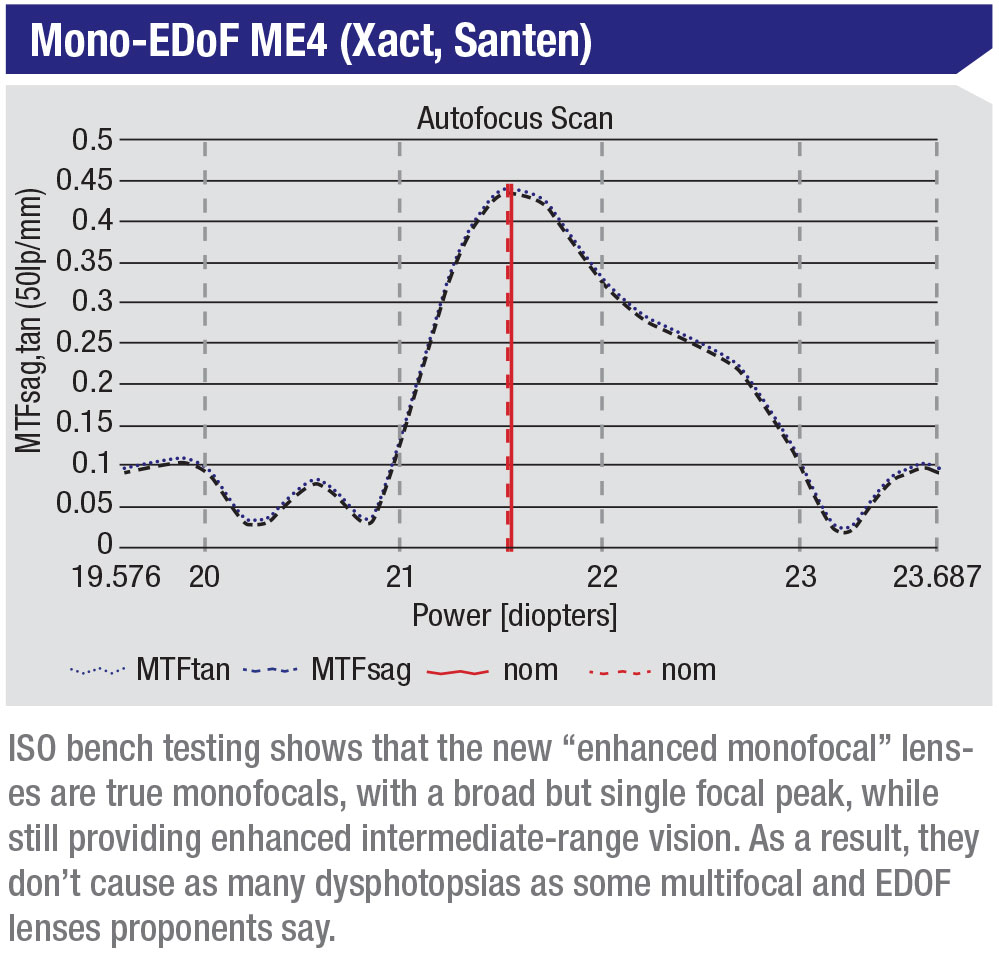
“This technology has several other important benefits,” he continues. “First of all, because it’s a monofocal, it doesn’t cause the dysphotopsias associated with multifocal lenses and extended depth-of-focus lenses. These lenses have a single through-focus modulation transfer function peak in ISO bench testing, so they really are monofocals. On the MTF graph they just have an extended single peak, meaning they give you increased intermediate vision. (See graph, below.) In contrast, the MTF graph for the Symfony lens has two peaks, so it’s not classified as a monofocal.
“Patients with enhanced monofocals don’t get halo or glare the way they might with a traditional diffractive or multifocal or EDOF lens,” he continues. “I saw this first-hand when I was involved with the clinical trials of Santen’s value-added monofocal in Europe. Among other things, we compared the dysphotopsias seen by these patients to dysphotopsias seen with other lenses. The Santen lens results were closer to a monofocal than to an EDOF or multifocal lens.
 |
“A second important benefit is that ophthalmologists in Europe are adding just a small surcharge for this benefit,” he continues. “They may add 100 or 200 Euros to the cost of a standard monofocal, instead of asking patients to pay thousands more for other advanced-technology lenses. These lenses don’t cost any more to produce; any additional cost was in the research and development and any clinical trials, which are all one-time costs.
“Of course,” he adds, “the profit margin isn’t anything close to current premium lenses, but if you can do enough in volume, that extra 100 or 200 Euros starts to add up. That means patients get some of the advantages of the more expensive lenses at a very affordable cost. Plus, you don’t have to deal with the much higher level of patient expectation that comes with higher cost.” (To learn more about these lenses, see “Dawn of the Monofocal Plus Era” on page 12.)
