Presentation
A 36-year-old female presented with two weeks of right upper eyelid swelling fluctuating in severity. She endorsed mild itching, tearing and injection, but denied decreased vision, diplopia or pain with extraocular movements. She had no fevers, chills or headaches. These symptoms began several days after returning from a trip to Costa Rica, during which she swam in fresh water and hiked in a muddy swamp. She reported wearing mosquito repellent, sleeping with a mosquito net for the entirety of the trip, and having no known insect bites or direct contact with wild animals. On the trip, she developed two ‘pimple-like lesions’ on her right temple and medial lower eyelid associated with mild itching that had since resolved.
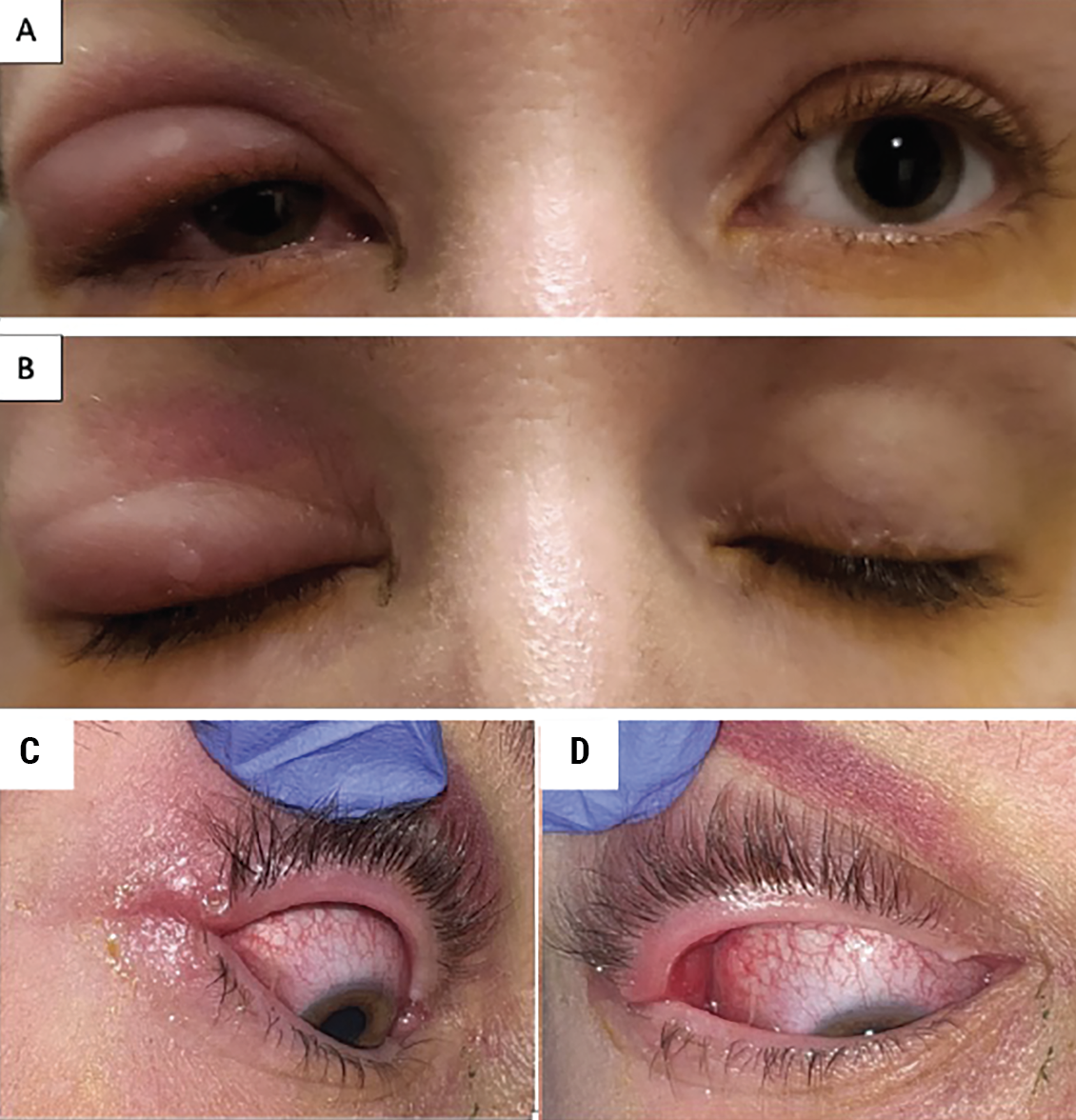 |
| Figure 1. (A, B) External exam demonstrating right upper lid edema and preseptal cellulitis. (C) Higher magnification demonstrating a 1 to 2 mm opening on the lash line that produced serosanguinous discharge on expression. (D) Fullness of the lateral right upper eyelid is visible from the palpebral conjunctiva. |
History
Her past medical history is notable for oral herpes simplex virus. Her past ocular history is positive for contact lens wear, false-eyelash use and occasional chalazia. She lives at home with her child, one male partner and two dogs. She gardens outdoors frequently and lives and works indoors in a major Northeast metropolitan area.