If You’re Just Starting Out
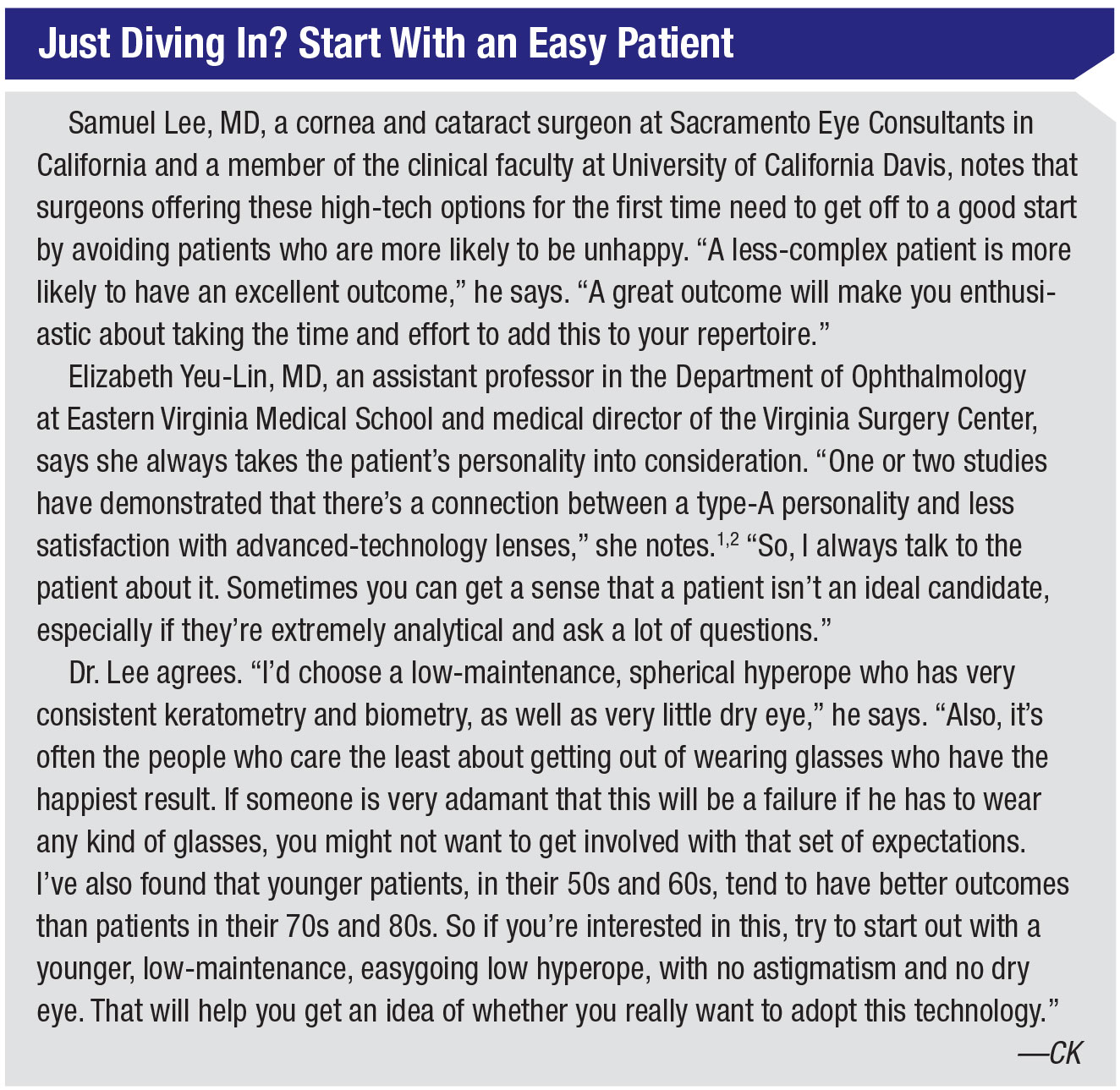
If you still haven’t taken the plunge into offering advanced-technology lenses, and plan to start once the crisis has passed, some preparation is essential. “If you just start offering multifocals without any preparation, that’s not a recipe for success,” notes Dr. Lee.
Surgeons offer these tips:
• Don’t offer these options unless you believe in them. Dr. Lee notes that most patients take their cue from the surgeon. “Sometimes patients will come in knowing what they want, but typically, patients will follow the surgeon’s recommendation,” he notes. “If the surgeon is hesitant about it, patients are less likely to go for it. If the surgeon is confident about the technology, patients will be much more receptive.”
• Lower the cost of admission for your first couple of patients. “If you’re just getting started with these implants, try to defer the surgeon fee for the refractive portion of the procedure,” Dr. Lee suggests. “If you just tack on the cost of the lens implant, the patient is spending maybe $900 per eye; that’s not a super high cost. Do that for one or two patients to get a feel for it. If you’re charging $3,000 or $5,000 an eye on your first patient, and you choose the wrong patient and he ends up unhappy, it will leave a bad taste in your mouth.”
• Ask about the patient’s goals. “Typically, when patients come in for a cataract consultation, we’ll have them watch a video and take a survey at home,” says Dr. Lee. “That gives us an idea about their goals in terms of spectacle independence, and it tells us whether they have any interest in a refractive correction during the cataract procedure.”
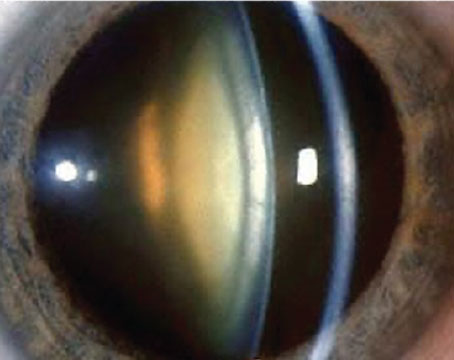
• Be careful about co-morbidities. “I won’t place a light-splitting presbyopia-correcting lens—multifocal or EDOF—in a patient with any retinal problem that crosses the fovea, whether it’s a subretinal elevation such as a foveal drusen or an epiretinal membrane,” says Dr. Yeu. “If the eye has a peripheral, stable ERM, I might consider implanting an advanced-technology lens, but not if the ERM crosses the fovea.
“Ultimately,” she says, “we should always offer correction of corneal astigmatism with a monofocal option such as a toric lens implant, or femtosecond-laser astigmatic keratotomy, to patients with decent visual potential.”
• Make sure you’re getting accurate information from your measuring devices. “Learn to evaluate the keratometric values on placido topography and optical biometry to determine the quality of the images and the actual amount of astigmatism that needs to be corrected,” advises Dr. Yeu. “That includes knowing how to distinguish between real astigmatism and astigmatism caused by a pathology such as dry-eye disease or anterior basement membrane dystrophy.”
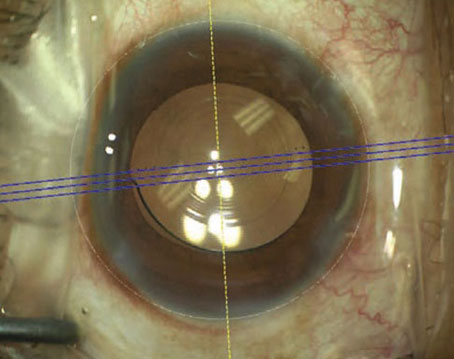
• Familiarize yourself with surgical techniques related to implant-
ing these options. “Familiarize yourself with implanting and orienting toric lenses, and centering presbyopia-correcting lenses,” says Dr. Yeu.
• Learn how to take care of the occasional unhappy patient. “There’s a systematic process for deciphering whether a problem is the result of dry eye, refractive error or the lens itself,” notes Dr. Yeu. “For example, if you’ve implanted a toric lens, it may simply need to be rotated. Of course, you have to be able to make whatever correction is necessary, or have a partner in the community who’s willing to help you in that situation, such as another surgeon who’s able to do laser vision enhancement as needed.”
• Pay extra attention to dry eye, both before surgery and after. “I occasionally see patients coming in for a second opinion who are unhappy with their late-model presbyopia-correcting IOL,” says Dr. Lee. “It often comes down to one foundational problem: dry eye. If there’s a little dry eye present but you don’t notice it during your initial preop testing, you may not get accurate measurements. The patient can end up with residual astigmatism and be walking around unhappy.”
 |
Looking to the Future
“It’s always hard to be offering what could be considered luxury items in a time of contraction,” Dr. Packer admits. “Everyone wants to get down to basic needs. But there are still reasons to think outside of that box. We won’t always be working in these circumstances. Remember that decisions you make now will have an impact five or 10 years from now.”
Dr. Yeu says it’s very important that surgeon education continues to expand so surgeons can move toward offering these high-tech options. “Surgeons just took a 15-percent hit on reimbursements for all routine cataract surgery procedures this year,” she points out. “That’s just the beginning. Reimbursements are going to continue to decline, which is reason enough to look for ways we can supplement our reimbursements. In addition, more and more patients today are coming in to the clinic desiring complete independence and freedom from glasses and contact lenses. And, as noted earlier, a crisis like the one we’re going through could actually increase the number of patients who desire that level of independence and spectacle freedom.” REVIEW
Dr. Yeu consults for Alcon, Johnson & Johnson Vision, Zeiss, Lensar and Bausch + Lomb. Dr. Packer is a consultant for Santen and Alcon. Dr. Lee reports no financial ties to any product discussed.
1. Henderson B, Sharif Z, Geneva I. Presbyopia Correcting IOLs: Patient Selection and Satisfaction. In: Bradley Randleman, Iqbal Ike K. Ahmed, eds. Intraocular Lens Surgery: Selection, Complications, and Complex Cases. Thieme Medical; 2015:72-77.
2. Rudalevicius P, Lekaviciene R, Auffarth GU, et al. Relations between patient personality and patients’ dissatisfaction after multifocal intraocular lens implantation: Clinical study based on the five factor inventory personality evaluation. Eye (Lond) 2020;34:4:717-724.
3. Packer M. Clinical comparison and patient satisfaction with novel extended-depth-of-focus intraocular lens satisfying ISO 11979-2 optical standards for monofocal intraocular lenses. (Presenting Author). European Society of Cataract and Refractive Surgeons, Vienna, Austria, 22 September 2018.