She had been using warm compresses and tobramycin-dexamethasone ophthalmic ointment for a presumed chalazion without much improvement and was later prescribed cefalexin by her primary care provider for preseptal cellulitis, which she had self-discontinued after three days due to worsening symptoms. She had also tried a course of trimethoprim-sulfamethoxazole and oral prednisone as well as valacyclovir given to her by a local urgent care. Despite these treatments, the eyelid swelling continued to progress and she began noticing spontaneous bleeding from the lesion which prompted her to seek care at the Wills Eye Emergency Room.
Examination
At this presentation, her vitals were within normal limits and she was afebrile. She had 20/20 vision in each eye, normal intraocular pressures and full extraocular movements. Her external exam was notable for a large, firm, non-tender pre-auricular node on the right as well as moderate right upper eyelid swelling (Figures 1A, 1B). On closer examination she had a small nodule on the right upper eyelid with a 1- to 2-mm opening on the lash line that produced serosanguinous discharge on expression (Figure 1C). The remainder of the slit lamp and dilated exam in both eyes was normal.
What’s your diagnosis? What further work-up would you pursue? The diagnosis appears below.
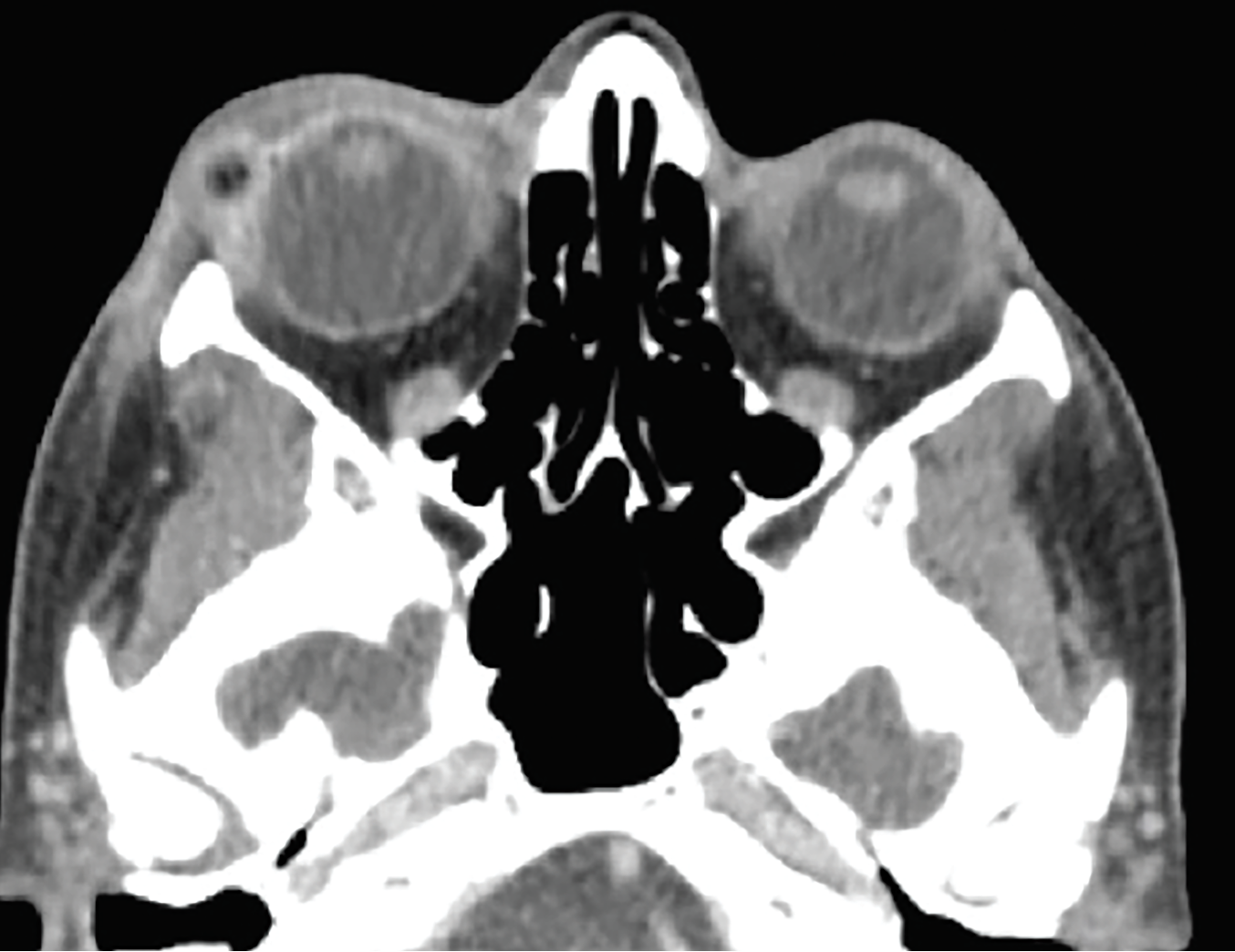 |
| Figure 2. CT orbits with contrast (axial view), showing right-sided preseptal soft-tissue swelling with a 0.6 x 0.8 cm fluid collection with foci of gas in the lateral superior eyelid, without post-septal involvement. |
Work-up, Diagnosis and Treatment
Given the lack of improvement with several antibiotics and antivirals and her recent tropical exposure, parasitic and less commonly encountered fungal and bacterial pathogens were considered. The serosanguinous drainage was sent for culture, and peripheral blood testing for several of the above infections was obtained with the help of infectious disease specialists (ultimately yielding no causative microorganism). She was discharged on doxycycline and tobramycin-dexamethasone ophthalmic ointment with close follow-up.
Over the following days the patient noticed worsening right upper lid swelling and returned to the ER. Her exam was similar to prior. She continued to have fullness of the lateral right upper eyelid, which was now visible from the palpebral conjunctiva on lid eversion (Figure 1D). Computed tomography imaging of the orbits with contrast showed right preseptal soft tissue swelling with a small fluid/gas collection (Figure 2).
 |
|
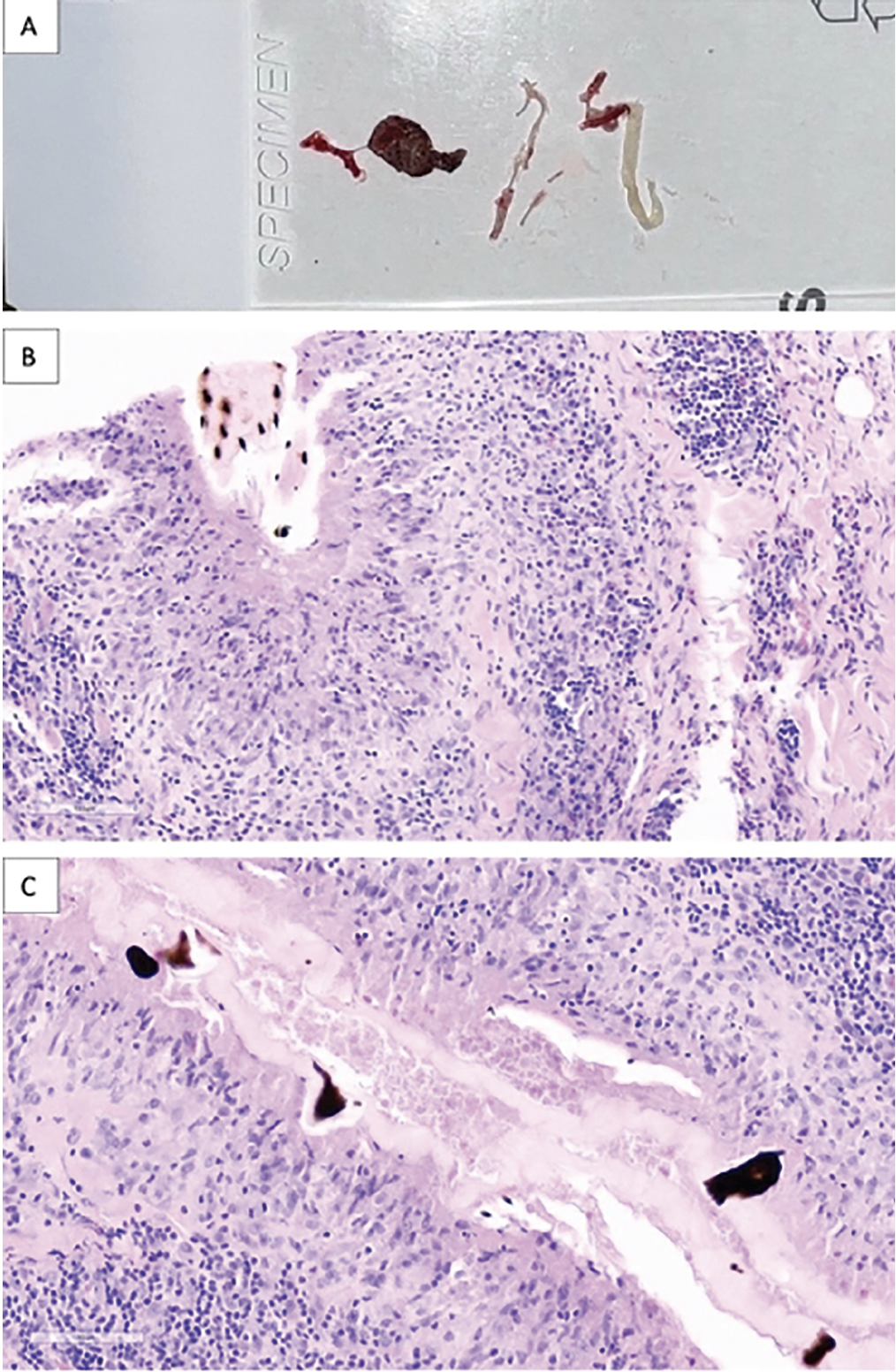
Figure 3. (A) Contents of incision and drainage: A 0.5-cm foreign body with black spines consistent with the appearance of botfly larvae. (B) Histopathology showing a prominent palisading zonal granuloma comprising epithelioid histocytes containing fragments of material consistent with the wall of a botfly. (C) Higher magnification of the characteristic intensely pigmented spiny processes. |
Decision was made for transconjunctival incision and drainage of the lesion. A white, string-like material was expressed first, followed by a 0.5-cm foreign body with black spines, consistent with the appearance of botfly larva (Figure 3A). The specimens were sent to pathology which eventually confirmed the diagnosis of botfly fragments with surrounding granulomatous inflammation (Figures 3B, 3C). Clindamycin and dexamethasone were injected into the lesion and the patient was continued on her course of doxycycline and ointment and started on oral methylprednisolone with taper. At one week, the lid swelling and other symptoms had improved significantly (Figure 4A); she was found to have an additional raised nodule below the medial canthus. Further incision and drainage was performed of the nodule which revealed two cystic lesions, confirmed as additional larvae fragments on pathology (Figure 4B).
Discussion
Infestation with the human botfly (Dermatobia hominis) is an uncommon cause of skin swelling.
Ophthalmomyiasis externa is human botfly larvae infestation of the external eye which is a rare cause of eyelid swelling. The human botfly is endemic to Central and South America,1 however North American botfly myiasis has also been reported with the Cuterebra, or North American botfly, larvae.2,3 The botfly lays up to 24 eggs on a carrier (usually a mosquito) which can then be transferred to humans via mosquito bite.1,4 Once transferred to the human skin, the abrupt change in temperature causes the eggs to hatch. The larvae bury deeper into the skin causing an inflammatory reaction that produces encapsulation and helps the larvae evade the human immune system.1,4 The host’s inflammatory response may produce intermittent swelling and bleeding from the lesion, as was seen in our patient.4 After four to 10 weeks, the mature larvae are expelled from the skin and drop into the soil where they pupate over several days, developing antennae and wings, and exit the soil to complete their life cycle.1,4,5
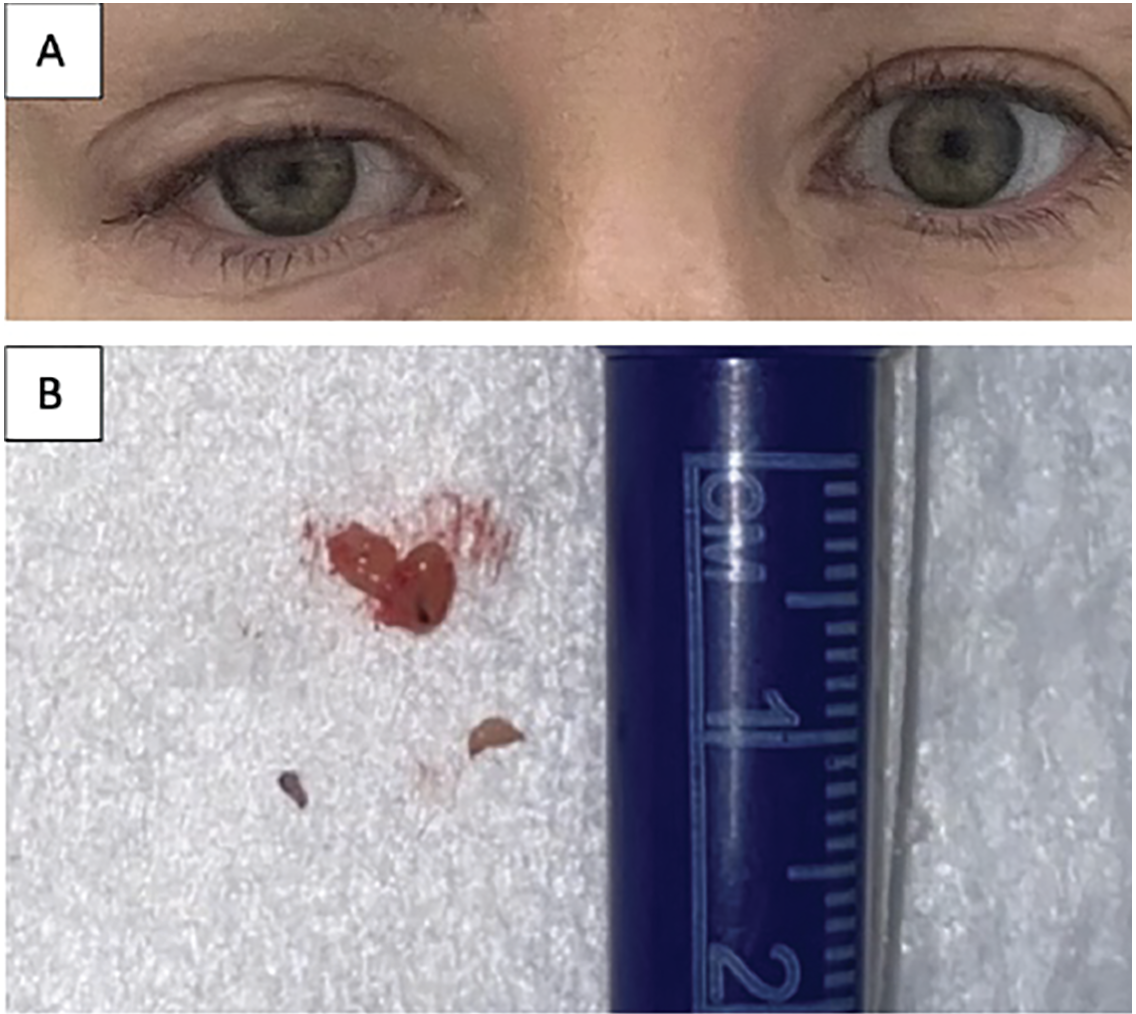 |
| Figure 4. (A) Improvement in upper lid swelling one week after incision and drainage. (B) Incision and drainage of medial canthal nodule revealing two additional cystic lesions with botfly fragments at one week follow-up. |
Patients infected with botfly larvae will often describe a slow growing nodule which may be confused with a chalazion or preseptal cellulitis.1,4 On close examination the nodule is usually found to have a small opening or central pore consistent with the breathing hole, which produces serosanguinous expression when palpated, as was seen in this case.4 This breathing hole is required for the larvae to stay alive under the skin and if blocked can cause botfly death and worsening focal inflammatory reaction.4 Patients often have no other systemic symptoms, but peripheral blood may show leukocytosis with eosinophilia.1,4 Treatment may be achieved non-surgically with suffocation by obstructing the breathing hole with ointment, injecting lidocaine, or by manual extraction with incision and drainage.1,4,6 Oral anti-helminthics such as ivermectin have been reported to be useful in severe cases or when surgical extraction is not possible.1,7,8 Expectant management is also plausible as the larvae eventually expel themselves, as mentioned above.4
Although the skin is the most common location for botfly infestation, they can also be found inside the globe.9,10 In ophthalmomyiasis interna, the larvae enter the posterior segment. Most commonly they burrow under the retina, where they can be seen on dilated fundus exam. They leave characteristic appearing ‘tracks’ when they move within the subretinal space, and rarely can even be found within the vitreous cavity. The treatment options include observation if the larva is dead or near the fovea, laser photocoagulation if outside the macula, or vitrectomy (with or without administration of intraocular steroids) if the larva is within the vitreous cavity.9 In cases of ophthalmomyiasis interna treated with laser, careful follow up is required as death of the larvae can lead to a rampant intraocular inflammatory response.10 Ophthalmomyiasis interna is often diagnosed late in the disease course with resultant significant visual morbidity.9
Although rare, Dermatobia hominis infestation should be considered in a patient with skin lesions not responding to conventional treatment, especially in patients who have had recent travel to endemic areas. Infestation with the Cuterebra species may be seen more frequently in North America, particular in the Northeast or Pacific Northwest in the summer months, and may present similarly.2,3
1. Ragi SD, Kapila R, Schwartz RA. The botfly, a tropical menace: A distinctive myiasis caused by Dermatobia hominis. Am J Clin Dermatol 2021;22, 81–88.
2. Baird JK, Baird CR, Sabrosky CW. North American cuterebrid myiasis. Report of seventeen new infections of human beings and review of the disease. J Am Acad Dermatol 1989;21(4 Pt 1):763–772.
3. Ahmet AH, Krafchik BR. The unidentified parasite: A probable case of North American cuterebrid myiasis in a pediatric patient. Pediatr Dermatol 2004;21:515–516.
4. Mattison N, Cooper JS. Botfly. StatPearls [online]. January 2022. Available at: https://www.ncbi.nlm.nih.gov/books/NBK559223/. Accessed September 6, 2022.
5. Starks V, Durand M, Ryan E, et al. Human bot fly infestation of the eyelid. Ophthal Plast Reconstr Surg 2018;34:1:e36.
6. Sucilathangam G, Meenakshisundaram A, Hariramasubramanian S, et al. External ophthalmomyiasis which was caused by sheep botfly (Oestrus ovis) larva: A report of 10 cases. J Clin Diagn Re 2013;7:3:539-42.
7. Wakamatsu TH, Pierre-Filho P. Ophthalmomyiasis externa caused by Dermatobia hominis: A successful treatment with oral ivermectin. Eye 2006;20:1088–1090.
8. Kaeley N, Kaushik RM, Rajput R, et al. Orbital myiasis with scalp pediculosis and buccal abscess–An uncommon presentation. J Clin of Diagn Res 2017;11:2:OD01-OD02.
9. Punjabi OS, Browning DJ, Clark L, et al. “Pacman” invasion of the retina: Two cases of ophthalmomyiasis interna posterior. Am J Ophthalmol Case Rep 2019;15:100491.
10. Buettner H. Ophthalmomyiasis Interna. Arch Ophthalmol 2002;120:11:1598–1599.



